22 Oberlin Transfer
Abstract
Restoration of elbow flexion is pivotal to improve function in patients with brachial plexus injuries. The Oberlin transfer was described in 1994 and involves transferring one or more motor fascicles of the ulnar nerve to the biceps branch of the musculocutaneous nerve. It has gained popularity as a more simple and reliable transfer than previously described procedures. Modifications to the Oberlin transfer has been proposed, such as the double fascicular transfer, but no procedure has proven to give better results than the Oberlin transfer.
22.1 Description
In 1994, Cristophe Oberlin et al described a nerve transfer using part of the ulnar nerve to the musculocutaneous branch of the biceps muscle in order to restore elbow flexion in C5–C6 nerve root avulsions. 1
22.2 Key Principles
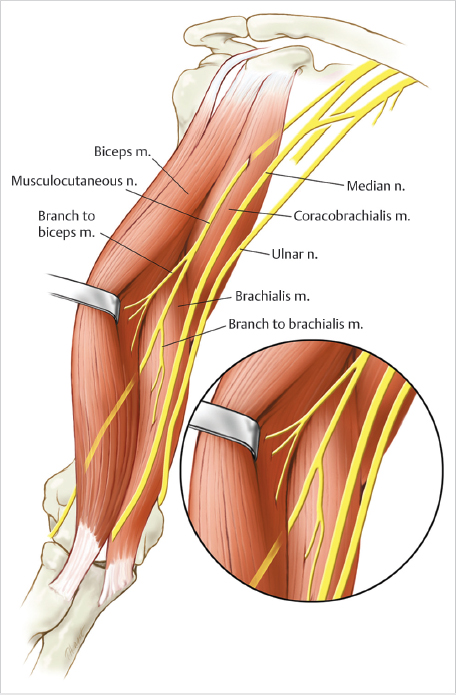
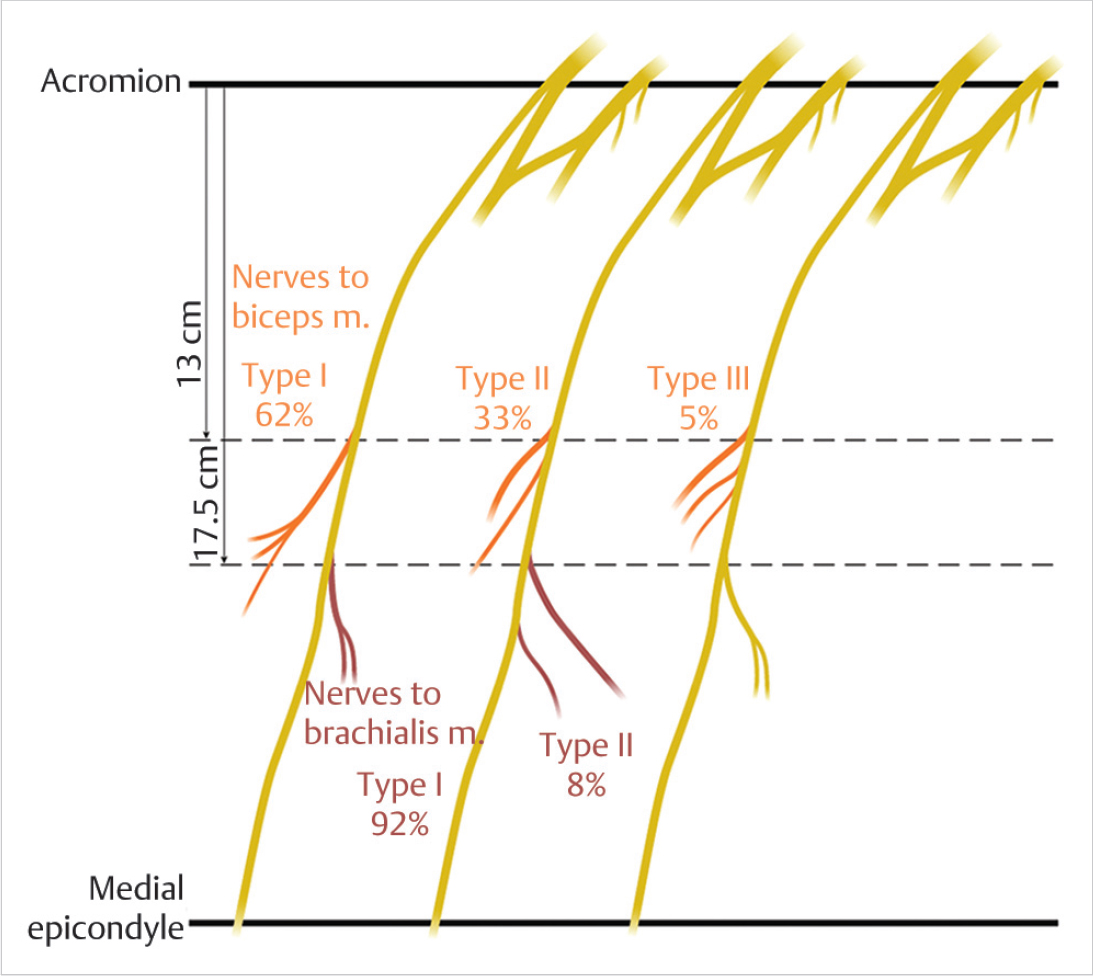
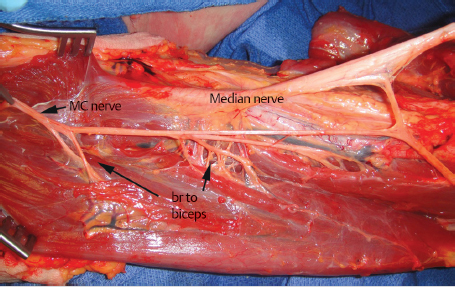
Restoration of elbow flexion is the primary goal in the treatment of upper brachial plexus injuries (► Fig. 22.1). The Oberlin transfer is particularly successful because the ulnar nerve is usually not affected by upper brachial plexus injuries, and the ulnar nerve is in close proximity to the target musculocutaneous nerve branch of the biceps, allowing for direct repair and relatively quick reinnervation of the biceps muscle (► Fig. 22.2 and ► Fig. 22.3).
22.3 Expectations
After this procedure, nearly all patients with C5–C6 plexus injuries are expected to regain elbow flexion with a motor grade level of greater than 3 (the ability to against gravity). Patients with involvement of C5–C6–C7 demonstrate less predictable results. 2 , 3 , 4 Most patients will experience transient postoperative ulnar nerve paresthesias that resolve spontaneously. Grip strength is expected to be equal to the contralateral unaffected extremity. Younger patients are expected to have more reliable results than older patients. The procedure has less successful outcomes if performed > 9 months after date of injury.
22.4 Indications
Upper brachial plexus injuries.
Pediatric peripartum Erb –Duchenne palsy without spontaneous resolution.
Musculocutaneous nerve injury proximal to the biceps muscle branch.
22.5 Contraindications
Lower brachial plexus injuries (involvement of C8– T1).
Ulnar nerve dysfunction.
18 months from initial injury.
22.6 Special Considerations
A detail-oriented examination is imperative preoperatively.
Ulnar nerve sensory and motor function should be carefully examined.
Preoperative electromyography (EMG) is recommended to confirm examination findings and demonstrate a lack of spontaneous reinnervation of the biceps.
Other deficits, which can be surgically addressed simultaneously, should be evaluated
22.7 Special Instructions, Positioning, and Anesthesia
General anesthesia is recommended.
Patient is positioned supine with the arm abducted and externally rotated on a hand table.
No tourniquet is used.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree