21 Nerve Conduits for Nerve Repair/Reconstruction
Abstract
A tension-free repair for sensory nerve injuries cannot always be achieved. Gaps in the neural tissue can often be bridged with a nerve conduit, usually made of polyglycolic acid or animal- derived collagen. Results appear to be best for sensory nerve defects less than 20 mm in length, although studies have demonstrated limited success for mixed motor and sensory nerve injuries.
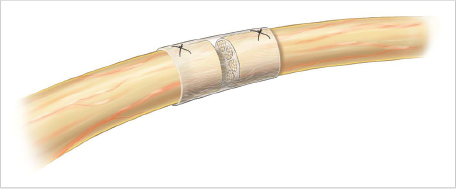
Preparation of the nerve ends is an important first step in obtaining a successful outcome. The internal diameter of the nerve conduit should be slightly wider than the nerve being reconstructed to simplify its insertion and accommodate postoperative swelling. During suture fixation of the conduit, the lumen must be carefully filled with sterile saline or heparinized saline to discourage clot formation, which could compromise axonal ingrowth. Temporary splint immobilization and a therapy program must then be followed to optimize outcomes.
21.1 Description
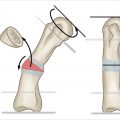
The primary goal of nerve repair is to provide a framework to maximize the number and concentration of axonal fibers that regenerate across a nerve repair site. This requires precise apposition of two sides of a transected nerve using a minimum number of sutures. If a tension-free repair cannot be completed primarily, then the use of a nerve conduit may be beneficial to span defects up to 30 mm in length.
21.2 Key Principles
The assessment of nerve function requires a thorough preoperative motor and sensory physical examination. The surgical approach is facilitated by using loupes or a microscope for appropriate magnification of the operative field. The microsurgical technique typically utilizes 8–0 or 9–0 synthetic suture with suitable instruments.
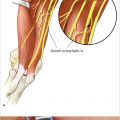
When repairing digital nerves, it is best to avoid positioning the adjacent joint into an extreme position simply to relieve tension at the nerve repair site. If necessary, excessive tension can be avoided by using a synthetic absorbable nerve conduit (► Fig. 21.1). Traditionally, nerve conduits are used for defects less than 30 mm in length, but results appear to be best for defects less than 20 mm. 1
21.3 Nerve Conduit Characteristics
21.3.1 Advantages of Nerve Conduits
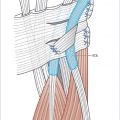
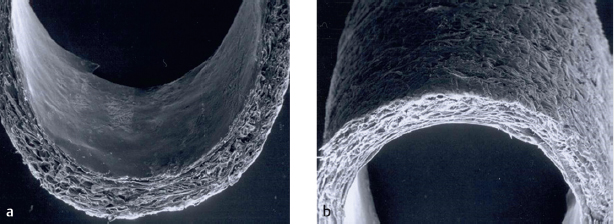
Commercially available, absorbable nerve conduits provide a noncollapsible scaffold for nerve reconstruction that features excellent availability without the disadvantages of donor site morbidity. The use of nerve conduits also provides a simplified means of reconstruction which is arguably superior to autogenous nerve grafting. Multiple size options are available, and nerve conduit walls are semipermeable, which helps in maintaining the influx of nutrients and other factors required for optimal nerve regeneration (► Fig. 21.2).
21.3.2 Materials for Nerve Conduits
Numerous materials for nerve conduits have been investigated. However, the optimal conduit material remains undetermined. In 1982, Lundborg et al published their results on bridging rat sciatic nerves using silicone tubes. 2 Unfortunately, silicone conduits are nondegradable, causing inflammation of the surrounding tissues, secondary nerve constriction, and local discomfort. A secondary surgery is required for the removal of silicone conduits, which makes them less ideal for nerve reconstructions.
Polyglycolic acid conduits are composed of a biodegradable thermos-polymer and absorb reliably in vitro via simple hydrolytic reactions. A randomized prospective study of digital nerve reconstructions using polyglycolic acid conduits demonstrated superior return of sensation when performed for nerve gaps of 4 mm or less. 3
For nerve gaps up to 30 mm, Mackinnon and Dellon 4 reported on 15 patients who underwent polyglycolic acid nerve conduit reconstructions. Clinical recovery was comparable to that of nerve autograft and end-to-end repair: Five patients (33%) demonstrated S4 sensory function, eight (53%) had S3 sensation, and two (14%) had S2 sensation or less. After implantation, polyglycolic acid conduits break down over a period of 90 days.
Conduits made of caprolactone polyester have been shown to be a viable option for nerve reconstruction. This substance is degraded in vivo over the course of 2 years. Unfortunately, the prolonged degradation time may lead to problems with foreign body reaction, graft extrusion, and even fistulization. 5
Bovine and porcine collagen conduits have become increasingly popular. Like other conduit materials, collagen is an attractive material as it is porous, biocompatible, and absorbable. In a retrospective review of collagen conduit reconstruction for average defects measuring 12.8 mm, 35% of patients demonstrated objective sensory improvement. 6 A prospective study by Taras et al 7 found that mean moving two-point discrimination and static two-point discrimination measured 5.0 and 5.2 mm, respectively, for those patients with measurable recovery following collagen conduit reconstruction for digital nerve injuries. Excellent results were achieved in 13 of 22 digits, good results in 3 of 22 digits, and fair results in 6 of 22 digits. There were no poor results.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree