20 Peripheral Nerve Injury and Repair using Autograft or Allograft
Abstract
Peripheral nerve injuries can lead to significant motor and/or sensory disturbances in patients. These injuries can be difficult to treat and a thorough understanding of nerve anatomy, pathophysiology, and repair options are critical for optimizing patient outcomes. There are multiple options available for treatment including direct neurorrhaphy, as well as bridging a nerve defect with autograft, or allograft, and recent advances in the field of microsurgery have led to improvement in patient outcomes. Several key steps during nerve repair, no matter which method is used, are important to ensure that an optimal healing environment is created.
20.1 Background
Nerve injuries can be a catastrophic event for patients and a major clinical challenge to treating surgeons. Although major advances have been made in the field of microsurgery leading to improvements in peripheral nerve repair results, the outcomes of such injuries continue to be unpredictable. With a thorough understanding of nerve anatomy and pathophysiology, attentive microsurgical technique, and adherence to important nerve repair principles, prognosis for satisfactory functional recovery is maximized.
20.2 Nerve Anatomy
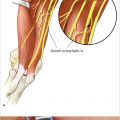
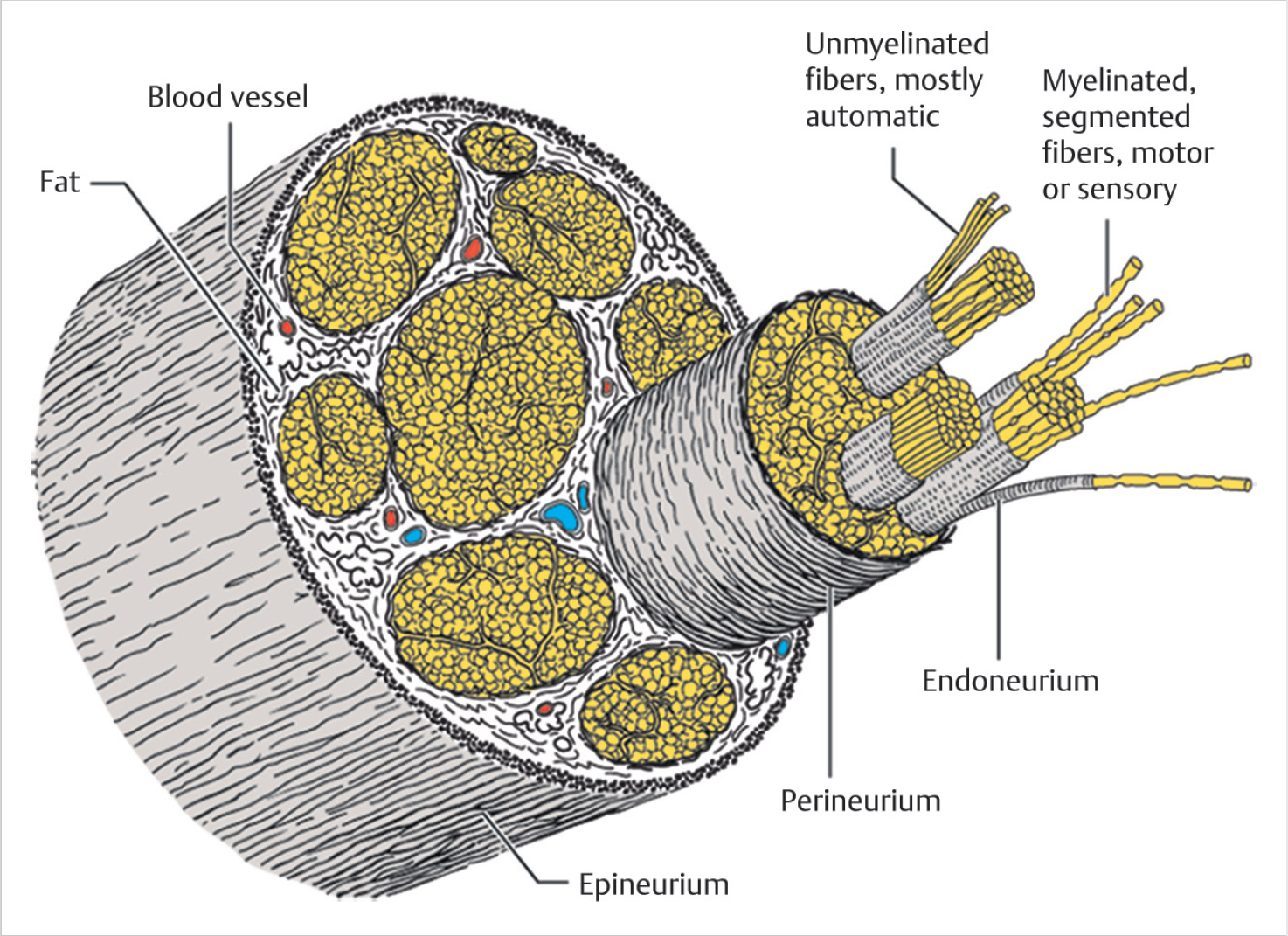
Peripheral nerves are organized into a network of nerve components and connective tissue. The endoneurium, perineurium, and epineurium comprise the framework of connective tissue that organize, nourish, and protect the nerve fibers and axons (► Fig. 20.1). The epineurium encircles the fascicles and acts as a cushion to protect the nerve, a consequence of its thick areolar tissue composition. In addition, the epineurium is highly vascularized, and feeder vessels from the epineurial blood vessels course throughout the inner aspects of the nerve, anastomosing with a vascular network within the perineurium and endoneurium. 1 Within the epineurium lie the fascicles which are surrounded by a perineurium. This layer provides most of the nerve tensile strength. The innermost layer is the endoneurium, which runs within the fascicles, protecting and nourishing the individual axons.
20.3 Pathophysiology
Trauma to a nerve results in a sequence of events affecting the proximal and distal ends of the transected or injured nerve. The proximal axonal segment undergoes degeneration extending to the nearest node of Ranvier, although depending on the type of injury and mechanism, the cell body may also die in the process. Distally, the axon undergoes Wallerian degeneration beginning 24 to 96 hours after injury, during which Schwann cells lose their myelin eath, proliferate, and phagocytose myelin and axonal debris. 1
20.4 Injury Classification
Sir Herbert Seddon described and published the original widely used scheme for classifying nerve injuries, which was later expanded by Sunderland in order to account for the variability in prognosis encountered with axonotmetic injuries 2 (► Table 20.1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree