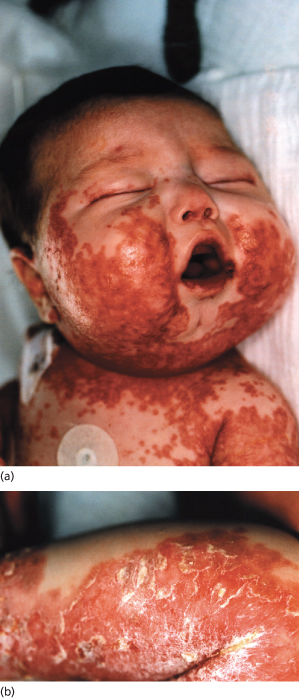
Fig. 170.2 A 4-month-old girl subsequently diagnosed with cystic fibrosis. (a) Desquamating erythematous patches on the face and chest with sparing of the mucous membranes. (b) Erythematous scaling eruption on the calf.
Courtesy of Dr J. Crone.
Cystic Fibrosis and Skin Wrinkling in Water
During the 1970s, many paediatricians reported that the skin of the hands and feet of children with cystic fibrosis would wrinkle much more rapidly than skin from control children when immersed in water and suggested this as a useful diagnostic test for cystic fibrosis [23 and references therein]. In subsequent decades this association was overlooked and many case reports appeared in the dermatological literature of children and adults who developed swelling and increased whitish wrinkling of the palms, often with a burning or itchy sensation, when exposed to water. Some were noted to have cystic fibrosis and/or hyperhidrosis. This condition was given a variety of names, transient aquagenic palmar hyperwrinkling probably being the most accurate. A recent report described a 10-year-old boy with transient aquagenic palmar hyperwrinkling and diabetes who was found to have cystic fibrosis based on increased sweat chloride levels [23].
Other Skin Manifestations
Infants newly diagnosed with cystic fibrosis typically develop a significant and sometimes erosive perianal dermatitis upon commencement of treatment with pancreatic enzymes. Enzymes being passed in stool are thought to contribute to this and it is self-limiting, just requiring barrier ointments. In older children on treatment for cystic fibrosis, the most common skin problems are erythematous or purpuric reactions secondary to the multiple antibiotics and other medications used in treatment regimes [24–26]. Palpable purpuric rashes indicative of vasculitis may be associated with vasculitis in other organs, including joints, kidney and brain [6]. Photosensitivity reactions from quinolone and tetracycline antibiotics are more common in children with cystic fibrosis and may be under-recognized. Up to 50% of adults with cystic fibrosis may develop photosensitivity with ciprofloxacin, and photosensitivity from this antibiotic induced by indoor fluorescent lighting has been reported in a 12-year-old girl [26].
About 40% of older children with cystic fibrosis who develop arthritis also have an associated rash. This is usually erythematous and maculopapular, but purpura, vasculitic nodules and erythema nodosum have also been observed [5,6,27]. Cutaneous reactivity to Aspergillosis species is common, particularly in children with more severe lung disease. The prevalence of cutaneous reactivity to other allergens used to test for atopy is the same as in the normal population [28–30]. The frequency and severity of acne in a group of 102 adolescents with cystic fibrosis at our institution were not higher than in the general population. In another study, a group of 100 children and adults with cystic fibrosis was shown to have a prevalence (not defined in the report) of acute urticaria of 9% and chronic urticaria of 7% [31].
Isolated associations between cystic fibrosis and Rothmund–Thomson syndrome [32], solar urticaria [33] and albinism [34] have been described and are all likely coincidental. Two children with cystic fibrosis and Kawasaki disease have been reported [35,36], but in both cases the diagnosis of Kawasaki disease is uncertain. Three teenage boys and a girl developed purpura on the lower limbs in conjunction with hypergammaglobulinaemia: all four died within 2 years of onset of purpura [37,38]. Mascaro et al. [39] described three siblings of consanguineous parents who had generalized follicular hamartoma and cystic fibrosis and suggested that there may be a genetic linkage between the two conditions.
Prognosis.
Untreated, cystic fibrosis usually leads to death during infancy or childhood from malabsorption and/or pulmonary disease. With continued treatment, the quality and length of life are greatly improved. Most children live active childhoods and, in leading centres, life expectancy of patients born in 2009 is expected to be greater than 50 years [3].
Diagnosis.
Many countries now routinely screen for cystic fibrosis by looking for elevated trypsinogen levels in neonatal heelprick blood. In these countries, diagnosis precedes the development of significant clinical problems and appears to provide better short-term [40] and long-term [3] outcomes and is cost-effective [3]. In countries where neonatal screening is not routine, laboratory diagnosis after the onset of symptoms is either by DNA analysis or by pilocarpine iontophoresis (sweat test) carried out in an experienced centre. In conjunction with appropriate clinical findings, a sweat test is highly sensitive and specific. However, infants with cystic fibrosis who present with a desquamating rash and/or oedema commonly give false-negative sweat test results [5,11] and need to be retested after treatment of their malabsorption. Children or adults presenting with transient aquagenic palmar hyperwrinkling should be assessed for cystic fibrosis [23].
The differential diagnosis depends on the clinical presentation and includes other causes of pulmonary disease, malabsorption or failure to thrive. In infants presenting with a widespread rash and failure to thrive, the differential diagnosis includes multiple causes of zinc, biotin, essential fatty acid, protein and amino acid deficiencies (e.g. inborn errors of metabolism, dietary deficiencies or increased losses from the gastrointestinal or urinary tracts) and immunodeficiency.
Prevention.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








