17 Lower Eyelid Rejuvenation and Blepharoplasty
Introduction
The lower eyelid ages as a result of the progressive descent of the malar complex, with or without concomitant facial volume deflation, which leads to the elongation of the lower eyelid, and the herniation or pseudoherniation of the orbital fat pads. This cheek descent creates a gutter-like depression at the inferior orbital rim, known as the tear trough deformity, which patients describe as the “circles under my eyes,” and above which they notice as “bags under my eyes.” The goal of lower eyelid rejuvenation is to recreate the characteristics of a youthful eyelid, which include reestablishment of the eyelid-malar complex continuum (also known as the single convexity), elimination of visible fat, and achievement of smooth, wrinkle-free skin, all while maintaining normal position and function.
While traditional approaches often focused on the removal of varying amounts of skin, muscle, and fat, current thinking has shifted to include a broader palate of approaches, both surgical and nonsurgical. Newer techniques, such as the transconjunctival approach, which may be combined with laser resurfacing or with a chemical peel, have allowed today’s surgeons to achieve excellent and more natural results while decreasing the risks for ectropion, contour deformity, and scarring. Recent technique modifications include fat preservation with transposition to correct the tear trough deformity, autologous fat transfer, dermal fillers, noninvasive skin tightening procedures (Thermage [Solta Medical Inc.], Ulthera [Ulthera, Inc.]), and lasers, which are used alone or in combination to rejuvenate the cheek-eyelid junction.
Achieving surgical success in lower blepharoplasty can be challenging and requires meticulous patient selection, intimate knowledge of the anatomy, and the selection and execution of the appropriate surgical and adjunctive techniques. This chapter will address the evaluation and surgical management of patients seeking lower blepharoplasty. It will also explore the use of adjuvant therapies, such as fillers, botulinum toxin A, radiofrequency, focused ultrasound, lasers, and chemical peels, and the role each plays in the rejuvenation of the lower eyelids. Surgical correction of midface ptosis performed in conjunction with lower blepharoplasty is sometimes necessary in order to achieve the desired aesthetic results. Please refer to Chapter 27 for comprehensive coverage of surgical treatment of the midface.
Surgical Anatomy
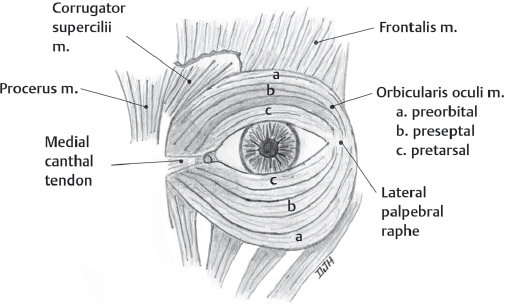
The upper and lower eyelids are composed of analogous layers of skin, muscle, and fat. Eyelid skin is the thinnest in the body, and the lower lid skin, in particular, becomes thin and wrinkled with aging. Beneath the skin and subcutaneous tissue lies the thin orbicularis oculi muscle. This circumferential muscle is innervated by the zygomatic branch of the facial nerve and is divided into two portions named by the regions that it overlaps: orbital and palpebral. The orbital portion is generally not encountered in blepharoplasty surgery, but contributes to the formation of lateral canthal wrinkles or “crow’s feet.” The palpebral portion is further subdivided into the pretarsal and preseptal regions ( Fig. 17.1 ). Hypertrophy of the orbicularis muscle can be seen, and the surgeon must be able to identify this as compared to lower lid fat hypertrophy, as the two are treated differently. Conservative muscle resection is indicated for pretarsal muscle hypertrophy, or, in mild cases, botulinum neurotoxin A can be injected to relax the muscle.
Deep to the preseptal orbicularis muscle lies the orbital septum, a fibrous structure that divides the orbit into anterior and posterior compartments. Weakening of the septum with aging allows for herniation of the underlying fat pads. The orbital septum arises from the orbital rim periosteum at the arcus marginalis and blends into the lower lid capsulopalpebral fascia (the anatomic analogue of the levator aponeurosis of the upper eyelid) ( Fig. 17.2 ).
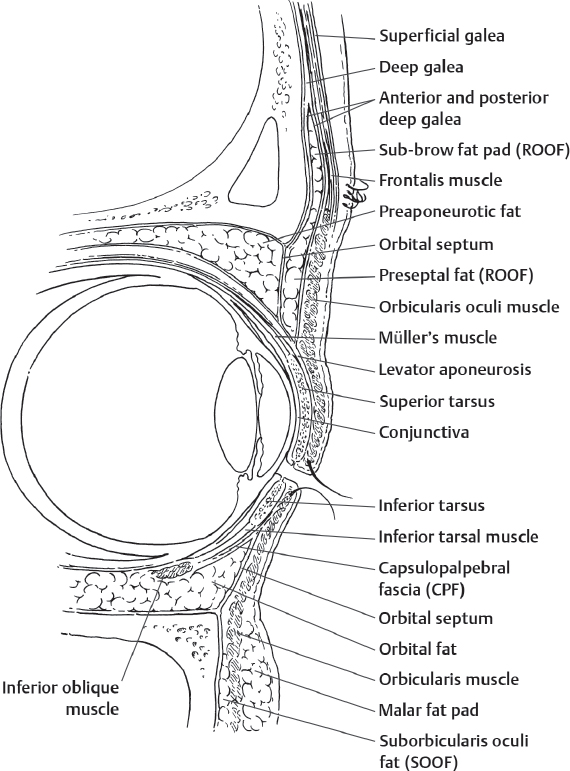
The three preaponeurotic fat pads of the lower lid are separated into central, medial, and lateral compartments. Large blood vessels may supply these fat pads, and meticulous hemostasis much be maintained to prevent retrobulbar hematoma and resulting blindness. The inferior oblique muscle courses between the medial and central compartments. During blepharoplasty surgery, care must be taken to avoid injury to this muscle, which could result in diplopia.
Preoperative Evaluation
Identifying the anatomic features that place a patient at risk for complications from lower blepharoplasty and formulating the appropriate surgical plan are perhaps as important, if not more important, than the surgery itself. In addition to obtaining a careful history regarding the health of the ocular surface, dry eyes, rosacea, allergies, and laser eye and glaucoma surgery, to name the most common, a methodic approach to the evaluation should follow. There are eight parts to the lower eyelid exam, and these include general inspection, skin, muscle, fat, eyelid laxity, vector, tear trough, and cheek position. Massry 1 described his approach to the lower eyelid evaluation using a mnemonic, SMFTV, to elicit the skin, muscle, fat, tone, and vector portions of the exam. We promote the expanded evaluation that follows:
General Inspection: Begin the evaluation by noting the position and prominence of each eye, each orbit, and their symmetry. Observe the position of each lower eyelid relative to the inferior corneal limbus, to the upper eyelid, to each canthus, and to each other. Note the presence of conjunctivochalasis, as this predisposes the patient to postoperative chemosis. The normal lower eyelid rests 1 mm above the limbus, 10 to 12 mm from the upper eyelid (the palpebral fissure), and is approximately 30 mm in length from the medial to the lateral canthal angles (intercanthal distance). The canthal tendons insert at the medial and lateral orbital rims, and provide a firm attachment for the eyelids, which defines the sharpness and position of the canthal angles. Lateral canthal rounding and distractibility, bowing of the lower eyelid, and inferior scleral show are signs of underlying excessive laxity, canthal tendon dehiscence, or incipient ectropion, and should lead to consideration of some form of horizontal tightening at the time of lower blepharoplasty. A Schirmer’s test should be performed to document tear production, especially in the reportedly dry eye and laser eye surgery patients.
Skin: Fine and deep rhytids, instead of true dermatochalasis, are most commonly found in the aging lower eyelid. Evaluate the quality and thickness of the skin in order to decide whether laser resurfacing or a chemical peel should be incorporated into the surgical plan, rather than simple skin removal. With the patient looking up, and the mouth open, attempt to pinch the skin just below the lashes, and consider only that small amount that can be pinched for removal. This maneuver can be performed intraoperatively as well, to avoid overexcision.
Muscle: To assess the orbicularis function, ask the patient to squeeze the eyelids shut as tightly as possible or “as if you have soap in your eyes,” and observe the completeness and strength of the closure. Look for evidence of paralysis or weakness, as in Bell’s palsy. Aberrant regeneration of the orbicularis following recovery from Bell’s palsy presents as a narrowing of the palpebral fissure ipsilateral to the palsy, with increased orbicularis tone at rest, exacerbated by recruitment during activities, such as speaking, chewing, or laughing. Overaction of the preseptal orbicularis has been described 2 as a cause leading to “bags” forming under the eyes, particularly while smiling, and is a common complaint in the prospective surgical patient. Botulinum toxin A may be considered in the isolated case as treatment, or in combination with surgery. Excessive excision of the muscle to correct this overaction is contraindicated as it may affect closure and lead to lagopthalmos and dry eyes.
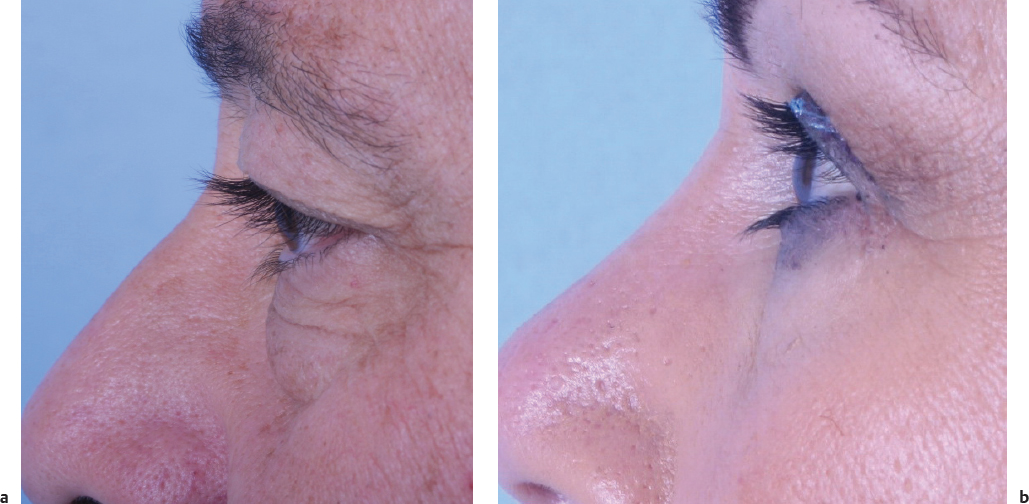
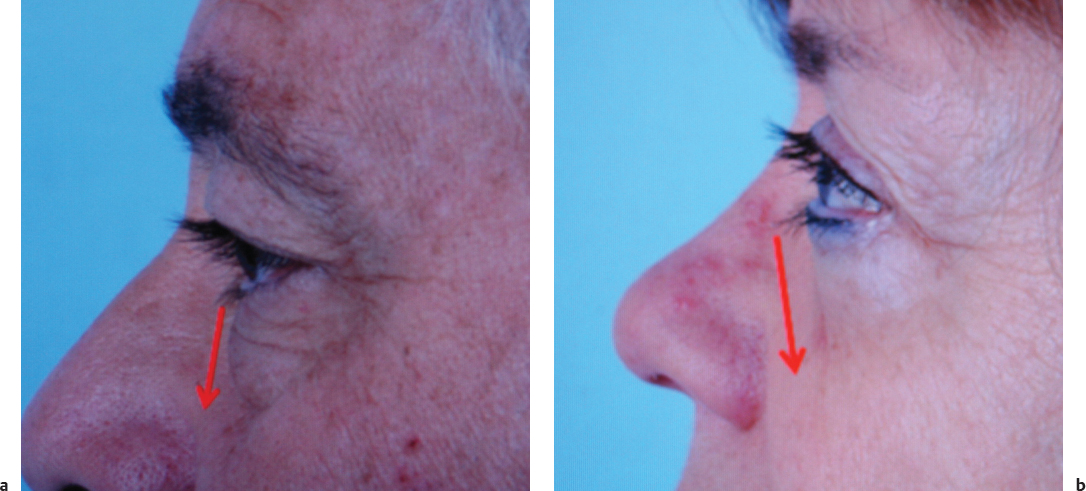
Fat: Although aging of the lower eyelids often leads to the appearance of visible fat, the decision to remove it should hinge on whether there is true prolapse or pseudo-fat prolapse. True fat herniation is defined as prolapse of the orbital fat pads beyond the plane of the cheeks, and this fat may be removed ( Fig. 17.3a ). Evaluate the patient in profile and in the oblique planes, with the patient’s gaze in the primary and upgaze positions. In pseudo-prolapse, the fat is clearly visible as “bags under the eyes,” but the fat does not protrude beyond the plane of the cheeks, and its removal should be avoided ( Fig. 17.3b ). Pseudo-fat prolapse patients typically have an adjacent tear trough deformity and variable degrees of concomitant midface descent, and their treatment should include correction of the midface position and volume at the tear trough if necessary, instead of excessive orbital fat excision.
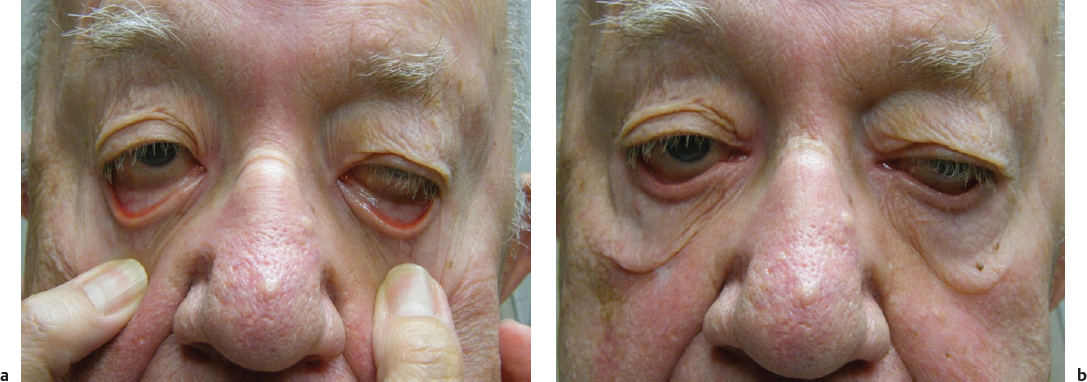
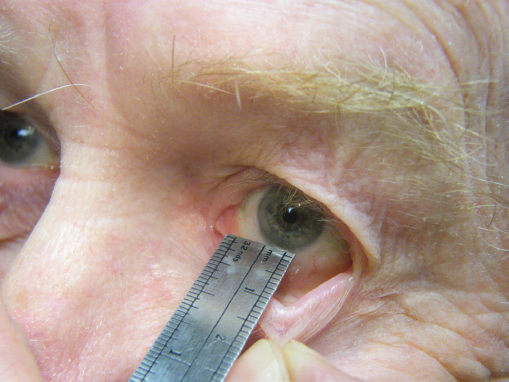
Eyelid Laxity: This is the single most important feature to consider and correct surgically in order to avoid postoperative ectropion. Some form of horizontal tightening is frequently necessary, especially in older patients, and whenever laxity is detected during the preoperative evaluation. The lid retraction or “pull” test ( Fig. 17.4 ) is performed by digitally distracting the lower eyelid inferiorly as far as it will stretch, then releasing it and observing whether the eyelid snaps back into position, slowly returns to its resting position spontaneously, or stays distracted until the patient blinks (poor or absent recoil). The eyelid that does not stretch or hardly distracts away from the eye and that snaps back quickly is considered to have a normal lid retraction test, and horizontal tightening is not necessary. The lid distraction or “pinch” test ( Fig. 17.5 ) also is performed to assess lower lid laxity, by determining the distance the lid can be pulled away from the globe; movement of more than 10 mm indicates excessive laxity. Mild positive results for these tests indicate that a lateral canthopexy, a lateral canthal tendon, and tarsal plication procedure should be considered. When moderate to severe laxity and poor recoil are seen, a lateral tarsal strip should be performed during lower blepharoplasty surgery.
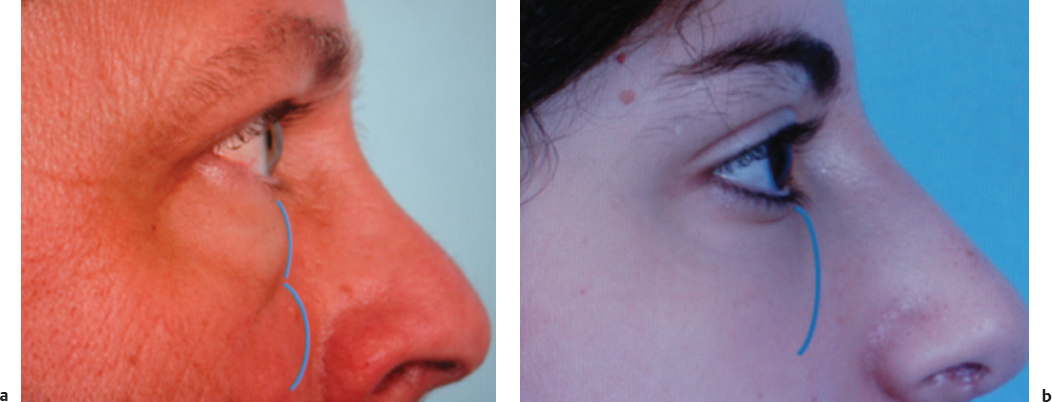
Vector: Vector refers to the angle of the lower eyelid, determined by the relative position of the eye or globe to the orbital rim. The vector can be “positive” when the lower eyelid slants forward from the lash line to the rim in lateral view ( Fig. 17.6a ), “neutral” when the eyelid shows a straight vertical trajectory, and “negative” when the eyelid slants posteriorly ( Fig. 17.6b ). A “negative” vector eyelid should be considered at high risk for postoperative ectropion and eyelid retraction, since the eyelid has an inherently longer, unsupported oblique trajectory to reach the lower limbus. Skin excision should be avoided altogether in these patients. Even isolated transconjunctival fat removal could lead to eyelid retraction and also enhances the prominence of the eye, making the patient appear more “bug-eyed” postoperatively. Consider nonsubtractive options such as fat transfer, with or without midface elevation, or more conservative options like Thermage and dermal fillers instead of lower blepharoplasty in the “negative” vector patient.
Tear Trough: The “tear trough” is the semicircular depression that forms as the malar complex descends away from the lower eyelid with aging. A double convexity is observed in lateral and oblique views ( Fig. 17.7a ). Malar descent also creates a progressive elongation of the lower eyelid with increasing bearing of the orbital fat pads and of the orbital rim. It often starts nasally, with the trough appearing only along the lower eyelid-nasojugal fold junction, 3 and the appearance of visible fat directly above. Some patients have a familial form which is present since early in life. Focal malar or maxillary hypoplasia is frequently found in these patients. 2
Anatomically, the trough itself is concave and consists of skin and orbicularis draped over the inferior orbital rim. The trough is flanked by fat on either side: that of the cheek below, and that of the orbit and the lower eyelid fat pads above. The greater the cheek descent, the wider the tear trough, and the more challenging it is to correct.
Cheek Position: The normal cheek or malar complex position starts well over the inferior orbital rim, approximately 12 to 15 mm from the lower eyelid margin. The volume of the cheek fat obscures the orbital rim and lies in direct apposition to the orbital fat pads to create a smooth eyelidcheek continuum, also known as the single convexity ( Fig. 17.7b ). When the cheek is in normal position, and true orbital fat prolapse is present, lower eyelid blepharoplasty can be performed in isolation to reestablish the eyelidcheek continuum. More often than not, aging of the lower eyelid is accompanied by malar complex descent, and determining what to do about both is crucial to achieving optimal aesthetic results.
Surgical Informed Consent
The risks or lower blepharoplasty, including loss of vision or even blindness, should be carefully discussed with each patient. The risks include damage to the eye or optic nerve, infection, orbital hemorrhage, lower eyelid ectropion, retraction, malposition, contour deformity, eyelid length shortening, palpebral narrowing, diplopia, over-/undercorrection, asymmetry, scarring, exacerbation of dry eyes, exposure keratopathy, lagophthalmos, and the possible need for further surgery. 4 Discuss with the patient what the goals of surgery will be, including what will and will not be possible to correct with blepharoplasty alone. If a horizontal tightening procedure is planned, discuss the implications of that surgery and possible lateral canthal angle, eyelid and lash line length shortening, trichiasis at the lateral commissure or elsewhere, and eyelid fissure changes.
Photographic Documentation
Preoperative photographic documentation is essential in any cosmetic surgery. Standard views include the forward, lateral, and three-quarter views ( Fig. 17.8 ). To visualize the lower lid fat pads, an additional view is taken with the patient performing an upward gaze. Such motion allows for protrusion of the fat and the surgeon can better assess the contribution of each of the fat pads to the patient’s lower lid bags.

Development of the Surgical Plan
Armed with the clinical data from the preoperative analysis and with knowledge of the lower lid anatomy, the surgeon must develop a precise surgical plan for each patient’s lower blepharoplasty surgery. Each layer of the eyelid must be evaluated and treated appropriately. First, the skin condition dictates the surgical approach. If redundant skin of the lower lid must be excised, a subciliary incision is used. If either no skin or a small pinch of skin excision is necessary, the transconjunctival approach is utilized. Similarly, if pretarsal orbicularis muscle must be excised, a subciliary approach is mandated. Lower lid laxity also dictates approach, as the transconjunctival approach is less likely to result in the development of ectropion. Next, it is important to have an idea preoperatively of which fat pads must be resected, as not all patients require removal of all three pads. Finally, the status of the inferior orbital rim will dictate if fat needs to be transposed or transferred to camouflage the tear trough deformity.
Surgical Procedures
Subciliary Blepharoplasty
The procedure is performed under general or intravenous sedation anesthesia. Local anesthesia (1% lidocaine with 1:100,000 epinephrine) is infiltrated using a 30-gauge needle. A stab incision is created in the lateral canthal region, and a Westcott scissors is used to extend the subciliary incision just below the lash line ( Fig. 17.9a ). The incision stops 4 to 5 mm lateral to the tear duct punctum. A traction suture of 5–0 nylon may be used to pull the lid superiorly, which both protects the globe from injury and provides countertraction support to assist in skin undermining. While seated at the patient’s head, the surgeon dissects initially in the subcutaneous plane keeping the pretarsal orbicularis muscle intact, and then enters the submuscular plane just deep to the preorbital division of the orbicularis muscle, thus producing a “skin-muscle” flap. The dissection extends in the submuscular plane to the level of the inferior orbital rim.
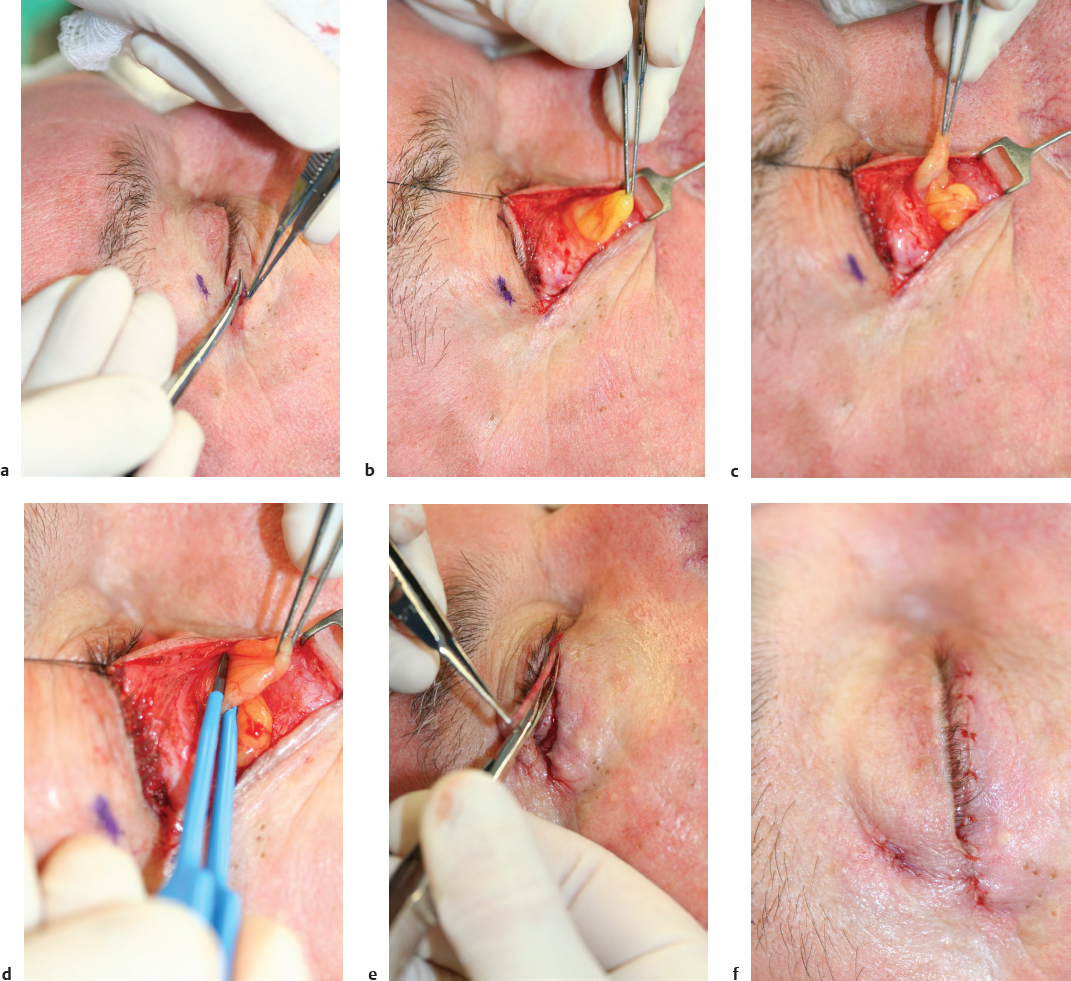
The medial, central, and lateral fat pads are nicely exposed using this approach ( Fig. 17.9b ). The medial fat pad is a lighter yellow color than the central and lateral pads, which aids in fat pad identification ( Fig. 17.9c ). Each pad is gently teased away from the surrounding tissue, and a bipolar cautery is used to cauterize the base of the pad before excision ( Fig. 17.9d ). Meticulous hemostasis must be obtained.
The skin of the lower eyelid is then redraped and the nylon traction suture removed. Conservative skin removal is essential to prevent ectropion. Usually no more than 2 to 3 mm of skin is excised ( Fig. 17.9e ). If the patient is under sedation, they may be asked to open their mouth widely and look upward, which puts the lower lid on maximum extension and assists in redraping the skin conservatively to assess the amount to excise. The skin edges are then reapproximated using a 6–0 fast absorbing gut ( Fig. 17.9f ). Occasionally, redundant orbicularis muscle on the skin flap must be excised to prevent a ridge at the suture line.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








