Abstract
Tendinitis refers to acute inflammation due to acute damage or overuse. Tendinosis refers to chronic, often attritional damage due to overuse, abnormal anatomy, or degenerative conditions. There is significant overlap. “Tendinopathy” encompasses both. They may affect any flexor or extensor tendons, typically within a sheath or at inflection point, but may also affect tendon origin/insertions, in which case they are considered enthesopathies. Understanding the anatomy of the hand, wrist and elbow is key to diagnosis. History can elucidate mechanism and help isolate pathology in most cases and advanced imaging is rarely indicated. Management is often conservative at the outset, with surgical treatment indicated in recalcitrant cases. Dupuytren disease, a fibro-proliferative genetic condition of incomplete penetrance, may lead to the evolution of cords and nodules in the hand and fingers. Treatment is typically reserved for cases leading to significant contracture and consists primarily of surgery, needle aponeurotomy or collagenase injection.
12 Tendinitis, Tendinosis, and Dupuytren’s Contracture
I. Tendinitis and Tendinosis of Hand and Wrist
Tendinitis refers to acute inflammation due to acute damage or overuse. Tendinosis refers to chronic, often attritional damage due to overuse, abnormal anatomy, or degenerative conditions. There is significant overlap. “Tendinopathy” encompasses both.
They may affect any flexor or extensor tendons, typically within a sheath or at inflection point, but may also affect tendon origin/insertions, in which case they are considered enthesopathies.
Avoid giving diagnosis of “tendinitis” to patients with nonspecific overuse pain. Nonspecific or specific overuse pain that is seemingly related to occupation may benefit from a formal ergonomic assessment versus self-directed activity modification.
History can elucidate mechanism and help isolate pathology in most cases. Physical examination is usually confirmatory. Special diagnostic tests such as MRI and ultrasound are necessary only in specific cases and should not be ordered without clear reason.
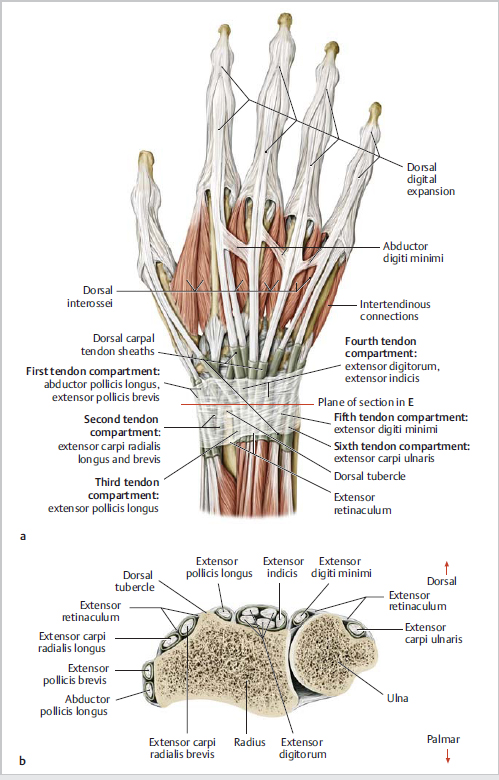
Understanding location of the six extensor compartments at the wrist (► Fig. 12.1) and flexor and extensor tendon anatomy is key to diagnosis.
A. Wrist Flexor/Extensor Tendinitis
Flexor carpi radialis (FCR)
Most common in people with exposure to seawater and the immunocompromised.
Most common in people with exposure to seawater and the immunocompromised.
Most common in people with exposure to seawater and the immunocompromised.
Most common in people with exposure to seawater and the immunocompromised.
Flexor carpi ulnaris (FCU)
Most common in people with exposure to seawater and the immunocompromised.
Most common in people with exposure to seawater and the immunocompromised.
Most common in people with exposure to seawater and the immunocompromised.
Extensor carpi radialis longus (ECRL) and extensor carpi radialis brevis (ECRB)
Most common in people with exposure to seawater and the immunocompromised.
Most common in people with exposure to seawater and the immunocompromised.
Conservative treatment, with splinting, activity modification, rarely CSI, and surgical intervention with craterization of boss with or without CMC fusion and tendon repair is rarely needed.
B. Stenosing Tenosynovitis—“Trigger Finger”
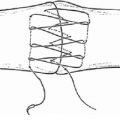
Thickening of flexor tendon at the level of A1 pulley with eventual formation of nodule of inflammatory tissue at the level of Camper’s chiasm (► Fig. 12.2).
Tenderness with or without palpable nodule at A1 pulley.
May be associated with retinacular cyst.
Early—just pain, progresses to “locking”.
Grading
Pain, no clicking.
Pain, clicking, easily reducible.
Must be reduced manually.
Locked, irreducible.
Initial treatment
CSI90 + % effective, approximately 70% long-term efficacy
Less effective in diabetes mellitus (DM).
May try up to three CSI (decreased efficacy with repeated injection).
Nighttime extension splinting and physical therapy (PT)/OT may be effective in reducing symptoms.
Surgical treatment
Release of A1 pulley—can be performed under local anesthesia.
Recurrence rate very low (< 5%) after surgery.
Failed surgery may require re-release with release of A0 and proximal A2 pulleys versus excision of one slip of flexor digitorum superficialis (FDS).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree