Differential Diagnosis.
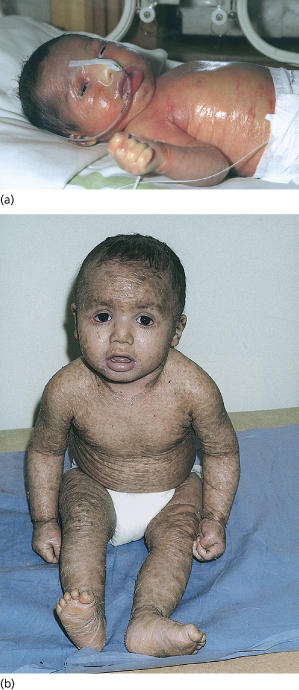
A collodion membrane baby is generally easily distinguished from the more severe harlequin fetus/ichthyosis presentation, but occasional cases with intermediate features have been recorded. These have in the past been referred to as ‘chrysalis babies’. Restrictive dermopathy or the ‘stiff baby syndrome’ produces a generalized taut, thick, tethered and unyielding skin at birth, which does not desiccate in the neonatal period. Its persistence causes respiratory failure and early neonatal death.
Complications and Prognosis of Collodion Membrane.
The collodion membrane is associated with impaired epidermal barrier function and resultant increased transepidermal heat and water loss. Hypothermia and dehydration quickly develop, and hypernatraemia is a particularly serious metabolic complication that can lead to renal failure and neurological damage [36]. Increased absorption of topical agents such as antiseptics, salicylic acid and steroids through the skin may lead to rapid systemic toxicity due to the impaired epidermal barrier.
Bacterial sepsis due to infected cutaneous erosions and fissures is a constant threat and, together with renal dysfunction, was previously a common cause of death of collodion babies. Larregue et al. [7], in a review of 29 collodion babies in 1976, recorded a mortality of 33% but in their update in 1986 (including 32 new cases and 39 reported in the literature), the mortality rate had fallen to 11%. Most infants died from infection but, with better recognition of the condition and the availability of intensive neonatal care, the current mortality is negligible [8].
Early investigation to identify the diagnosis may include blood film, hair microscopy, hearing test, metabolic studies and, rarely, skin biopsy, transglutaminase activity assays on skin biopsy and mutational analysis on peripheral blood. In the UK, the majority of paediatric dermatologists wait to see what the clinical phenotype is before considering skin biopsy (usually not needed) or mutation analysis.
Treatment.
Affected infants should be nursed from the beginning in humidified incubators to maintain body temperature and prevent dehydration. Regular monitoring of vital signs, blood counts, electrolytes and renal function is needed. Intravenous fluid therapy may be required, and facilities for peritoneal dialysis should be available.
Skin care can include the use of aqueous cream to cleanse the skin and a lubricating, water-resistant emollient such as white soft paraffin, which should be applied regularly at feeding times and each nappy change. Aseptic handling is extremely important to reduce the risk of infection. The possible link between emollient use or intravenous lines and skin infection was highlighted in one report [8]. Single-dose (sterile) emollient containers or pump dispensers should be used. Signs of skin or systemic sepsis must be investigated and treated immediately. Candida or Pseudomonas infection of the skin and eyes is common because of the high-humidity environment. Candida albicans
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree