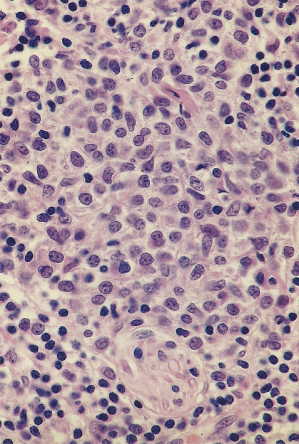
Fig. 101.2 Detail of dermal infiltrate with numerous plasmacytoid monocytes, surrounded by several normal-sized lymphocytes.
Clinical Features.
Jessner’s lymphocytic infiltrate is usually found in adults of middle age. Classically, JLI is regarded as a condition of older males, but good epidemiological data are lacking. Of the two largest studies to date, there is a slight female preponderance in the series of 100 cases by Toonstra et al. [5] and slightly more males in the series reported by Lipsker et al. [15]. There are few reported cases of JLI in childhood [16,17]. The youngest reported case is of a 4-year-old boy (whose mother was also affected) [18]. Familial cases have been reported elsewhere [19,20].
The condition manifests as erythematous-to-brownish coloured papules and plaques (Fig. 101.3). These may exhibit central clearing and can take on an arcuate appearance. The lesions are usually asymptomatic but can be tender or pruritic. Distribution is predominantly on the head, neck and upper trunk although arms and, less frequently, legs may be affected. Lesions may be exacerbated by sunlight and provoked by phototesting but these are not consistent features. In one series, some patients reported emotional stress as a trigger factor [5]. Lesions may last for several months and rarely may be persistent.
Fig. 101.3 Clinical picture of Jessner’s lymphocytic infiltrate. In this 20-year-old female patient, lesions developed for the first time at the age of 12.

Differential Diagnosis.
There are multiple conditions which may present with similar clinical findings. The main differentials include subtypes of cutaneous lupus erythematosus (e.g. discoid lupus erythematosus or lupus erythematosus tumidus), polymorphic light eruption (which may occur along with JLI [5]), lymphoma, pseudo-lymphoma and cutaneous drug eruptions. Diagnostic skin biopsy with H&E and direct immunofluorescence may differentiate some of these alternative diagnoses. The role of antinuclear antibody serology is uncertain. For a differential of lymphoma or lymphocytoma cutis, or in possible lupus where immunofluorescence is negative, immunohistochemistry may assist. A diagnosis of JLI relies on the marrying of clinical and histological findings as well as other investigations such as phototesting and serology.
Prognosis.
The course of JLI tends to follow a chronic relapsing and remitting pattern. The condition tends to last for several years (10–15 is not uncommon) and has been reported to last for 20 or more years in some affected individuals. In one of the largest studies [5], no progression to either lymphoma or lupus erythematosus was found. A multicentre series with 32 JLI patients also found no progression [6]. However, a large retrospective study of 210 patients found that 7.6% of cases also had typical findings of lupus erythematosus at some point during follow-up [15].
Treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








