Epidermal Necrolysis (Stevens–Johnson Syndrome and Toxic Epidermal Necrolysis): Introduction
|
Toxic epidermal necrolysis (TEN) and Stevens–Johnson syndrome (SJS) are acute life-threatening mucocutaneous reactions characterized by extensive necrosis and detachment of the epidermis. Stevens and Johnson first reported two cases of disseminated cutaneous eruptions associated with an erosive stomatitis and severe ocular involvement.1 In 1956, Lyell described patients with epidermal loss secondary to necrosis and introduced the term toxic epidermal necrolysis.2 Both SJS and TEN are characterized by skin and mucous membrane involvement. Because of the similarities in clinical and histopathologic findings, risk factors, drug causality, and mechanisms, these two conditions are now considered severity variants of an identical process that differs only in the final extent of body surface involved.3–5 Therefore, it is better to use the designation epidermal necrolysis for both, as proposed by Ruiz-Maldonado (acute disseminated epidermal necrosis)6 and Lyell (exanthematic necrolysis).7
Epidemiology
Epidermal necrolysis (EN) is rare. The overall incidence of SJS and TEN was estimated at 1 to 6 cases per million person-years and 0.4 to 1.2 cases per million person-years, respectively.8,9 EN can occur at any age, with the risk increasing with age after the fourth decade, and more frequently affects women, showing a sex ratio of 0.6. Patients infected with human immunodeficiency virus and to a lesser degree patients with collagen vascular disease and cancer are at increased risk.10–12 The overall mortality associated with EN is 20% to 25%, varying from 5% to 12% for SJS to more than 30% for TEN. Increasing age, significant comorbidity, and greater extent of skin involvement correlate with poor prognosis. In the United States, evaluation of death certificates suggested a seven time higher risk of dying from EN among blacks than whites.13
A prognosis score (SCORTEN) has been constructed for EN,14 and its usefulness has been confirmed by several teams.15–18 (See Table 40-1.)
SCORTEN | |
Prognostic Factors | Points |
| 1 |
| 1 |
| 1 |
| 1 |
| 1 |
| 1 |
| 1 |
SCORTEN | Mortality Rate (%) |
0–1 | 3.2 |
2 | 12.1 |
3 | 35.8 |
4 | 58.3 |
5 | 90 |
Etiology
The pathophysiology of EN is still unclear; however, drugs are the most important etiologic factors. More than 100 different drugs have been implicated,19–21 but fewer than a dozen “high-risk” medications account for about one half of cases in Europe (Table 40-2), as evidenced by two multinational case–control studies.12,22–25 These high-risk drugs are antibacterial sulfonamides, aromatic anticonvulsants, allopurinol, oxicam nonsteroidal anti-inflammatory drugs, lamotrigine, and nevirapine.26–27 The risk seems confined to the first 8 weeks of treatment. Slow dose escalation decreases the rate of rash with lamotrigine and nevirapine,28,29 but there is no evidence that it decreases the risk of EN.26 Oxcarbazepine, a 10-keto derivative of carbamazepine, which was considered to carry a lower risk, seems to significantly cross-react with carbamazepine.30 Many nonsteroidal anti-inflammatory drugs (primarily oxicam derivatives and diclofenac) were suspected to be associated with EN.12,31,32 A significant but much lower risk has also been reported for non-sulfonamide antibiotics such as aminopenicillins, quinolones, cephalosporins, and tetracyclines.22 Corticosteroids were significantly associated with a high relative risk, but confounding was not excluded.22
High Risk | Lower Risk | Doubtful Risk | No Evidence of Risk |
|---|---|---|---|
Allopurinol Sulfamethoxazole Sulfadiazine Sulfapyridine Sulfadoxine Sulfasalazine Carbamazepine Lamotrigine Phenobarbital Phenytoin Phenylbutazone Nevirapine Oxicam NSAIDs Thiacetazone | Acetic acid NSAIDs (e.g., diclofenac) Aminopenicillins Cephalosporins Quinolones Cyclins Macrolides | Paracetamol (acetaminophen) Pyrazolone analgesics Corticosteroids Other NSAIDs (except aspirin) Sertraline | Aspirin Sulfonylurea Thiazide diuretics Furosemide Aldactone Calcium channel blockers β Blockers Angiotensin-converting enzyme inhibitors Angiotensin II receptor antagonists Statins Hormones Vitamins |
The role of infectious agents in the development of EN is much less prominent than for erythema multiforme. However, cases of EN associated with Mycoplasma pneumoniae infection, viral disease, and immunization have been reported, particularly in children.33,34 These rare observations underscore the fact that medications are not the only cause of EN, but there is still little evidence that infections can explain more than a very small percentage of cases.
Cases of EN have been reported after bone marrow transplantation. Some are an extreme form of acute graft-versus-host disease (see Chapter 28); others could be drug induced. The relationship between EN and graft-versus-host disease is difficult to assess because clinical and histological skin features are nearly indistinguishable.35 Lupus erythematosus (systemic LE or subacute cutaneous LE) is associated with an increased risk of EN.12,22 In such cases, drug causality is often doubtful and necrolysis might be an extreme phenotype of cutaneous lupus.36 Finally, radiotherapy in addition to treatment with antiepileptic drugs, such as phenytoin, phenobarbital, or carbamazepine, can trigger EN with lesions localized predominantly at sites of radiation treatment.37,38 In clinical practice, the causality of a medication can be clearly established in approximately 60% of cases and suspected in 20%. Other causes (infection, GVH, LE) are rarely apparent, about 20% of cases as idiopathic.39
Pathogenesis
Even if the precise sequence of molecular and cellular events is incompletely understood, several studies provided important clues to the pathogenesis of EN. The immunologic pattern of early lesions suggests a cell-mediated cytotoxic reaction against keratinocytes leading to massive apoptosis.39–41 Immunopathologic studies have demonstrated the presence within early lesions of cytotoxic cells including natural killer T cells (NKT) and drug-specific CD8+ T lymphocytes; monocytes/macrophages and granulocytes are also recruited.42–44 However, it is generally accepted that specific and nonspecific cytotoxic cells are too few within the lesions to explain the death of cells on the full thickness and large areas of the epidermis and mucous membranes. Amplification by cytokines has been suspected for years, especially for factors activating “death receptors” on cell membranes, especially antitumor necrosis factor (TNF) α and soluble Fas ligand (Fas-L).42,45 In the past decade it had been widely accepted that Fas-L was inducing the apoptosis of keratinocytes in EN,45,46 despite partial evidence and discordant findings.47–49 An important recent study has challenged this dogma by demonstrating the key role in EN of granulysin.50 Granulysin was present in the blister fluid of EN at concentrations much higher than those of perforin, granzyme B, or Fas-L. At such concentrations, only granulysin, and to a much lesser degree perforin, were able to kill human keratinocytes in vitro; Fas-L was not. Furthermore injection of granulysin in the dermis of normal mice resulted in clinical and histological lesions of EN.50
When combined, the above results strongly suggest that the effector mechanisms of EN have been deciphered. Cytotoxic T-cells develop and are usually specifically directed against the native form of the drug rather than against a reactive metabolite, contrarily to what has been postulated for 20 years. These cells kill keratinocytes directly and indirectly through the recruitment of other cells that release soluble death mediators, the principal being granulysin.50,51
These advances on understanding the final steps of the reaction point to inhibition of release and/or blockade of granulysin as major aims of therapeutic interventions.
Little is known on what are the initial and intermediate steps. We still do not understand why very few individuals develop a violent immune response to medications and why effector cells are especially directed to the skin and other epithelia. Actually, most drugs associated with a “high risk” for EN can also induce a variety of milder and more frequent reactions. Drug-specific CD8 cytotoxic T-lymphocytes were also often found in skin reactions with more benign phenotype.52 Hence, it is tempting to speculate on an abnormal regulation of immune response. Regulatory CD4+ CD25+ T cells have been demonstrated to be potentially important in the prevention of severe epidermal damage induced by reactive cytotoxic T lymphocytes in a mouse model of EN.53 Similar regulatory cells may play a role in drug eruptions in humans.54 Altered regulation of the immune response to medications in patients with EN could result from comorbidities that are frequent, for example, cancer, HIV infection, collagen vascular disease; from comedications, for example, corticosteroids; or from genetic background.
Genetic susceptibility plays an important role in the development of EN to a few “high-risk” medications. A strong association was observed in Han Chinese from Taiwan between the human leukocyte antigen HLA-B*1502 and EN induced by carbamazepine, and between HLA-B*5801 and EN induced by allopurinol.55,56 B*1502 association with carbamazepine-related cases was confirmed in several Asian countries,57,58 with the remarkable exceptions of Japan and Korea.59,60 The association between carbamazepine-induced EN and HLA-B*1502 was not present in European patients who do not have Asian ancestry.61 On the other hand, HLA-B*5801 was confirmed to be associated with allopurinol-related EN in Japan59 and Europe,62 but the strength of association was lower than in Taiwan.
Clinical Findings
Even in cases requiring immediate referral to specialized wards, the dermatologist will have a specific role in the management of patients with EN (Fig. 40-1).
EN clinically begins within 8 weeks (usually 4 to 30 days) after the onset of drug exposure for the first time. Only in very rare cases with prior reaction and inadvertent rechallenge with the same drug does it appear more rapidly, within a few hours. Nonspecific symptoms such as fever, headache, rhinitis, cough, or malaise may precede the mucocutaneous lesions by 1 to 3 days. Pain on swallowing and burning or stinging of the eyes progressively develop, heralding mucous membrane involvement. About one-third of cases begin with nonspecific symptoms, one-third with symptoms of mucous membrane involvement, and one-third with an exanthema. Whatever the initial symptoms are, their rapid progression, the addition of new signs, severe pain, and constitutional symptoms should alert one to the onset of a severe disease.
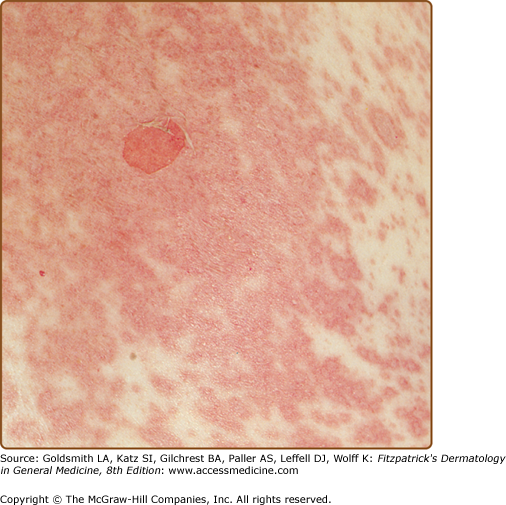
The eruption is initially symmetrically distributed on the face, the upper trunk, and the proximal part of limbs.63 The distal portions of the arms as well as the legs are relatively spared, but the rash can rapidly extend to the rest of the body within a few days and even within a few hours. The initial skin lesions are characterized by erythematous, dusky red, purpuric macules, irregularly shaped, which progressively coalesce. Atypical target lesions with dark centers are often observed (Fig. 40-2A). Confluence of necrotic lesions leads to extensive and diffuse erythema. Nikolsky’s sign, or dislodgement of the epidermis by lateral pressure, is positive on erythematous zones (Fig. 40-3 and eFig. 40-3.1). At this stage, the lesions evolve to flaccid blisters, which spread with pressure and break easily (see Fig. 40-2B). The necrotic epidermis is easily detached at pressure points or by frictional trauma, revealing large areas of exposed, red, sometimes oozing dermis (see Figs. 40-2C and 40-2D). In other areas, epidermis may remain.
Figure 40-2
A. Early eruption. Erythematous dusky red macules (flat atypical target lesions) that progressively coalesce and show epidermal detachment. B. Early presentation with vesicles and blisters, note the dusky color of blister roofs, strongly suggesting necrosis of the epidermis. C. Advanced eruption. Blisters and epidermal detachment have led to large confluent erosions. D. Full-blown epidermal necrolysis characterized by large erosive areas reminiscent of scalding.
Patients are classified into one of three groups according to the total area in which the epidermis is detached or “detachable” (positive Nikolsky): (1) SJS, less than 10% of body surface area (BSA); (2) SJS/TEN overlap, between 10% and 30%; (3) TEN, more than 30% of BSA (eFig. 40-3.2). Correct evaluation of the extent of lesions is difficult, especially in zones with spotty lesions. It is helpful to remember that the surface of one hand (palm and fingers) represents a little less than 1% of the BSA.
Mucous membrane involvement (nearly always on at least two sites) is observed in approximately 90% of cases and can precede or follow the skin eruption. It begins with erythema followed by painful erosions of the oral, ocular, and genital mucosa. This usually leads to impaired alimentation, photophobia, conjunctivitis, and painful micturition. The oral cavity and the vermilion border of the lips are almost invariably affected and feature painful hemorrhagic erosions coated by grayish white pseudomembranes and crusts of the lips (Fig. 40-4). Approximately 80% of patients have conjunctival lesions,64,65 mainly manifested by pain, photophobia, lacrimation, redness, and discharge. Severe forms may lead to epithelial defect corneal ulceration, anterior uveitis, and purulent conjunctivitis. Synechiae between eyelids and conjunctiva often occur. There may be shedding of eyelashes (see Fig. 40-4B). Genital erosions are frequent, often overlooked in women, and may lead to synechiae.66
Shedding of nails occurs in severe forms.
EN is associated with high fever, pain, and weakness. Visceral involvement is also possible, particularly with pulmonary and digestive complications. Early pulmonary complications occur in approximately 25% of patients and are essentially manifested by elevated respiratory rate and cough, which should prompt strict surveillance.67,68 Bronchial involvement in EN is not correlated with the extent of skin lesions or with the offending agent. In most cases chest radiographs are normal on admission but can rapidly reveal interstitial lesions that can progress to acute respiratory distress syndrome (ARDS). In all reported cases, when acute respiratory failure developed rapidly after the onset of skin involvement, it was associated with poor prognosis. In the case of respiratory abnormalities, fiberoptic bronchoscopy may be useful to distinguish a specific epithelial detachment in the bronchi from an infectious pneumonitis, which has a much better prognosis.
Gastrointestinal tract involvement is less commonly observed, with epithelial necrosis of the esophagus, small bowel, or colon manifesting as profuse diarrhea with malabsorption, melena, and even colonic perforation.69,70 Renal involvement has been reported. Proteinuria, microalbuminuria, hematuria, and azotemia are not rare. Proximal tubule damage can result from necrosis of tubule cells by the same process that destroys epidermal cells.71 Glomerulonephritis is rare.72
Laboratory Tests
There is no laboratory test to support the diagnosis of EN. Laboratory examinations are essential to evaluation of severity and daily management as for all life-threatening conditions in intensive care units.
Evaluation of respiratory rate and blood oxygenation are among the first steps to take in the emergency room. Any alteration should be checked through measurement of arterial blood gas levels. Serum bicarbonate levels below 20 mM indicate a poor prognosis.14 They usually result from respiratory alkalosis related to the specific involvement of bronchi and more rarely from metabolic acidosis.
Massive transdermal fluid loss is responsible for electrolyte imbalances, hypoalbuminemia, and hypoproteinemia, and mild and transient renal insufficiency and prerenal azotemia are common. Raised blood urea nitrogen level is one marker of severity. Anemia is usual, and mild leukocytosis as well as thrombocytopenia may occur. Neutropenia is often considered to be an unfavorable prognostic factor but is too rare to have a significant impact on SCORTEN. Transient peripheral CD4+ lymphopenia is nearly always seen and is associated with decreased T-cell function. Mild elevation in levels of hepatic enzymes and amylase (most probably of salivary origin) are frequent but without impact on prognosis. A hypercatabolic state is responsible for inhibition of insulin secretion or insulin resistance, which results in hyperglycemia and occasionally overt diabetes. A blood glucose level above 14 mM is one marker of severity.14 Other abnormalities in laboratory values may occur, indicating involvement of other organs and complications such as sepsis.
Skin biopsy for routine histologic and possibly immunofluorescence studies should be strongly considered, especially if there are alternative diagnoses to consider. In the early stages, epidermal involvement is characterized by sparse apoptotic keratinocytes in the suprabasal layers, which rapidly evolves to a full-thickness necrosis and subepidermal detachment (Fig. 40-5
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree