28 Congenital hand IV
Disorders of differentiation and duplication
Synopsis
 Syndactyly is one of the most common congenital differences in the upper extremity and can be classified as incomplete (soft tissue only, not extending to the tip), complete (soft tissue only, extending to the tip), complex (with distal bony union) or complicated (with more than only distal bone fusion).
Syndactyly is one of the most common congenital differences in the upper extremity and can be classified as incomplete (soft tissue only, not extending to the tip), complete (soft tissue only, extending to the tip), complex (with distal bony union) or complicated (with more than only distal bone fusion).
 Timing of surgery depends on the fingers involved and whether the syndactyly is cutaneous or not. In the simple digit 3–4 syndactyly there is no hurry, while in the simple thumb-index syndactyly release is undertaken early. When bony fusion accompanies syndactyly (complex/complicated), these fusions should be separated early to prevent asymmetric growth if the fused fingers have different lengths.
Timing of surgery depends on the fingers involved and whether the syndactyly is cutaneous or not. In the simple digit 3–4 syndactyly there is no hurry, while in the simple thumb-index syndactyly release is undertaken early. When bony fusion accompanies syndactyly (complex/complicated), these fusions should be separated early to prevent asymmetric growth if the fused fingers have different lengths.
 Creating a web and nail fold and adding skin to the inner borders of the digits in complete syndactyly are the three key elements in separating the digits.
Creating a web and nail fold and adding skin to the inner borders of the digits in complete syndactyly are the three key elements in separating the digits.
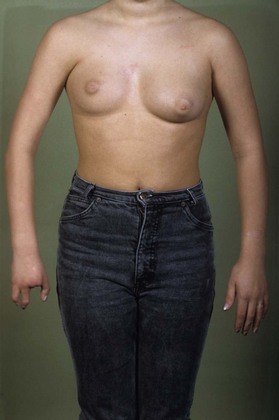
 Poland syndrome is characterized by unilateral absence of the sternocostal head of the pectoralis muscle combined with ipsilateral short and webbed fingers. The central three digits are most affected. It can vary from a smaller hand, simple syndactyly to symbrachydactyly, up to more severe hypoplasia of the entire arm.
Poland syndrome is characterized by unilateral absence of the sternocostal head of the pectoralis muscle combined with ipsilateral short and webbed fingers. The central three digits are most affected. It can vary from a smaller hand, simple syndactyly to symbrachydactyly, up to more severe hypoplasia of the entire arm.
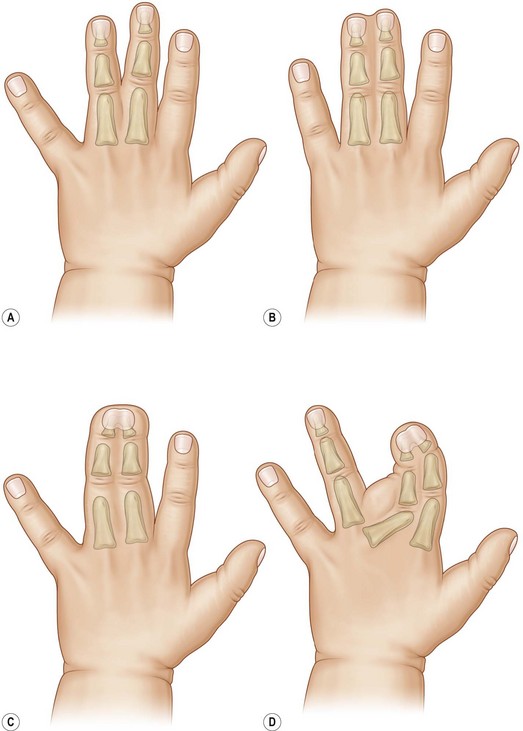
 Apert syndrome (acrocephalosyndactyly) is characterized by craniosynostosis with complex acrosyndactyly of both hands and feet. Common features of both hands in Apert Syndrome are: brachy-clinodactyly of the thumb, complex syndactyly of index/long/ring finger, symbrachyphalangism and simple syndactyly of the fourth web. Three different types of hand malformations can be recognized: the flat, “spade” hand (type I), the constricted cupped, “mitten” hand (type II) and the coalesced “rosebud” hand (type III).
Apert syndrome (acrocephalosyndactyly) is characterized by craniosynostosis with complex acrosyndactyly of both hands and feet. Common features of both hands in Apert Syndrome are: brachy-clinodactyly of the thumb, complex syndactyly of index/long/ring finger, symbrachyphalangism and simple syndactyly of the fourth web. Three different types of hand malformations can be recognized: the flat, “spade” hand (type I), the constricted cupped, “mitten” hand (type II) and the coalesced “rosebud” hand (type III).
 The surgical sequence in correction of Apert syndrome is release of thumb and index or deepening of the first web and separation of digit 4 and 5, followed by separation of the other digits and correction of clinodactyly of the thumb. If present, 4–5 metacarpal synostoses can be separated.
The surgical sequence in correction of Apert syndrome is release of thumb and index or deepening of the first web and separation of digit 4 and 5, followed by separation of the other digits and correction of clinodactyly of the thumb. If present, 4–5 metacarpal synostoses can be separated.
 Symphalangism is a longitudinal bony fusion of the finger and/or toe joints. In hereditary symphalangism, the PIPJ is mostly involved.
Symphalangism is a longitudinal bony fusion of the finger and/or toe joints. In hereditary symphalangism, the PIPJ is mostly involved.
 In metacarpal synostosis, curvature of the epiphysis, discrepancy in length between the two involved metacarpals, and the shape of the bones, will direct the choice of treatment. Surgical treatment in metacarpal synostosis is functional and aesthetic. Consultations are necessary until skeletal maturity because of angulation, length discrepancies and rotation that can occur due to growth.
In metacarpal synostosis, curvature of the epiphysis, discrepancy in length between the two involved metacarpals, and the shape of the bones, will direct the choice of treatment. Surgical treatment in metacarpal synostosis is functional and aesthetic. Consultations are necessary until skeletal maturity because of angulation, length discrepancies and rotation that can occur due to growth.
 Congenital radioulnar synostosis is less common than the post-traumatic version. In most cases of radioulnar synostosis, the proximal third is involved, with bilateral involvement in 60%. It is common in craniofacial hand disorders. Treatment is recommended in patients with a fixed pronation of more than 60° and complaints of disability in daily life.
Congenital radioulnar synostosis is less common than the post-traumatic version. In most cases of radioulnar synostosis, the proximal third is involved, with bilateral involvement in 60%. It is common in craniofacial hand disorders. Treatment is recommended in patients with a fixed pronation of more than 60° and complaints of disability in daily life.
 Polydactyly of the hand can be divided into radial, central (digit 2, 3, and 4), and ulnar polydactyly, referring to the region of the extra digit or part of a digit. It can occur isolated or syndromic. Syndromes are more associated with ulnar polydactyly than radial polydactyly. The most commonly used classification for radial polydactyly is the Wassel classification (also known as the Iowa system). Ulnar polydactyly is either classified into two or three types.
Polydactyly of the hand can be divided into radial, central (digit 2, 3, and 4), and ulnar polydactyly, referring to the region of the extra digit or part of a digit. It can occur isolated or syndromic. Syndromes are more associated with ulnar polydactyly than radial polydactyly. The most commonly used classification for radial polydactyly is the Wassel classification (also known as the Iowa system). Ulnar polydactyly is either classified into two or three types.
 Timing of surgery is arbitrary. Surgery is recommended in the first year of life by many authors, and depends on the severity of the condition. Floating little fingers are often removed early. At the first operation as much correction as possible is performed on both soft tissues and bones. Correct alignment and balancing forces on the joints and bones is crucial. Growth will make insufficiently corrected tissue worse.
Timing of surgery is arbitrary. Surgery is recommended in the first year of life by many authors, and depends on the severity of the condition. Floating little fingers are often removed early. At the first operation as much correction as possible is performed on both soft tissues and bones. Correct alignment and balancing forces on the joints and bones is crucial. Growth will make insufficiently corrected tissue worse.
 Inadequate correction in proximal radial polydactyly leads to complications such as S- and Z-deformities mostly due to imbalance. In distal polydactyly it can lead to nail deformities and broadness of the distal end of the thumb.
Inadequate correction in proximal radial polydactyly leads to complications such as S- and Z-deformities mostly due to imbalance. In distal polydactyly it can lead to nail deformities and broadness of the distal end of the thumb.
 Triphalangeal thumb can vary from a longer thumb with deviation due to the extra phalanx to a nonopposable thumb with an inadequate first web and aberrant muscles and tendons, with the thumb in the same plane as the hand, resembling a five fingered hand. Triphalangeal thumb can be associated with polydactyly, syndactyly, cleft hand and longitudinal ray deficiency (e.g., Holt–Oram syndrome). It occurs isolated or as an autosomal dominant trait.
Triphalangeal thumb can vary from a longer thumb with deviation due to the extra phalanx to a nonopposable thumb with an inadequate first web and aberrant muscles and tendons, with the thumb in the same plane as the hand, resembling a five fingered hand. Triphalangeal thumb can be associated with polydactyly, syndactyly, cleft hand and longitudinal ray deficiency (e.g., Holt–Oram syndrome). It occurs isolated or as an autosomal dominant trait.
 In less complex opposable triphalangeal thumbs, primary surgical strategies are focused on the distal two joints of the “thumb” comprising correction of deviation, reduction of additional length and joint stabilization. In more complex nonopposable triphalangeal thumbs, treatment not only is concentrated on the middle and distal phalanx but also on balancing of the MCPJ and CMCJ, together with reduction of metacarpal length up to formal pollicization. Additional polydactyly and syndactyly, if present, will also need attention.
In less complex opposable triphalangeal thumbs, primary surgical strategies are focused on the distal two joints of the “thumb” comprising correction of deviation, reduction of additional length and joint stabilization. In more complex nonopposable triphalangeal thumbs, treatment not only is concentrated on the middle and distal phalanx but also on balancing of the MCPJ and CMCJ, together with reduction of metacarpal length up to formal pollicization. Additional polydactyly and syndactyly, if present, will also need attention.
 Camptodactyly is a contracture of the PIPJ in the antero-posterior direction (campylo = arched and dactylos = finger). Camptodactyly is mostly sporadic without obvious family history. The most involved finger is the little finger, followed by the ring finger. All fingers can be involved. It can occur in the first year of life and progress further or present during adolescence. Conservative treatment is mostly advocated. Multiple surgical treatment regimens have been proposed varying from full release, tendon transfers and skin grafts to correction osteotomy, arthroplasty and arthrodesis. All techniques have relative merit.
Camptodactyly is a contracture of the PIPJ in the antero-posterior direction (campylo = arched and dactylos = finger). Camptodactyly is mostly sporadic without obvious family history. The most involved finger is the little finger, followed by the ring finger. All fingers can be involved. It can occur in the first year of life and progress further or present during adolescence. Conservative treatment is mostly advocated. Multiple surgical treatment regimens have been proposed varying from full release, tendon transfers and skin grafts to correction osteotomy, arthroplasty and arthrodesis. All techniques have relative merit.
 Clinodactyly is derived from “klineia” (to bend, incline or slope) and “dactylos” (finger, toe) and is used for a deviated finger in a radio-ulnar direction. The deviation is caused by an abnormally shaped bone. The middle phalanx of the little finger and the proximal phalanx of the thumb are the most frequently involved. Treatment can be a closed wedge osteotomy, reversed wedge osteotomy or an opening wedge osteotomy, with or without bone graft or a physiolysis.
Clinodactyly is derived from “klineia” (to bend, incline or slope) and “dactylos” (finger, toe) and is used for a deviated finger in a radio-ulnar direction. The deviation is caused by an abnormally shaped bone. The middle phalanx of the little finger and the proximal phalanx of the thumb are the most frequently involved. Treatment can be a closed wedge osteotomy, reversed wedge osteotomy or an opening wedge osteotomy, with or without bone graft or a physiolysis.
Syndactyly
Introduction
The distal end of the ‘normal’ web lies on the palmar side roughly at the mid-level of the proximal phalanx.1 A more distal web is called syndactyly. Syndactyly is one of the most common congenital hand malformations with an incidence of 1 in 2000 live births. Familial syndactyly is reported in 15–40% of syndactylies.2,3 They are more common in Caucasians than in people from African descent. About 50% of patients have bilateral involvement. Males are more affected than females varying from 46–84%. The incidence of ray involvement in syndactyly is in digit 3–4: 50%; digit 4–5: 30%; digit 2–3: 15% and digit 1–2: 5%.1,2 It can appear isolated or in association with other deformities in the upper or lower extremity or as part of a syndrome (like Poland Syndrome or Apert Syndrome). Syndactyly can be associated with polydactyly and/ or clefting (like in synpolydactyly, Greig syndrome, Oculodentodigital syndrome and cleft hand).
Syndactyly can be classified as incomplete (soft tissue only, not extending to the tip), complete (soft tissue only, extending to the tip), complex (with distal bone union) or complicated (with more than only distal bone fusion) (Fig. 28.1).2 For the first web the terms simple, complex and complicated are used most.
History
In 1801, fingers have already been separated by straight line incisions leaving the wounds to heal by secondary intention. In 1808, Rudtorffer guided a wire from dorsal to ventral between the fingers proximally creating an epithelialized sinus by and then separated the fingers distally from it. In 1810, Zeller used dorsal triangular flaps to reconstruct the defect following separation to create a web. As scarring and necrotic flaps developed from these techniques, Dieffenbach performed a dorsal rectangular flap in 1845. Furthermore, Valpeau reported using stitches to separate the fingers in 1847 and Norton reported using a dorsal and palmar triangular flap in 1881. Thus in the last half of the 19th century already, the basic techniques of flaps for web reconstruction still used today were described. Concerning the further distal separation, Faniel described in 1911, a Z-shaped incision to cover the defects after separation. In 1940, Cronin introduced the zig-zag approach.4
Basic science/disease process
In the developing limb bud, fingers become apparent at day 41–43 and are fully separated at day 53.5–7 Apoptosis is needed for separation of the fingers. This process is mediated by BMP-4 (bone morphogenic protein).8 Current understanding relates these anomalies to differentiation disturbances in the developing hand plate.9
Diagnosis/patient presentation
Syndactyly can be present in a large variety of forms as it is only a descriptive term. The fingers can be normal or anomalous; the number of affected fingers can differ, as well as the nature of involvement (Fig. 28.2).



Fig. 28.2 (A) Nearly complete syndactyly, (B) complex syndactyly radial side and (C) complicated syndactyly.
Complicated syndactyly is characterized by an abnormal bone structure inside the syndactyly with fusions, rudimentary bones, missing bones, abnormal joints and sometimes cross bones.5,10
Patient selection
Timing of surgery depends on the fingers involved and whether the syndactyly is cutaneous or not.
Early indications for surgery are syndactylies between fingers of unequal length; with distal bone fusions; and in complex or complicated acrosyndactyly especially if the thumb is involved. These early indications are to prevent asymmetric growth and/or to create a possibility to grasp.11 In the simple digit 3–4 syndactyly, there is no hurry.
Simple syndactyly release can be performed from 6 months onwards. Most surgeons will operate on these children between 1–2 years to prevent anesthesia problems.12
Treatment/surgical technique
Treatment of syndactyly should not only address the key points of adequate release but also in the least number of operations while minimizing complications.12 Release of syndactyly implicates separation of conjoined skin and subcutaneous tissue preserving integrity of the neurovascular bundles. Furthermore, conjoined ligaments and bands and existing sites of osseous union are divided. On the dorsal side subcutaneous fat can be removed but care has to be taken to prevent damage to the neurovascular bundle. For safety reasons two adjacent complete syndactylous fingers are not separated at the same time as vascular anatomy can be different. In short multiple syndactylous fingers, for instance, dominant digital vessels can only exist on the lateral sides of the conjoined fingers. Sometimes it is necessary to sacrifice one of the vessels in a distal bifurcation. The nerves in these cases can mostly be dissected more proximally. In young children bone or cartilaginous fusions can be separated by knife or osteotome.11
Creation of a web
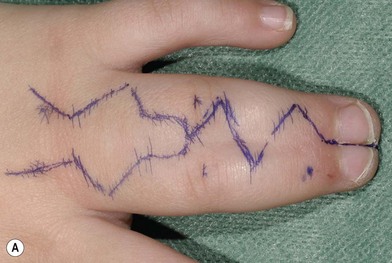
The web in syndactyly can basically be created by a dorsal flap; a palmar flap or a combination of both. These techniques have already been practised in the second half of the 19th century and are still used today. To these techniques have been added flaps with slightly different design or flaps more proximal from the dorsum of the hand.14–19 I use a dorsal clover leaf flap because the wings will cover partly the lateral side of the proximal phalanx and the tip is interdigitated on the palmar side preventing linear scars in the web itself as well as palmarly. In an effort to prevent skin grafts, dorsal metacarpal flaps have been used to create the web, followed by primary closure of the fingers (Fig. 28.3).18–20
For the first web, different kinds of Z-flaps (four flap, double, double opposing, five flap) transposition flaps from the dorsum of the hand and index or thumb are used depending on the width and deepness of the created defect following release. Also pedicled flaps and free flaps have been advocated for the larger defects.21 In the first web, the release of the tight fascia on the first dorsal interosseous muscle in combination with the fascia on the adductor muscle is essential to create a deeper web. Sometimes even the insertion of the adductor muscle is shifted more proximally to open the web.
Upton has published an excellent overview of all the different flaps for web reconstruction.5 For incomplete syndactyly many variations of rotating Z-flaps have been described for web reconstruction (Fig. 28.4).22
Treating the lateral soft tissue defects
In syndactyly, the shortage of skin is very often underestimated. In the regular simple syndactyly, skin shortage is at least 36% of the circumference of the finger which is separated. Cronin has popularized the zig-zag skin separation distal to the flap for web reconstruction.23 The created triangular flaps provide coverage at the PIPJ. The triangular flaps can either be fully or partially interdigitated depending on the extent of the skin shortage. In this way the areas for skin grafting can be diminished and placed on less demanding parts of the fingers. Full thickness skin grafts (FTSG) are mostly used to cover the defects (Fig. 28.5). They can be taken from the groin more laterally to prevent later hair growth on the grafts or from other sites like the inner side of the upper arm or from the cubital fossa. Also thicker split thickness skin grafts (STSG) can be taken from the nonweight bearing part of the sole of the foot. Withey et al. used only STSGs at the proximal base of the inner sides of the released fingers together with a large number of triangular flaps. The remaining defects were left open resulting in good scars.24
Separation of the fingertips
If the nails are separately developed in complete syndactyly, the pulp can be separated and the skin advanced to the rim. If the nails are partly fused with a deep furrow and indentation on the pulp side than simple separation and primary closure is often still possible. If the nails are conjoined, with hardly or no ridge than nail wall reconstruction with flaps is necessary. Buck-Gramcko has introduced the pedicled pulp flaps for nail wall reconstruction from the adjacent finger pulp.25 The disadvantage of these flaps is the sometimes thinner finger tips. Alternatives are the use of a thenar flap, but this has the disadvantage that the finger has to be supple to reach the thenar easily and it is a two-stage procedure.26
Postoperative care
Perioperative paraffin gauze is applied on the wounds and grafts, followed by moist dressings, synthetic cotton, and an elastic bandage. The elbow, forearm and hand are subsequently covered with a longitudinal adhesive bandage to prevent removing the dressing. The general concept among most authors is to perform wound inspection in the first 2 weeks after operation.14,25
Outcomes, prognosis, and complications
Outcome can be related to web creep, scarring, graft take, rotation, deviation and loss of function.
Web creep has been reported to be from 0% to 12% depending on the used techniques, the long-term follow-up, and the variety of included patients. Reoperations have been performed for web creep in up to 8% of patients.20,27–30
With regard to skin grafts, FTSGs have a better skin quality than STSGs; they can also create problems such as graft loss; skin contracture; web creep; hair growth; hyperpigmentation, and hypertrophic scarring.19,25,31–35
Skin contractures in using STSGs are reported to occur in 40%, while this was only 22% when using FTSGs.33 Flexion contractures are reported in a series with long-term follow-up to be 13% and rotation and lateral deviation in 12%.36 Hair growth when using FTSGs from the groin is reported as being 71%.30 Leaving small areas open between numerous triangular flaps seems to result in less scarring and there is no difference in web creep versus the classical approach.24
In a group treated with dorsal metacarpal flaps or extended dorsal interdigital flaps and primary closure, results were better, avoiding all the problems with skin grafts.18–20
Patients should be followed till the end of growth to detect later problems, such as web creep and scar contractures. Redo releases of residual syndactyly is often undertaken, especially at the first web in more complex cases (Fig. 28.6).
Poland syndrome
History
In 1841, Poland37 described cadaver findings as a student demonstrator of anatomy. He reported deficiency of the external oblique muscle, absence of the sternal and costal portion of the major pectoral muscle, as well as absence of the minor pectoral muscle and portions of the serratus magnus muscle. In the ipsilateral shorter hand, all middle phalanges where absent except for the middle finger, with webbing between the proximal phalanges. However, absence of the pectoral muscle without a hand deformity has been described in 1826 by Lallemand and Froriep was the first to point out the combination of absence of the pectoralis muscle together with ipsilateral syndactyly in 1839.38
Basic science/disease process
Several mechanisms in the pathogenesis of Poland syndrome have been described. Despite some familial occurrence, no inheritance patterns have been determined. The most prevailing theory focuses on the interruption of blood supply to the limb bud in the 6th week of gestation. The interruption will cause hypoplasia to the ipsilateral subclavian artery or one of the branches39,40 determining the diversity of the defect.
Diagnosis/patient presentation
In Poland syndrome, patients present with a broad range of ipsilateral trunk, upper limb and hand anomalies. The classical presentation comprises a combination of absence of the sternocostal portion of the pectoral major muscle, hypoplastic arm and a hypoplastic hand with a simple syndactyly usually of all web spaces (Fig. 28.7). The thoracic deformities might range from the classical absence to complete hypoplastic shoulder girdle with involvement of the ribs and nipple, scoliosis, and seldom dextrocardia.41,42 Furthermore, Poland syndrome can be associated with multiple other malformations, ranging from craniofacial, internal organs to the lower extremity.43,44
Treatment/surgical technique
Because of the wide scope in presentation of the syndactyly and symbrachydactyly, several treatment options are possible (see Chapters 27 and 29). Reconstruction of the breast, deficient muscle contour or chest wall deformity is beyond the scope of this chapter.
Outcomes, prognosis, and complications
Outcome is very much related to the original defect and the reconstruction used.
In syndactylous hypoplastic fingers, the separated individual fingers can be less functional than before the operation, resulting in poor outcome. Normally, similar outcome and complications occur as in syndactyly and symbrachydactyly. For prognosis and complications on nonvascularized and vascularized toe transfers, see Chapters 14 and 27.
Apert syndrome
Introduction
The birth prevalence of Apert syndrome ranges from 7.6 to 22.3 per million live births, the lowest incidence being in Hispanics and the highest in Asians. Males and females are equally affected.45 In the author’s series, the male to female ratio was 1.5 : 1.
History
Apert, a French physician in Paris described nine collected cases in 1906, but probably Wheaton was the first to describe it in 1894.46,47
Basic science/disease process
Apert syndrome is caused by a mutation in the gene encoding fibroblast growth factor receptor-2 (FGFR 2). The gene map locus is 10q26. Two mutations are well recognized and are related to substitutions at two amino acid positions P253R and S252W in FGFR 2. The more severe type of Apert hand is mostly related to the P253R mutation. In our series, nearly all type III Apert hands were attributed to this mutation. Most cases are sporadic, but autosomal dominant inheritance has been reported.48,49
Diagnosis/patient presentation
In the Apert syndrome child, the level of function depends more on their intellectual capacities than the severity of extremity involvement. Most Apert children are capable of self-care over 5 years of age. Regarding the upper extremity, motion of the shoulder is not normal and decreases with age. In the older Apert patient, a marked deltoid muscular atrophy is often encountered. They appear to have anterior subluxation of the humeral head.50 The elbow deformities can differ more extensively between these patients than at the shoulder. Elbow function can be slightly decreased but mostly do not worsen over the years.50
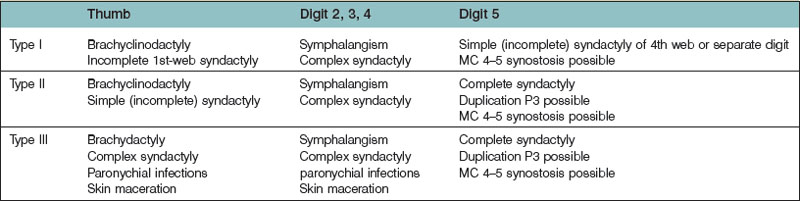
Upton has classified the Apert syndrome hand into type I, II, and III for ease of clinical decision-making (Table 28.1). In the type I hand (“spade” hand), there is a radially deviated small thumb with a shallow first web. The index, long, and ring fingers display complete or complex syndactyly. The little finger is attached by a simple complete or incomplete syndactyly and can mostly move at the DIPJ. The MPJs have adequate range of motion. In the type II hand (“mitten” or “spoon” hand), the thumb is radially deviated and has an incomplete or complete simple syndactyly with the index. The index, long, and ring fingers are distally fused, creating a curve in the palm with divergent metacarpals. The little finger is attached to the ring with a mostly complete but simple syndactyly.
In the type III hand (‘rosebud’ hand) the thumb, index, long, and ring are distally fused either cartilaginous or bony attachments. The thumb can be very difficult to identify separately from the index. The little finger is united to the ring by simple complete syndactyly. The nails can be confluent or have ridges indicating the distal finger underneath. Proximal synostosis at the base of the fourth to fifth metacarpal can be present, as well as carpal fusions.51 In our series of 66 patients the ratio of type III:type II:type I hand was 4 : 3 : 3; although Upton reports that type III is the most uncommon.
Up to 7% ulnar polydactyly has been reported.52 In the author’s series, there is one case of a duplicated distal phalanx of the index and two cases of duplication at the little finger (5%). In the type III hand, finger nails growing through surrounding skin causing frequent paronychial infections is frequently seen.
The flexion creases are often absent. Dimples on the dorsum indicate the metacarpophalangeal joints (MPJs). Distal to the MPJs, neurovascular structures can vary considerably in branching, or are absent. Distal in the hand, tendons can have a different shape and course. Regarding the thumb, adduction, palmar abduction, and flexion are always present. The first dorsal interosseous is hypertrophic and fan shaped extending to the delta phalanx of the thumb in the more severe types. The abductor pollicis brevis muscle (APB) is anomalous as it inserts into the radial aspect of the distal phalanx of the thumb causing radial deviation.53 Lumbricals if present act as MPJ flexors. The hypothenar muscles are present and normal.
The proximal phalanx of the thumb is abnormal and triangular shaped. The IPJ and the CMCJ have little motion, while the MPJ is mobile. With skeletal maturity the IPJ fuses after first being segmented. The distal phalanx and nail matrix are broad.54,55
Patient selection
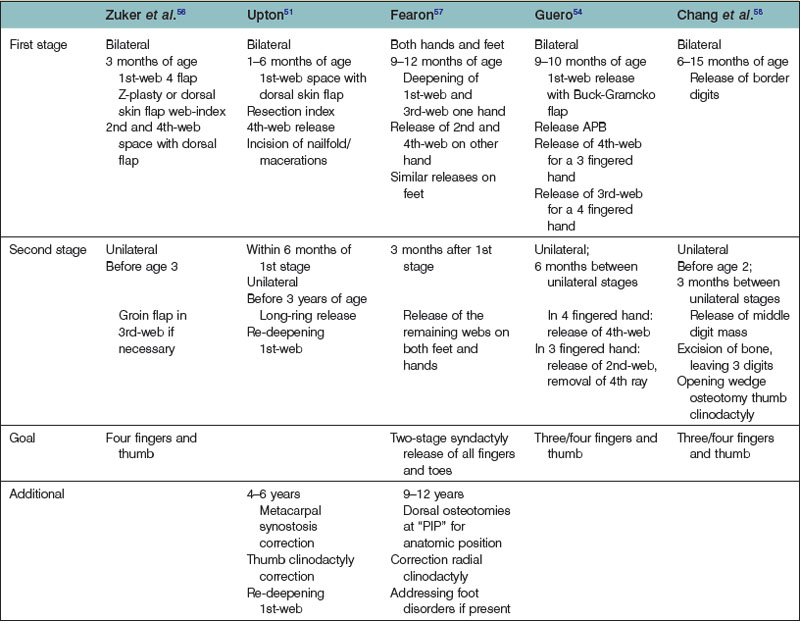
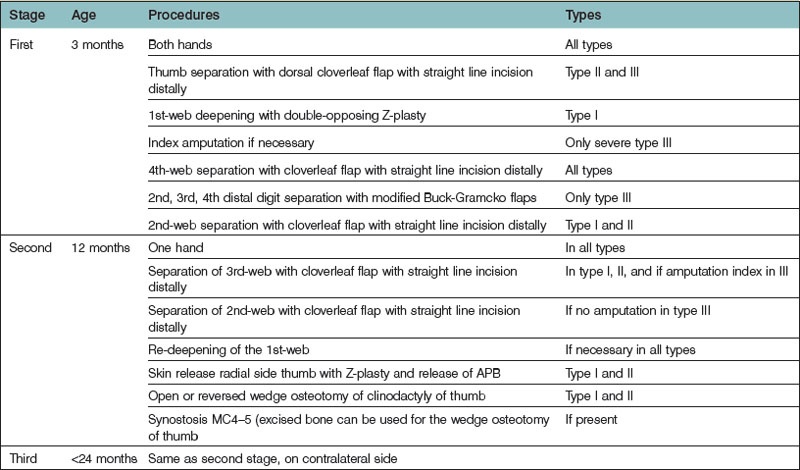
Many articles have been published on treatment timing in Apert syndrome.51,54,56–58 Most philosophies try to diminish the number of operations by releasing as many fingers as possible in one session. The way this is accomplished varies among authors (Table 28.2).
Treatment/surgical technique
Separation of thumb and fingers, correction of thumbs and mobilization of the little finger in as few operations as possible is the surgical goal. The author’s preferred method is illustrated in Table 28.3 and Figures 28.8 and 28.9.
Separation of fingers
The residual defects are covered with skin grafts. Chang only used local flaps and skin grafts, while Zuker et al. and Kay use groin flaps for the central digits and the first web, respectively.21,56,58 Often further corrections are necessary to deepen webs.
Habenicht uses small external fixators to transversely distract the complicated and complex syndactyly of the central fingers, with separation of the distal bone fusions. The created skin is used for coverage of the defects instead of skin grafts. Other methods such as silastic sheets and tissue expanders to separate fingers have been discarded.59
Thumb and first web
A well separated thumb is crucial in these hands. In a shallow first web (in the type I hand), a 4- or 5-flap Z-plasty can be utilized. In a complete or nearly complete syndactyly (in the type II hand), a large dorsal flap is used to create a first web.60 Tight fascia around the adductor muscle is released to open up the first web.
Preferably, a hand with four fingers and a thumb is created. In the type III hand however, it can be necessary to sacrifice the index to create a useful first web with a dorsal flap.61,62
Dao et al. considered the abnormal radiodistal insertion of the APB responsible for the deviation of the thumb, and released the APB muscle and tendon distally without performing a corrective osteotomy.53 In the type III hand, the thumb is short and has less bone volume distally.
Outcomes, prognosis, and complications
Complications
The hyperhidrosis and oily skin makes the skin grafts prone to maceration, skin slough and even infection. Barot and Caplan reported a 22% partial skin graft loss.63 Guero operates on these children in winter, to diminish sweltering bandages and casts.54 Secondary procedures for web contractures are therefore common. The revision rate for secondary web contracture varies among authors from 3–18%.54,57,58,63 In the author’s series, there has been 13% secondary contracture release. Revising web contractures depends very much on the surgeon’s idea of contracture. Patients rarely complain of web contractures. The author tends to deepen the first web extra if a syndactyly release of fingers is planned. Other described interventions are amputation of a finger due to limited opening of the first web space or because of ankylosis.54
Secondary procedures
• Web deepening with advancing of the primary flap or skin grafting the newly created defect
• Wedge osteotomies of the border digits as necessary to correct the deviation following separation due to partial closure of the epiphyseal plate
• Extra thumb lengthening is sometimes requested in very short thumbs in type III hands.
Synostosis
Introduction
Symphalangism was first described by Cushing as an autosomal dominant genetic skeletal disorder64 and is characterized by longitudinal bone fusions along the finger and toe joints. Most commonly, the PIPJ is fused. Associated bone fusions are carpal or tarsal synostosis, and stapes fixation resulting in conductive deafness. Flatt and Wood65 classified the congenital difference as true symphalangism with normal length of digits; with symphalangism in symbrachydactyly; or associated with other anomalies (i.e., Apert or Poland). The incidence of true symphalangism is 0.03–4%.60 Because of the conjunction with other conditions, the general incidence of all types of symphalangism is not known.
Metacarpal synostosis is a rare congenital anomaly, with wide anatomical variations. The fourth and fifth metacarpals are usually affected. The synostosis is more common in patients with a craniofacial and hand difference. Incidences in a large group of congenital hand anomalies range from 0.02%66 to 0.07%.67 Buck-Gramcko and Wood distinguished three groups based on the length of fusion: type I, fusion at the base; type II, fusion of about half; type III, more than half; IIIa separated MCPJ, and IIIb common MCPJ.67 A classification, useful for treatment, has been proposed by Foucher et al.68 It comprises the shape of the synostosis, the growth direction of the epiphysis, the deformity of the finger distal from the synostosis, the webbing, and the hypoplasia of the metacarpal bone.
Carpal coalitions are reported rarely, and often go unnoticed. All combinations of carpal fusions have been mentioned, with the most frequent synostosis being between the triquetrum and lunate, and the hamate and capitate.69,70 In a predominantly white population, an incidence with a range of 0.07–0.1% has been mentioned,71,72 compared with 8% in a Nigerian population. Despite the fact that coalition will theoretically impair the movement of the wrist, no disabilities have been described.
Radioulnar synostosis is a rare upper limb malformation and is defined as a fusion of the proximal ends of the radius and ulna, which will prohibit normal rotational movement of the radius around the ulna. Radioulnar synostosis can be unilateral or bilateral (60%), of autosomal dominant inheritance, or associated with other congenital differences. In one-third of cases syndromes and anomalies are listed.5,73,74
History
The term symphalangism was used by Cushing in 1916,64 describing a family with dominant inherited ankylosis of the PIPJs of the hand. One year later, Drinkwater reported the anomaly as “Talbot fingers”, because of the digital anomaly in the Talbot family in England in 14 generations. Today, the term ‘symphalangism’ is used in isolated finger deformities as well as in concurrent anomalies or syndromes.
Metacarpal synostosis was recognized and illustrated by Kelikian,75 and is known throughout history by several names, such as fifth ray anomaly, congenital metacarpal malformation, absent fifth metacarpal, bilateral ulnar thumbs, and congenital fusion.
Radio-ulnar synostosis was first described by Sandifort in 1793, and in 1932, Fahlstrom76 reviewed 185 reported cases since the first description.
Basic science/disease process
Mutations in genes involved in limb development and mutations in the Noggin gene (NOG) have been associated with synostosis. An interruption of apoptosis responsible for the segmentation is believed to be the most common cause for synostosis. The gene responsible for the hereditary form of symphalangism (SYM or SYM1) is the NOG, which maps to human chromosome 17 (17q21–q22).77 Mutations in HOXA11 are associated with radioulnar synostosis.
Diagnosis/patient presentation
In metacarpal synostosis, the most common fusion is between the fourth and fifth metacarpals (Fig. 28.10A). A short and abducted little finger is seen in these cases. However, the extent of deformity is dependent on the plane of the joint space and the configuration of the epiphysis of the involved metacarpal heads. A radiograph will give insight into the skeletal abnormality and will guide in the abnormalities of soft tissue alignment.

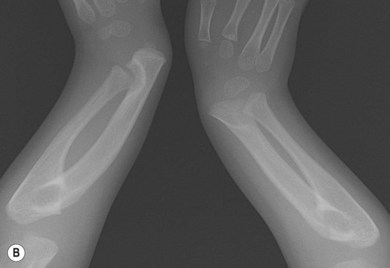
Fig. 28.10 (A) X-ray of metacarpal 4–5 synostosis. (B) X-ray of bilateral carpal and radioulnar. synostosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree