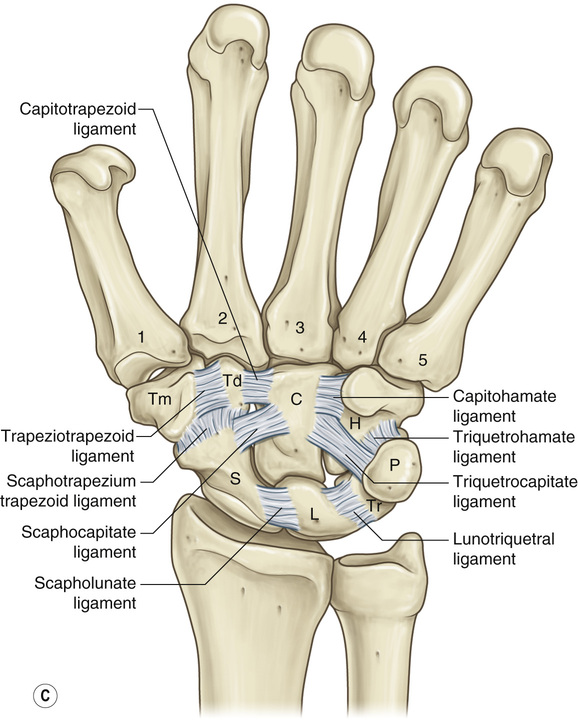
1. The distal radioulnar joint (DRUJ) allows for supination and pronation of the hand. 2. The proximal carpal row consists of the scaphoid, lunate, triquetrum, and pisiform and allows for wrist extension, flexion, and radial/ulnar deviation. • The proximal row articulates primarily with the distal radius through the scaphoid and lunate. 3. The distal carpal row consists of the trapezium, trapezoid, capitate, and hamate and forms the fixed unit of the hand along with the second and third metacarpals (see Figure 18.1). 4. The extrinsic carpal ligaments help to anchor the proximal row with the distal radius and ulna. 5. The intrinsic carpal ligaments are strong structures that link the carpal bones together, and/or the carpal rows together. The two most important intrinsic carpal ligaments are the scapholunate (SL) ligament and the lunotriquetral (LT) ligament. Disruptions of these ligaments lead to carpal instability. • The SL ligament allows synchronous motion of the scaphoid and lunate • The LT ligament anchors the lunate and triquetrum together and allows less motion than the SL ligament (see Figure 18.2). 7. The ulna should complete the smooth curve of the articular surface of the radius. The relationship of the ulna to this imaginary curve is called ulnar variance. • Ulnar positive variance: The ulna extends distal to this imaginary curve. ▪ Associated with ulnar impaction syndrome (ulnar-sided wrist pain) • Ulnar negative variance: The ulna is short of this imaginary curve. ▪ Associated with Kienböck’s disease (avascular necrosis of the lunate) 8. Gilula’s lines: Imaginary curves within the carpus that indicate normal extracarpal and intracarpal architecture (see Figure 18.3). • Disruptions of these lines suggest ligamentous or bony carpal abnormalities. • Results from an injury to, or tear of, the SL ligament or scaphoid fracture • Characterized by pain and swelling over the radial dorsal wrist with widening of the gap between the scaphoid and lunate on plain X ray (“Terry Thomas” sign) ▪ Must compare with unaffected hand ▪ A gap >2 mm is suggestive of an injury. • Disrupts the synchrony between the scaphoid and lunate, allowing the scaphoid to flex and lunate to extend ▪ Immobilization for 3 to 4 weeks is generally acceptable for partial tears ▪ For chronic SL injuries, severe arthritis can develop, creating an SL advanced collapse (SLAC) wrist deformity. • Disrupts the synchrony of the lunate and triquetrum, allowing the lunate to flex with the scaphoid ▪ A VISI (volar intercalated segment instability) deformity develops as the lunate tilts volarly. • Caused by wrist hyperextension and supination with ligamentous injuries around the lunate, which progress from radial to ulnar • Can also develop with scaphoid fracture and/or other carpal fractures (see Figures 18.4 and 18.5) • Follows a natural progression of injury around the lunate complex ▪ Mayfield classification (see Figure 18.6) • The most common fracture of the human skeleton • Often caused by a fall onto an outstretched hand • Characterized by pain, swelling, limited motion, and gross deformity of the wrist ▪ Open reduction internal fixation (ORIF) ○ Most commonly performed with volar locking plates • Extensor pollicis longus (EPL) tendon rupture can occur after distal radius fracture. ▪ Secondary to attrition through disruption of tendon vascularity ▪ Treated with extensor indicis proprius tendon transfer • The most common carpal fracture • The scaphoid can be divided into three segments: Distal pole, waist, and proximal pole ▪ Single, dominant, vascular supply that enters the distal pole and travels retrograde to supply the proximal pole via the dorsal carpal branch of the radial artery • Scaphoid fractures are often caused by a fall onto an outstretched hand. • Characterized by pain in the anatomic snuff box • Fractures may not be visualized on initial plain radiographs ▪ Long arm thumb spica cast immobilization for 6 to 8 weeks ○ Indicated for nondisplaced, distal pole fractures ○ For proximal pole fractures, immobilization is often recommended for 6 months. ▪ ORIF ○ Often performed with compression screw fixation (see Table 18.1) Table 18.1 Algorithm for Acute Scaphoid Fracture Management • Long arm thumb spica cast for 6 weeks, short arm cast for 6 weeks or until CT confirmed healing • Lateral intrascaphoid angle >35 degrees • Perilunate fracture/dislocation
Carpal Injuries and Hand Arthritis
Carpal Anatomy

Common Carpal Ligament Injuries
Common Wrist/Carpal Fractures
Type of Fracture
Treatment
Stable Fractures, Nondisplaced
Tubercle fracture
Short arm cast for 6 to 8 weeks
Distal third fracture/incomplete fracture
Short arm cast for 6 to 8 weeks
Waist fracture
Proximal pole fracture, nondisplaced
Percutaneous or open internal fixation
Unstable Fractures
Dorsal percutaneous/open screw fixation ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Carpal Injuries and Hand Arthritis
Chapter 18