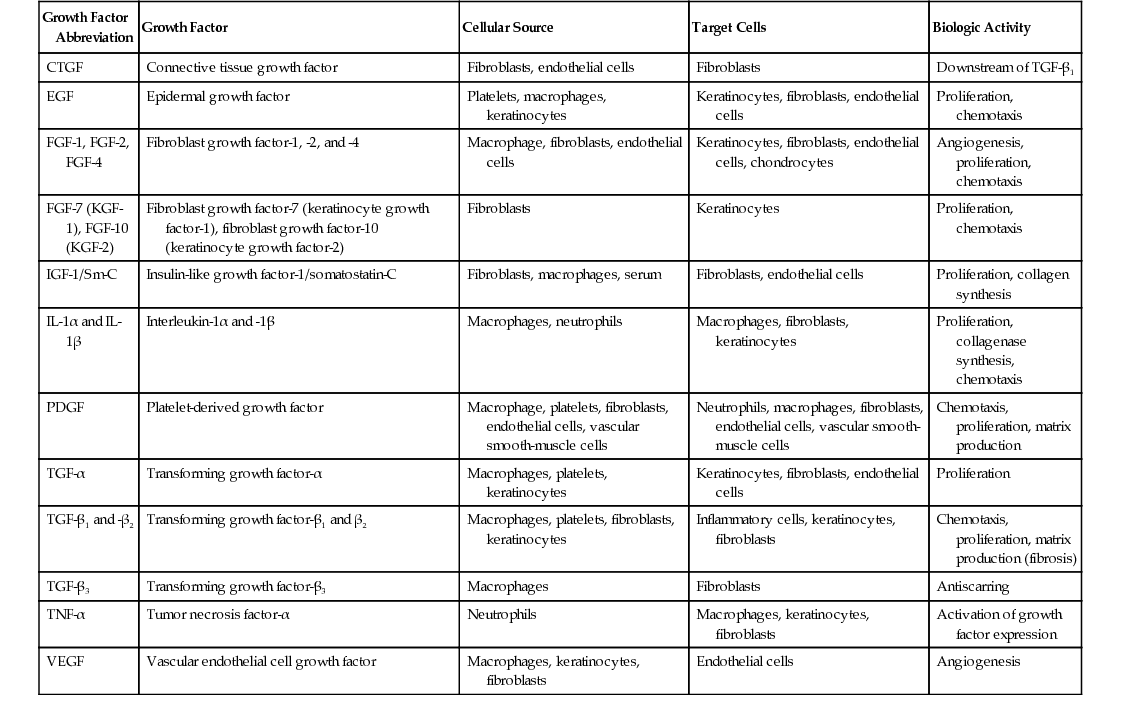
• Inflammatory: Activated to cleanse and prepare wound for healing ▪ Polymorphonuclear (PMN) leukocytes: Initial 24 to 48 hours. Act as defensive units, phagocytosing bacteria and foreign debris from the wound to prevent infection ○ Phagocytosed by macrophages and destroyed • Proliferative/fibroplastic: 3 to 5 days after injury, fibroblasts migrate into the wound and become predominant cell type. They begin to lay down new collagen. At first, type 3 is greater than type 1 but is eventually replaced by type 1 to the normal ratio (4:1, T1:T3). ▪ It is during this time that the greatest rate of collagen synthesis occurs in the wound. ▪ Contraction begins and continues into remodeling phase. • Remodeling begins day 21. Cross-linking and organization of collagen fibers (procollagen is cleaved into collagen) ▪ Net amount of collagen is constant because there is an equal amount of degradation and synthesis. ▪ Wound becomes stronger because of cross-linking. ○ Maximum tensile strength is achieved after ~12 weeks. • Epithelial cell migration: Initiated by loss of contact inhibition and occurs from the periphery of the wound and adnexal structures ▪ Cell division occurs in 48 to 72 hours, resulting in a thin epithelial cell bridge across the wound. ▪ Epidermal growth factors play a key role. ▪ Can be delayed by retinoids (Accutane/isotretinoin) ▪ Can be stimulated by tretinoin (Retin-A) • Myofibroblasts: Involved in wound contraction and play no role in epithelialization • Collagen deposition is seen in the remodeling phase of wound healing. 3. Growth factors involved in wound healing process (see Table 20.1) 4. Important nutrients for wound healing • Vitamin C: Collagen cross-linking via the hydroxylation of proline and lysine to hydroxyproline and hydroxylysine, respectively ▪ Lack of cross-linking results in impaired collagen synthesis and a decrease in collagen tensile strength. Collagen-containing tissues, such as skin, dentition, bone, and blood vessels, are therefore affected, leading to the development of scurvy. • Folate and vitamin B6 (pyridoxine) are integral in DNA synthesis and cellular proliferation. • Vitamin A is an essential factor in epithelialization and fibroblast proliferation. • Vitamin E is a strong antioxidant and immune modulator. • Zinc is one of the most important micronutrients because it acts as a cofactor for numerous metalloenzymes and proteins. ▪ Essential for proper protein (like collagen) and nucleic acid synthesis ▪ Exact mechanism of action unknown ▪ Most widely accepted hypothesis is that there is an increase in hydration resulting from occlusion ▪ To be effective, it must be worn for at least 12 hours/day for 3 months or longer. 5. Systemic factors affecting wound healing (see Table 20.2) Table 20.2 Factors that May Impair Normal Healing and Lead to Chronic Nonhealing Wounds
Wound Healing and Tissue Expansion
Etiopathology
Examples
Vascular
Arterial
Arteriosclerosis, arterial aneurysm, fat embolism with arterial obstruction, hypertension (Martorell ulcer)
Lymphatic
Lymphatic edema, lymphangiodysplasia
Venous
Chronic venous insufficiency, necrotizing thrombophlebitis
Mixed arteriovenous
Combined arteriosclerosis with venous insufficiency, arteriovenous malformations/dysplasia; steal phenomenon (e.g., arteriovenous shunts, vascular compression/obstruction; due to tumors, enlarged lymphatic nodes, etc.)
Vasculitis
Wegener’s granulomatosis, Churg-Strauss vasculitis, Henoch-Schönlein purpura, Sneddon syndrome, systemic lupus erythematosus, rheumatoid arthritis, Felty syndrome, Takayasu arteriitis, polyarteritis nodosa, Kawasaki syndrome, pyoderma gangrenosum, necrobiosis lipoidica diabeticorum, thromboangiitis obliterans (Buerger’s disease), allergic reactions
Vasculopathic syndromes
Raynaud’s syndrome, systemic scleroderma, CREST, Klippel-Trenaunay syndrome, proteus syndrome, CLOVES syndrome, Kasabach-Merritt syndrome
Physical, chemical, and biological causes
Pressure
Immobility, intra- and postoperative bedding, tight shoes and casts, compression therapy
Trauma
Lacerations, any type of soft-tissue and bone injury, vascular rupture
Thermal
Burns/frostbite, electrical injury (electrical current/high voltage/lightning)
Radiation
Radiation therapy
Chemical-toxic
Extravasation, chemical burns (acids/bases), sclerotherapy
Infections
Erysipelas, necrotizing fasciitis, septic cutaneous embolism, osteomyelitis, complications after cutaneous infection
Herpes simplex, cytomegalovirus, human immunodeficiency virus, syphilis, leprosy, tuberculosis
Tropical ulcers, parasitic and vermicular infections
Neuropathic
Posttraumatic
Spinal lesions with palsy, peripheral nerve injury
Congenital
Spina bifida, syringomyelia, multiple sclerosis, neurological syndromes
Systemic neuropathic diseases
Diabetes mellitus, ethylene oxide toxic neuropathy, degenerative central and peripheral neuropathies
Poliomyelitis, leprosy, tabes dorsalis
Hemopathological
Systemic diseases
Polycythemia vera, sickle-cell anemia, other anemias, thalassemia, thrombocythemia vera, thrombocytopenic purpura, increased blood viscosity (paraneoplastic, paraproteinemia, hyperglobulinemia, leukemia), complication after blood transfusion
Disturbed hemostasiology
Factor V Leiden syndrome, antiphospholipid syndrome, disturbed fibrinolysis, factor-XIII deficiency syndrome, antithrombin-III deficiency, proteins C and S deficiency, Marcumar necrosis, disseminated intravascular coagulation, necrosis due to vitamin K antagonist therapy
Neoplastic diseases
Cutaneous tumors
Basal and squamous cell carcinoma, melanoma, Bowen syndrome, Marjolin ulcer (scar carcinoma), tumors with cutaneous metastasis or penetration (e.g., Paget syndrome)
Therapeutic modalities
Steroids, vaccination ulcer (BCG), cytostatic drugs, NSAIDs, extravasation of various drugs
Systemic diseases
Hepatic and/or renal insufficiency, immunosuppression, sarcoidosis, homocysteinemia, hemochromatosis
Other causes
Alcoholism, obesity, gout, smoking, advanced age, malnutrition (e.g., vitamin, protein, and micronutrient deficiency; scurvy); psychiatric diseases with self-harming, neglect, intravenous drug abuse; foreign bodies/projectiles with fistulas ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Wound Healing and Tissue Expansion
Chapter 20