■ Incisional biopsies are sometimes necessary for large lesions, especially in cosmetically sensitive areas. Such a biopsy approach does not always reflect the full primary tumor microstaging of the lesion, including margin assessment, and such limitations need to be considered during definitive treatment.
■ Shave biopsies are not generally recommended when a cutaneous lesion is suspicious for melanoma, because the full extent of the lesion (especially Breslow thickness) may not be included in the biopsy and the approach may limit accurate microstaging of the primary tumor.
■ Confirmation of the melanoma biopsy site(s) must be performed prior to any planned definitive treatment.
Histopathologic microstaging of primary melanoma
■ In order to determine the appropriate extent of surgery for a patient with a primary melanoma—including WE margin and whether to offer/perform intraoperative lymphatic mapping and SNB—assessment of several of the primary tumor’s histopathologic features is essential.
■ Breslow thickness (in millimeters), mitotic rate (expressed in mitoses/mm2), presence or absence of primary tumor ulceration, and the biopsy margin status (peripheral and deep margins) are all essential to define T stage and to guide appropriate surgical therapy; they should be assessed by a dermatopathologist. Additional primary tumor information that may be useful to the operative surgeon includes the presence or absence of lymphovascular invasion, neurovascular invasion, regression, extent of tumor-infiltrating lymphocytes, histologic subtype, and Clark level.
Margins of excision
■ WE includes a radial margin of skin and underlying subcutaneous tissue, with margins appropriate for tumor thickness.
■ The radial margin chosen for the WE is based on the primary tumor (Breslow) thickness. At least five prospective randomized trials conducted over the past three decades informed an evidence-based approach. Although detailed discussion is beyond the scope of this section, the recommendations from the National Comprehensive Cancer Network (NCCN) for the radial margin are as follows:5
■ Melanoma in situ: 0.5–cm margin (Note: For large diameter melanoma in situ, for example, lentigo maligna type, margins >0.5 cm may sometimes be considered to adequately treat occult early invasive disease).
■ Less than or equal to 1.0 mm: 1.0 cm
■ 1.01 to 2.0 mm: 1.0 to 2.0 cm
■ 2.01 to 4.0 mm: 2.0 cm
■ Greater than 4.0: 2.0 cm
Positioning
General positioning strategies
■ Depending on primary tumor characteristics and other considerations, lymphatic mapping and SNB are most often performed in the same operative setting as a WE. For this reason, proper patient positioning should account for both the location of the primary melanoma and the location(s) of draining regional nodal basins. This may become challenging when the primary melanoma drains to multiple nodal basins and/or to interval, ectopic, and/or in-transit sites. Skin graft donor sites or other reconstructive issues must also be considered when positioning the patient.
Proximal extremity
■ For proximal upper extremity lesions, a supine position is generally appropriate for WE and SNB. For more posterior lesions near the shoulder, a modified supine position using a shoulder roll or a lateral decubitus position provides easy access for WE and closure. The arm, prepped circumferentially, should be supported to prevent injury to the brachial plexus and/or shoulder.
■ For proximal lower extremity lesions, the supine position provides excellent exposure of anterior or lateral sites, allowing both WE and SNB. When the melanoma is on the posterior proximal leg or the buttock, the WE may be performed with the patient in the lateral or prone position. Pressure points need to be padded and axillary and chest rolls need to be appropriately positioned. Some surgeons are comfortable performing both WE and inguinal SNB in the lateral position; a potential advantage is that repositioning is not required. Alternately, SNB can be performed in the supine position, and the patient repositioned for the WE.
Distal extremity
■ In general, a supine position is appropriate for most distal extremity lesions. If SNB is also to be performed, access to the axillary, epitrochlear, and inguinal nodal basins is readily achieved. If a patient’s melanoma drains to the popliteal nodal basin, then an alternative position other than the supine approach should be used. The prone position is sometimes used so as to allow the sentinel node to be removed through an incision that could be incorporated into a full popliteal node dissection incision if evidence of metastasis were to be identified.
■ Heel melanomas not only have the potential to drain to the popliteal basin but may also require specialized reconstructive approaches (e.g., wound vac device, rotational flaps, and/or vascularized free flaps). In this situation, use of a beanbag on the operating room table allows for repositioning as indicated.
Truncal sites
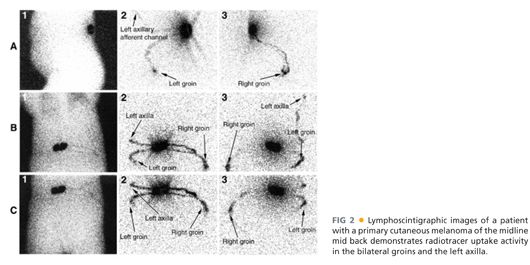
■ When an SNB is performed with WE of a truncal melanoma, the possibility of multiple nodal basin drainage patterns must be considered when devising an operating room positioning strategy. A preoperative lymphoscintigraphy will demonstrate afferent lymphatic drainage patterns to major and unusually situated (e.g., ectopic, interval) nodal basins.
■ For most anterior truncal melanomas (e.g., chest and abdomen), the supine position allows for access to the primary and draining regional nodal basins. For lateral truncal melanomas, ideal positioning for the WE may include placing the patient in a partial or formal lateral position (with appropriate padding and brachial plexus protection).
■ When performing a WE only (e.g., for a thin melanoma without adverse risk features), back melanomas may be performed in the prone (e.g., for medial lesions) or lateral (e.g., for most back lesions) position at the discretion of the surgeon. Appropriate padding and brachial nerve protection must be employed and airway protection is essential. If SNB is being performed in the same operative setting, patient positioning must foster access to draining nodal basins including multiple and/or unusually situated nodal basins. It may be necessary to reposition the patient after the SNB and before the WE (FIGS 2 and 3).


Head and neck sites
■ Head and neck melanoma patients must also be carefully positioned with consideration of the WE, reconstructive requirements, and in continuity access to draining regional nodal basins if SNB is to be performed. Whether in a supine, prone, or lateral position, the head and neck must be appropriately supported and padded. Additionally, the airway, eyes, and ears must be protected.
TECHNIQUES
WIDE EXCISION MARGIN
■ The planned margin of excision of the primary melanoma is based on the Breslow tumor thickness as described above and refers to the radial margin of normal-appearing skin to be resected. If the primary melanoma is entirely or partially intact, the margin should be measured from the periphery of the visible lesion. When the entire pigmented lesion has been excised by the previous biopsy, the margin should be measured from the periphery of the biopsy scar.
PLACEMENT AND ORIENTATION OF INCISION
■ Proper planning of the incision is critical. The surgeon must consider the required radial margin (i.e., margin of excision), the specific anatomic primary site involved, as well as the quality and quantity of local soft tissue.
■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








