Fig. 8.1
After general anesthesia with a double-lumen endotracheal tube, the patient is placed in a half-sitting position with both arms abducted to 90°, and ribs 2 through 4 are identified. A 1-cm stab incision is then performed at third intercostal space, along the midclavicular line for male patients (a) and along the anterior axillary line for female patients (b), in order to hide the postoperative scar as much as possible
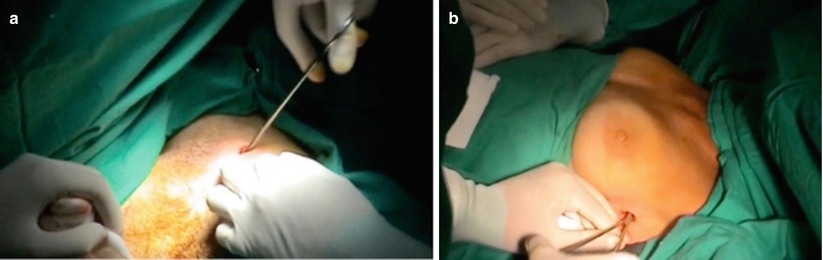
Fig. 8.2
Subcutaneous tissues are undermined through the cutaneous incision, as shown in a male (a) and a female (b) patient, in order to reach the intercostal plane at the third intercostal space. It is important during both undermining and further insertion of the endoscope that the instruments always be kept upon the upper edge of the rib, in order to avoid the neurovascular bundle located just under the surface of the lower edge of the rib

Fig. 8.3
After selective mechanical deflation and collapse of the ipsilateral lung, a 9-mm trocar with an air/insufflator/suction triple valve is inserted through the previously created incision at the third intercostal space on the left side of the patient, always keeping it on the surface of the upper edge of the rib to avoid the vascular bundle
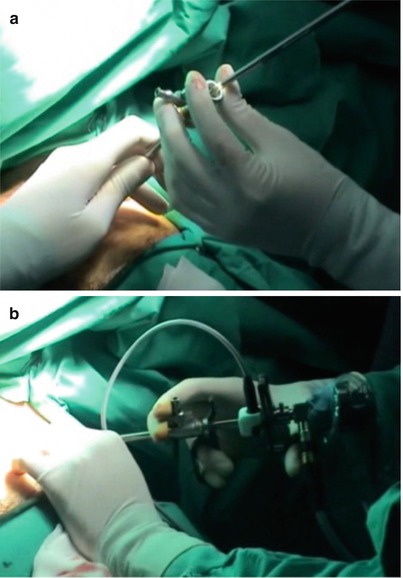
Fig. 8.4
After trocar insertion and creation of an artificial ipsilateral apical pneumothorax, a specifically designed thoracoscope (shown in Fig. 8.5) is guided through the trocar (a) down into the pleural cavity (b). From this point on, the entire procedure is displayed on the external monitor
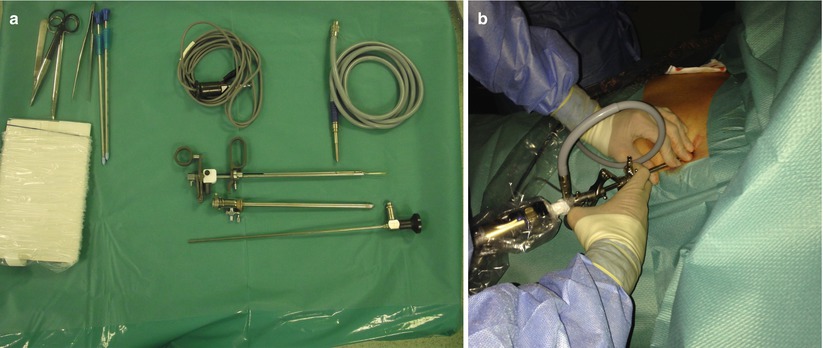
Fig. 8.5
(a) The modified thoracoscope (Karl Storz; Tuttlingen, Germany) consists of a 9-mm trocar with air/insufflator/suction triple valve, a straight Hopkins telescope with fiber-light transmission, a Wittmöser operating sheath with a connection for high-frequency diathermy, and a specifically designed triangle-tipped wire loop electrode for the electrocautery. (b) The thoracoscope enters the pleural cavity through the previously performed incision (third intercostal space) while the patient trunk is positioned at 45°
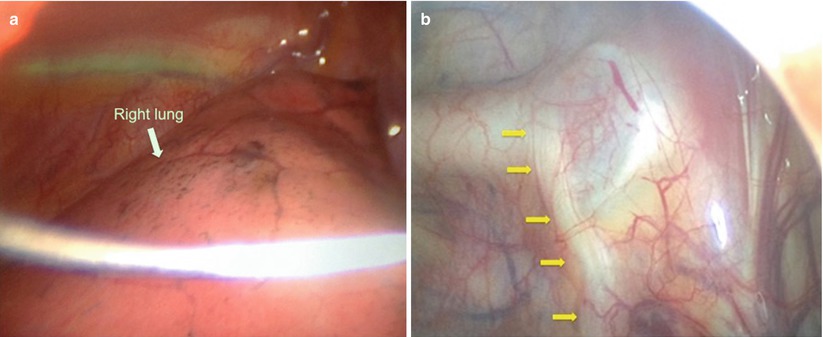
Fig. 8.6
(a) Following ipsilateral lung deflation, the modified thoracoscope is introduced into the thoracic cavity, where the mediastinum is now visible. (b) The right dorsal sympathetic chain (yellow arrows) is visualized through the parietal pleura as it passes over the neck of the ribs close to the costovertebral junction
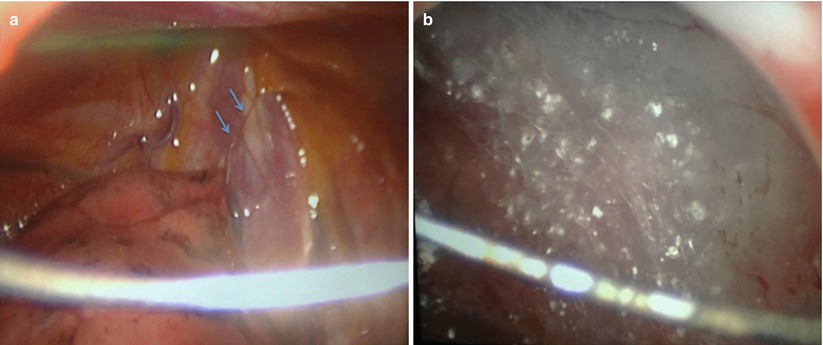
Fig. 8.7
Sometimes, small pleural adhesions (a, blue arrows) to widespread pleural adhesions (b) may be found, which preclude access to the ganglia and limit the completion of the procedure. If removal of the pleural adhesions is thought to be without risk, they can easily be divided endoscopically
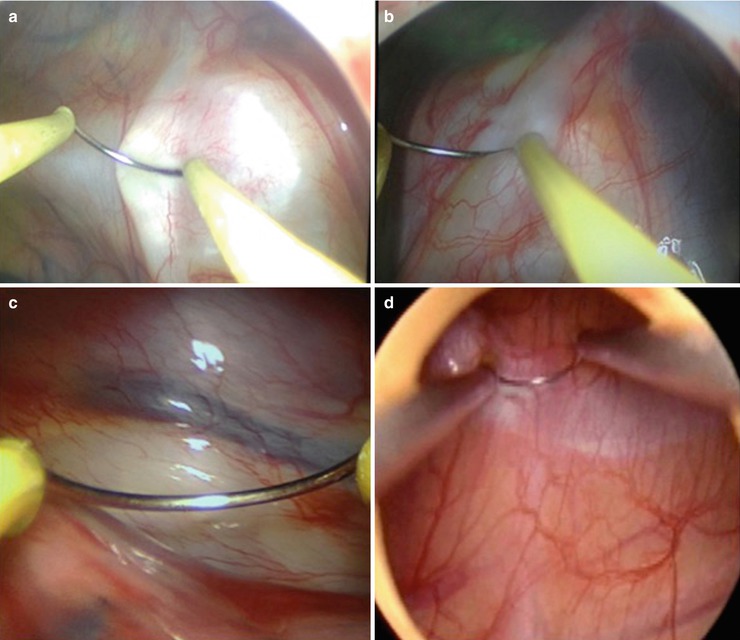
Fig. 8.8
(a–d) The ribs are endoscopically identified, as well as the sympathetic chain, which appears as a pink/white longitudinal structure protruding over the neck of the ribs, close to the costovertebral junction
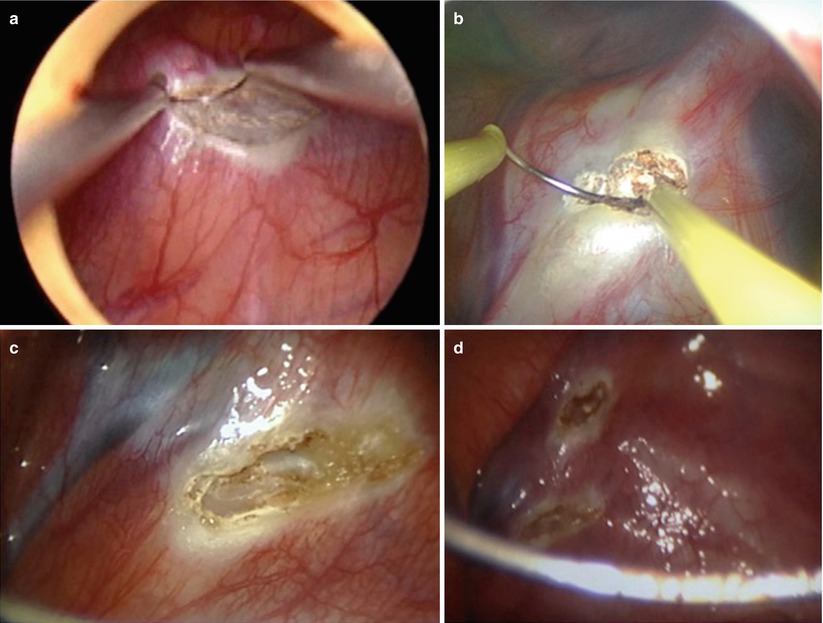
Fig. 8.9
(a–d) Electrocauterization (sympathicotomy) of the second, third, and/or fourth thoracic sympathetic ganglia (T2, T3, T4) is then performed, with special care to not injure the crossing vessels in the intercostal spaces or nearby (c)
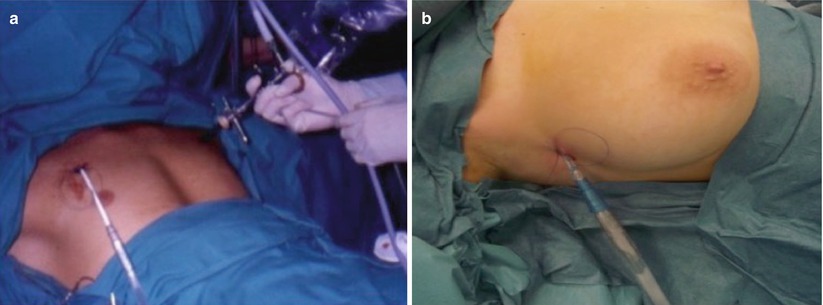
Fig. 8.10
The surgical procedure on the first side is completed by re-insufflation of the collapsed lung, insertion of a chest drain by the same operative incision on the mid-clavicular (a) or anterior axillary (b) line, and closure of the wound with cutaneous sutures. The entire procedure is then repeated on the opposite side

Fig. 8.11
Male patient after surgery in a half-sitting position with both arms abducted to 90°, before removal of the double-lumen endotracheal tube. Surgical dressings are applied on both sides to cover the incisions and keep the chest drains from moving
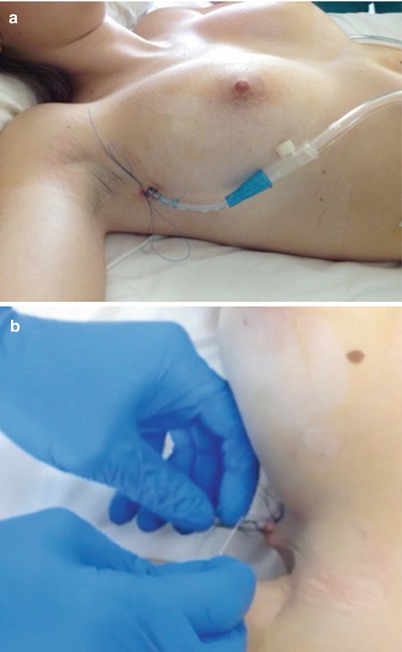
Fig. 8.12
(a, b) Removal of chest drains is performed 2 h after surgery, if a postoperative pulmonary radiograph has excluded the presence of pneumothorax or hemothorax. A #11 blade is used to cut the suture knot tied around the tube; once the knot is untied, the drain on one side is extracted from the chest with a rapid movement. Another operator then immediately ties the knot that was sutured all around the tube, in this way closing the incision
Conclusions
Minimally invasive endoscopic transthoracic sympathicotomy [2




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree