The authors’ vertical neck lifting procedure is an extended deep plane facelift, which elevates the skin and SMAS-platysma complex as a composite unit. The goal is to redrape cervicomental laxity vertically onto the face rather than laterally and postauricularly. The authors consider this an extended technique because it lengthens the deep plane flap from the angle of the mandible into the neck to release the cervical retaining ligaments that limit platysmal redraping. This technique does not routinely use midline platysmal surgery because it counteracts the extent of vertical redraping. A majority of aging face patients are good candidates for this procedure in isolation, but indications for combining vertical neck lifting with submental surgery are elucidated.
Key points
- •
The authors’ vertical neck lifting procedure is an extended deep plane facelift, which elevates the skin and superficial muscular aponeurotic system (SMAS)-platysma complex as a composite unit.
- •
The goal is to redrape cervicomental laxity vertically onto the face rather than laterally and postauricularly.
- •
The authors consider this an extended technique because it lengthens the deep plane flap from the angle of the mandible into the neck to release the cervical retaining ligaments that limit platysmal redraping.
- •
This technique does not routinely use midline platysmal surgery because it counteracts the extent of vertical redraping.
- •
A majority of aging face patients are good candidates for this procedure in isolation, but indications for combining vertical neck lifting with submental surgery are elucidated.
Introduction
Restoration of a youthful jawline and neck is an integral part of facial rejuvenation and arguably the most important goal for patients and doctors alike in aging face surgery. As the middle-aged population has grown and plastic surgery of the face has gained increasing acceptance, more patients are seeking cervicofacial rejuvenation at an earlier age; it is not uncommon to see patients in their 40s pursuing cervicofacial rhytidectomy. Even if the jowls are eliminated, residual neck redundancy may render the procedure a failure. The authors’ practice has noted that undertreatment of the neck is probably the most common reason for patients to seek revision rhytidectomy within the first 3 years after a primary facelift.
Although aesthetic ideals may differ between various surgeons and patients, a majority aspire to recreate a neck and jawline similar to those described by Ellenbogen and Karlin. Using a 26-year-old model, they establish 5 visual criteria believed to strike the eye as youthful after rhytidectomy: (1) distinct inferior mandibular border, (2) subhyoid depression, (3) visible thyroid cartilage bulge, (4) visible anterior sternocleidomastoid muscle (SCM) border, and (5) SM-SM angle of 90° (cervicomental angle between 105° and 120°).
Approaches to Achieve Aesthetic Ideal
To attain these aesthetic ideals, there have been myriad surgical approaches to address the issues existing in the lamina of the neck (ie, the skin, subcutaneous fat, and platysma and subplatysmal spaces). Choosing among the many different options requires a through physical examination. Surgeons must define which layers require manipulation and identify neck habitus that leads to poor neck lift outcomes. These include excessive supraplatysmal fat, redundant platymsa with vertical banding, and excessive fat or submandibular gland ptosis in the subplatymsa space. Those with a low anterior hyoid have a blunted cervicomental angle resulting from low insertion of the anterior belly of the digastric and the floor of mouth musculature. These specific problems limit a surgeon’s ability to redrape neck redundancy and create the 105° to 120° cervicomental angle.
Barring patients with these specific anatomic configurations, the 2 most essential layers to manipulate in neck lifting are the skin/subcutaneous tissues and the SMAS-platysma complex. Although advances in rhytidectomy techniques have drastically improved aesthetic outcomes, there is a lack of consensus as to the preferred approach to the neck. Since the description of the SMAS layer by Skoog in 1974, investigators have described a large variety of modifications of the sub-SMAS rhytidectomy. In 1976, Mitz and Peyronie described the 2-layer rhytidectomy.
Bidirectional Technique
Since 1976, several influential surgeons have independently adapted and modified the extent of SMAS dissection technique, including Connell, Owsley, Barton, Baker and Stuzin. All these surgeons use the bidirectional cervicofacial rhytidectomy developed by Owsley that pulls the skin and SMAS-platysma complex in different directions with different amounts of tension. In his original description of this bidirectional technique, the SMAS-platysma complex is elevated in a more superior or vertical fashion, and the skin is delaminated and redraped in a more lateral fashion. The benefits of a more vertical vector for SMAS directional pull have been recognized in both limited and extensive dissection techniques. An additional submental incision and central platysmal plication is the preferred approach for extensive aging neck changes. These techniques have produced reliable and consistent outcomes.
Bidirectional and Vertical Technique Compared
The authors’ vertical neck lifting technique differs from the bidirectional technique in 2 ways. First, both the SMAS-platysma complex and the skin are redraped in a more vertical vector. Additionally, the authors’ dissection involves release of the facial retaining ligaments as part of the dissection to allow for greater vertical elevation of the platysma, SMAS, and neck skin.
Proponents of lamellar dissection and bidirectional rhytidectomy contend that the skin and SMAS age at different rates and along different vectors, implying that the SMAS descends along a vertical gravitational vector but the skin along a horizontal vector. Dynamic examination of the preoperative rhytidectomy candidate reveals a greater laxity of the skin in the vertical vector than the horizontal vector in both the neck and lower cheek alike. This indicates the majority of aging of the skin occurs in the gravitational or vertical plane.
Skin Redraping
On closer examination of the bidirectional technique, horizontal skin redraping is performed to minimize superior temporal hairline displacement and temporal skin bunching that is associated with more vertical skin shifting techniques. Additionally, it limits the length of the temporal incision and hides more of the incision in the postauricular region as the skin redundancy is removed posteriorly. In vertical skin redraping techniques, temporal hairline shifts can be managed by appropriate modification of the anterior incision by using an extended pretemporal hair tuft incision. To avoid bunching, the temporal skin must be undermined subcutaneously and redraped. These techniques are discussed later.
There are other inherent problems with horizontal skin redraping that warrant re-evaluation of this approach. Horizontal skin redraping has a greater propensity to create a lateral sweep deformity along the lower face and mandible. Lateral tension on the skin creates a horizontal tension bar across the cheek from the perioral region extending laterally and superiorly toward the ear. In more severe cases, this has been described as a joker line cross-cheek depression from the oral commissure. This problem of the lateral tension vector was also described by Hamra as a “lateral sweep deformity.” This problem can be fixed with a revision rhytidectomy that redrapes the skin and the SMAS-platysma complex in a vertical antigravitational vector ( Fig. 1 ).

Another issue with more lateral redraping of the facelift skin flap is that it limits the degree of definition at the cervicomental angle, one of the primary goals of rhytidectomy espoused by Ellenbogen and Karlin. When the facelift skin flap is redraped in a more lateral fashion, the neck skin is tightened against the anterior neck overlying the hyoid and thyroid cartilages. In those patients with more redundant neck skin, this movement results in less redraping of the skin anterior to the hyoid, creating submental bunching and paramedian cervical pleating ( Fig. 2 ). Even though this may not be evident in the early postoperative period, it may become evident as the skin relaxes over the first 6 to 12 months after surgery. This approach is favored by many surgeons because it places most of the rhytidectomy scar in the posterior auricular region. The authors noticed these anterior submental failures in their practice prior to adopting the vertical technique approximately 7 years ago. Increasing experience with this technique has led the authors to notice this issue more often in patients presenting for a revision neck lift consultation after primary surgery ( Fig. 3 ).


Vertical elevation of the rhytidectomy flap maximizes redraping of the neck skin into the cervicomental angle, hence enhancing its definition. The minimal access cranial suspension (MACS) lift originally described by Tonnard and colleagues pioneered a purely vertical elevation of the skin and SMAS to accomplish cervicomental rejuvenation and limit the posterior auricular scar. In the authors’ technique, the skin flap is redraped more vertically, although not at a purely 90° angle with the horizontal, hence the term, vertical neck lift , is somewhat a misnomer. Purely vertical lifting tightens the neck skin against the submentum overlying the floor of mouth musculature (digastric and mylohyoid region). It does not conform tightly into the cervicomental angle, resulting in anterior skin neck laxity.
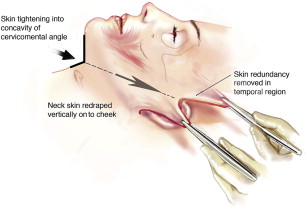
The authors studied the angle of maximal redraping of the neck skin flap into the cervicomental angle. The facelift was performed as originally described by Hamra, but with the modification of extending the deep plane below the angle of the mandible into the neck. After complete elevation of the flap, the flap is placed under a moderate amount of tension and then rotated through a medially based arc. Rotation begins from directly horizontal (0°) and moves toward the vertical axis (90°); for the left hemiface, this is counterclockwise whereas the right is clockwise. The angle that results in the greatest reduction of submental laxity and jowling was calculated using vector calculations from the excised vertical and horizontal skin excess. The average angle of redraping required was 60°, creating maximal cervical rejuvenation. This indicates that the flap is redraped more vertically than a purely superolateral angle of 45°. With this vector of flap displacement, the majority of neck skin redundancy is shifted superiorly and is removed in the temporal region rather than in the postauricular region ( Fig. 4 ). This effectively decreases the length of the posterior hairline incisions. The 60° angle is approximately parallel to a line drawn that bissects the cervicomental angle, tightening the redundant neck skin into this concavity.
SMAS-platysma Complex
As discussed previously, to counter the effects of aging and gravity, the authors prefer a more vertical vector of redraping for both the SMAS-platysma complex and the skin. With the deep plane technique, the SMAS-platysma complex is left connected to the skin in the majority of the facelift flap and thus lifted in the same direction. These vectors can similarly be accomplished using a biplanar technique by elevating the delaminated SMAS and skin independently in a more vertical vector. The 60° angle that contours the cervicomental region also approximately parallels the zygomaticus major muscle, which is the vector of pull placed on the SMAS in a bidirectional high SMAS facelift.
Although the mean angle of redraping with the authors’ technique is 60°, vectors calculated in this study ranged from 40° to the 70°s. The 3-D structure of the skeleton as well as the degree of laxity present dictate where the sweet spot or direction of maximal redraping of the soft tissue envelope exists in each face; it is not a cookie-cutter approach. A statistically significant inverse relationship is noted when comparing the angle of greatest redraping with age: older patients in their 70s develop greater horizontal laxity of their tissue nearing 40° whereas younger patients in their 40s have more vertical facial redundancy requiring a vector of pull approaching 70°.
The importance of vertical displacement of the SMAS-platysma complex in this technique must be emphasized. Because neck failure is the most common issue requiring tuck-up surgery after rhytidectomy, appropriate mobilization of the deeper layers is crucial, especially in those with platysmal banding and cording. To understand how this can be accomplished, further elucidation of the anatomy of the SMAS and platysma is necessary as is what limits the SMAS-platysma complex’s motion.
The platysma has a higher extension onto the face than is classically illustrated in a variety of texts. A study of 71 consecutive deep plane rhytidectomies demonstrated that, on average, the platysma extends approximately 4 cm above the mandibular border into the cheek. The significance of this should not be overlooked for several reasons. First, this suggests that the platysma plays a larger role than previously thought with regard to facial rejuvenation with use and manipulation of the SMAS-platysma complex. Most importantly, it suggests that redundancy of platysma in the neck has a significant contribution from inferior displacement of the platysma from the cheek. This anatomy elucidates that platysmal redraping should occur more superiorly than laterally as is traditionally performed. Fogli and Desouches have promoted a technique that elevates the cervical portion of the platysma and anchors it to the malar periosteum, parotid fascia, and prelobar fibrous tissue. Cadaver studies comparing superolateral and vertical lifting of the SMAS-platysma complex further emphasize the importance of the vertical vector. Following intervention, Superolateral lifting was found to increase midline platysma dehiscence whereas it actually decreased after a vertical lift.
The SMAS-platysma complex can be mobilized with suture techniques, such as lateral platysma plication sutures or platysmal flap elevation. Even with subplatysmal dissection and release, there are tethering points and retaining ligaments that limit motion of the deeper tissues. These fibers, described as the retinacular cutis, are located in relatively constant spaces and connect dermis down through the subcutaneous tissues, SMAS, and the muscle and periosteum overlying the facial skeleton. They create anchoring points and septations between fat compartments that restrict redraping of the facial tissues. The importance of these retaining ligaments with regard to structure, shadowing, surgical implications, and relation to the facial nerve has been meticulously outlined. Theoretically and conceptually, these zones serve as fulcra around which the pendular descent of soft tissues and skin occurs with aging and gravity.
Ligament Release
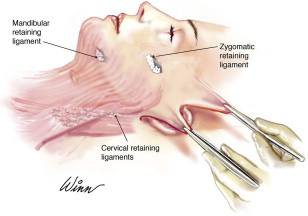
The important fibrous attachments to release in a vertical neck lift are the cervical retaining ligaments, the zygomatic cutaneous ligament, and the mandibular cutaneous ligament ( Fig. 5 ). Retaining ligaments exist in the neck that anchor the platysma to the deep fascia of the overlying the SCM, significantly limiting the mobility of the platysma. Limited subplatysmal dissection restricts the degree of neck mobilization and limits the extent of cervical rejuvenation. Releasing the cervical retaining ligaments allows for more significant redraping of the platysmal and midline cervical banding. Cadaver studies have been performed by the senior author (AAJ) comparing suture elevation of the platysma with release of the SMAS-platysma complex in a deep plane dissection extending into the neck. The deep plane dissection in this study included release of the cervical retaining ligaments. This study demonstrated there was a 554% greater redraping of submental platysmal laxity with the extended deep plane technique compared with SMAS-platysmal plication. There are several important clinical implications of these data. First, retaining ligament release has the advantage of minimizing the need for midline platysmal plication. The senior author has demonstrated this in a cohort of 323 patients, where using a greater lateral platysmal release with deep plane surgery reduced the rate of platysmal plication to 13%. Other investigators have claimed that they have completely eliminated the need for midline platysmoplasty with greater lateral release of the platysma but it is the authors’ experience that banding and redundancy associated with more advanced aged necks require midline platysmal reduction and plication combined with lateral platysmal release and elevation.
Midline plication
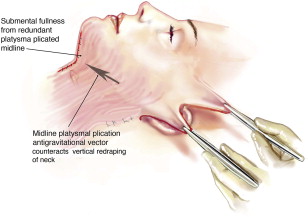
Limiting midline platysmal plication has further benefits in the vertical neck lift. Midline platysmal tightening directly counteracts the superior lifting of the neck tissues, thereby limiting the degree of potential improvement in the neck and jawline ( Fig. 6 ). Siwani and Friedman quantified this in their cadaveric dissections, showing that the addition of platysma plication in facelift reduced the amount of total lift at points along the jawline by approximately 40%. Further disadvantages of midline approaches include an additional incision, increased operative time, and increased recovery time and, most importantly, fullness and irregularities in the submentum. Midline platysma binding pulls the redundant platysma into the suprahyoid submentum, adding bulk, and potentially creates postsurgical irregularities that are difficult to correct. Adding bulk to this region also minimizes the desired definition of the neck in the cervicomental angle around the hyoid, as described by Ellenbogen.
Zygomatic-cutaneous ligaments
The zygomatic-cutaneous ligaments penetrate the upper border of the SMAS and bind it solidly to the zygoma. Their release is necessary to allow for vertical elevation of the SMAS-platysma complex from the neck to the inferior cheek (along the jawline) and into the upper cheek where the ligaments reside. Biomechnical studies have shown the zygomatic ligaments not only are the strongest ligament of the face but also have the least elongation or stretch. Because of how tightly they tether the skin, their release is also required to prevent bunching in the periorbital region when redraping redundant skin from the neck vertically into the midface and removing it in the temporal region. The necessity of ligamentous release to limit bunching and improve drapage was originally described by McGregor in the 1950s.
Mandibular cutaneous ligaments
The mandibular cutaneous ligaments, although often overlooked, can have significant implications in neck lifting surgery. The mandibular ligament is an osteocutaneous ligament that arises from the anterior third of the mandible and inserts directly into the dermis. Langevin and colleagues reported the dimensions of the ligament measuring 2 cm horizontally and 1.2 cm vertically, positioned 4.5 cm anterior to the angle of the mandible. The clinical importance of this ligamentous complex in rhytidectomy surgery was originally described by Furnas, who noted that their release was required to adequately redrape the prejowl sulcus that is anterior to the jowl. He further noted that the cutaneous extension of this ligament causes skin indentations that can be magnified after rhytidectomy, ultimately causing patient dissatisfaction.
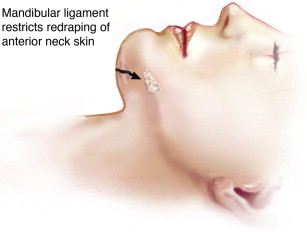
In vertical neck lifting, the authors have noted that the mandibular ligaments can also limit submental rejuvenation. The senior author has been measuring the clinical skin tethering effect of the mandibular ligament along the mandibular margin in 75 consecutive patients. This ligament limits motion of the skin along the jawline on average 5 cm posterior to the symphysis (Andrew A. Jacono, MD, personal communications, 2013). This tethering limits mobilization and redraping of the submental skin directly inferior and anterior to the mandibular ligament as it is lifted vertically. This results in anterior submental redundancy and recurrent neck ptosis in the early postoperative period ( Fig. 7 ). When this occurs, a secondary procedure is often required, such as tuck-up neck lift surgery or a variety of other direct neck excision procedures. These sequelae are more problematic in necks with greater skin redundancy. As a guide, the authors use Baker’s classification of neck aging, which grades progressive aging from I to IV. Class III patients with moderate cervical skin laxity and poor neck skin elasticity (usually in their late 50s–60s) and class IV patients with severe deep skin neck laxity and folds below the level of the cricoid (usually in their late 60s–70s) are most at risk for the mandibular ligaments limiting neck skin redraping.
Introduction
Restoration of a youthful jawline and neck is an integral part of facial rejuvenation and arguably the most important goal for patients and doctors alike in aging face surgery. As the middle-aged population has grown and plastic surgery of the face has gained increasing acceptance, more patients are seeking cervicofacial rejuvenation at an earlier age; it is not uncommon to see patients in their 40s pursuing cervicofacial rhytidectomy. Even if the jowls are eliminated, residual neck redundancy may render the procedure a failure. The authors’ practice has noted that undertreatment of the neck is probably the most common reason for patients to seek revision rhytidectomy within the first 3 years after a primary facelift.
Although aesthetic ideals may differ between various surgeons and patients, a majority aspire to recreate a neck and jawline similar to those described by Ellenbogen and Karlin. Using a 26-year-old model, they establish 5 visual criteria believed to strike the eye as youthful after rhytidectomy: (1) distinct inferior mandibular border, (2) subhyoid depression, (3) visible thyroid cartilage bulge, (4) visible anterior sternocleidomastoid muscle (SCM) border, and (5) SM-SM angle of 90° (cervicomental angle between 105° and 120°).
Approaches to Achieve Aesthetic Ideal
To attain these aesthetic ideals, there have been myriad surgical approaches to address the issues existing in the lamina of the neck (ie, the skin, subcutaneous fat, and platysma and subplatysmal spaces). Choosing among the many different options requires a through physical examination. Surgeons must define which layers require manipulation and identify neck habitus that leads to poor neck lift outcomes. These include excessive supraplatysmal fat, redundant platymsa with vertical banding, and excessive fat or submandibular gland ptosis in the subplatymsa space. Those with a low anterior hyoid have a blunted cervicomental angle resulting from low insertion of the anterior belly of the digastric and the floor of mouth musculature. These specific problems limit a surgeon’s ability to redrape neck redundancy and create the 105° to 120° cervicomental angle.
Barring patients with these specific anatomic configurations, the 2 most essential layers to manipulate in neck lifting are the skin/subcutaneous tissues and the SMAS-platysma complex. Although advances in rhytidectomy techniques have drastically improved aesthetic outcomes, there is a lack of consensus as to the preferred approach to the neck. Since the description of the SMAS layer by Skoog in 1974, investigators have described a large variety of modifications of the sub-SMAS rhytidectomy. In 1976, Mitz and Peyronie described the 2-layer rhytidectomy.
Bidirectional Technique
Since 1976, several influential surgeons have independently adapted and modified the extent of SMAS dissection technique, including Connell, Owsley, Barton, Baker and Stuzin. All these surgeons use the bidirectional cervicofacial rhytidectomy developed by Owsley that pulls the skin and SMAS-platysma complex in different directions with different amounts of tension. In his original description of this bidirectional technique, the SMAS-platysma complex is elevated in a more superior or vertical fashion, and the skin is delaminated and redraped in a more lateral fashion. The benefits of a more vertical vector for SMAS directional pull have been recognized in both limited and extensive dissection techniques. An additional submental incision and central platysmal plication is the preferred approach for extensive aging neck changes. These techniques have produced reliable and consistent outcomes.
Bidirectional and Vertical Technique Compared
The authors’ vertical neck lifting technique differs from the bidirectional technique in 2 ways. First, both the SMAS-platysma complex and the skin are redraped in a more vertical vector. Additionally, the authors’ dissection involves release of the facial retaining ligaments as part of the dissection to allow for greater vertical elevation of the platysma, SMAS, and neck skin.
Proponents of lamellar dissection and bidirectional rhytidectomy contend that the skin and SMAS age at different rates and along different vectors, implying that the SMAS descends along a vertical gravitational vector but the skin along a horizontal vector. Dynamic examination of the preoperative rhytidectomy candidate reveals a greater laxity of the skin in the vertical vector than the horizontal vector in both the neck and lower cheek alike. This indicates the majority of aging of the skin occurs in the gravitational or vertical plane.
Skin Redraping
On closer examination of the bidirectional technique, horizontal skin redraping is performed to minimize superior temporal hairline displacement and temporal skin bunching that is associated with more vertical skin shifting techniques. Additionally, it limits the length of the temporal incision and hides more of the incision in the postauricular region as the skin redundancy is removed posteriorly. In vertical skin redraping techniques, temporal hairline shifts can be managed by appropriate modification of the anterior incision by using an extended pretemporal hair tuft incision. To avoid bunching, the temporal skin must be undermined subcutaneously and redraped. These techniques are discussed later.
There are other inherent problems with horizontal skin redraping that warrant re-evaluation of this approach. Horizontal skin redraping has a greater propensity to create a lateral sweep deformity along the lower face and mandible. Lateral tension on the skin creates a horizontal tension bar across the cheek from the perioral region extending laterally and superiorly toward the ear. In more severe cases, this has been described as a joker line cross-cheek depression from the oral commissure. This problem of the lateral tension vector was also described by Hamra as a “lateral sweep deformity.” This problem can be fixed with a revision rhytidectomy that redrapes the skin and the SMAS-platysma complex in a vertical antigravitational vector ( Fig. 1 ).
Another issue with more lateral redraping of the facelift skin flap is that it limits the degree of definition at the cervicomental angle, one of the primary goals of rhytidectomy espoused by Ellenbogen and Karlin. When the facelift skin flap is redraped in a more lateral fashion, the neck skin is tightened against the anterior neck overlying the hyoid and thyroid cartilages. In those patients with more redundant neck skin, this movement results in less redraping of the skin anterior to the hyoid, creating submental bunching and paramedian cervical pleating ( Fig. 2 ). Even though this may not be evident in the early postoperative period, it may become evident as the skin relaxes over the first 6 to 12 months after surgery. This approach is favored by many surgeons because it places most of the rhytidectomy scar in the posterior auricular region. The authors noticed these anterior submental failures in their practice prior to adopting the vertical technique approximately 7 years ago. Increasing experience with this technique has led the authors to notice this issue more often in patients presenting for a revision neck lift consultation after primary surgery ( Fig. 3 ).
Vertical elevation of the rhytidectomy flap maximizes redraping of the neck skin into the cervicomental angle, hence enhancing its definition. The minimal access cranial suspension (MACS) lift originally described by Tonnard and colleagues pioneered a purely vertical elevation of the skin and SMAS to accomplish cervicomental rejuvenation and limit the posterior auricular scar. In the authors’ technique, the skin flap is redraped more vertically, although not at a purely 90° angle with the horizontal, hence the term, vertical neck lift , is somewhat a misnomer. Purely vertical lifting tightens the neck skin against the submentum overlying the floor of mouth musculature (digastric and mylohyoid region). It does not conform tightly into the cervicomental angle, resulting in anterior skin neck laxity.
The authors studied the angle of maximal redraping of the neck skin flap into the cervicomental angle. The facelift was performed as originally described by Hamra, but with the modification of extending the deep plane below the angle of the mandible into the neck. After complete elevation of the flap, the flap is placed under a moderate amount of tension and then rotated through a medially based arc. Rotation begins from directly horizontal (0°) and moves toward the vertical axis (90°); for the left hemiface, this is counterclockwise whereas the right is clockwise. The angle that results in the greatest reduction of submental laxity and jowling was calculated using vector calculations from the excised vertical and horizontal skin excess. The average angle of redraping required was 60°, creating maximal cervical rejuvenation. This indicates that the flap is redraped more vertically than a purely superolateral angle of 45°. With this vector of flap displacement, the majority of neck skin redundancy is shifted superiorly and is removed in the temporal region rather than in the postauricular region ( Fig. 4 ). This effectively decreases the length of the posterior hairline incisions. The 60° angle is approximately parallel to a line drawn that bissects the cervicomental angle, tightening the redundant neck skin into this concavity.
SMAS-platysma Complex
As discussed previously, to counter the effects of aging and gravity, the authors prefer a more vertical vector of redraping for both the SMAS-platysma complex and the skin. With the deep plane technique, the SMAS-platysma complex is left connected to the skin in the majority of the facelift flap and thus lifted in the same direction. These vectors can similarly be accomplished using a biplanar technique by elevating the delaminated SMAS and skin independently in a more vertical vector. The 60° angle that contours the cervicomental region also approximately parallels the zygomaticus major muscle, which is the vector of pull placed on the SMAS in a bidirectional high SMAS facelift.
Although the mean angle of redraping with the authors’ technique is 60°, vectors calculated in this study ranged from 40° to the 70°s. The 3-D structure of the skeleton as well as the degree of laxity present dictate where the sweet spot or direction of maximal redraping of the soft tissue envelope exists in each face; it is not a cookie-cutter approach. A statistically significant inverse relationship is noted when comparing the angle of greatest redraping with age: older patients in their 70s develop greater horizontal laxity of their tissue nearing 40° whereas younger patients in their 40s have more vertical facial redundancy requiring a vector of pull approaching 70°.
The importance of vertical displacement of the SMAS-platysma complex in this technique must be emphasized. Because neck failure is the most common issue requiring tuck-up surgery after rhytidectomy, appropriate mobilization of the deeper layers is crucial, especially in those with platysmal banding and cording. To understand how this can be accomplished, further elucidation of the anatomy of the SMAS and platysma is necessary as is what limits the SMAS-platysma complex’s motion.
The platysma has a higher extension onto the face than is classically illustrated in a variety of texts. A study of 71 consecutive deep plane rhytidectomies demonstrated that, on average, the platysma extends approximately 4 cm above the mandibular border into the cheek. The significance of this should not be overlooked for several reasons. First, this suggests that the platysma plays a larger role than previously thought with regard to facial rejuvenation with use and manipulation of the SMAS-platysma complex. Most importantly, it suggests that redundancy of platysma in the neck has a significant contribution from inferior displacement of the platysma from the cheek. This anatomy elucidates that platysmal redraping should occur more superiorly than laterally as is traditionally performed. Fogli and Desouches have promoted a technique that elevates the cervical portion of the platysma and anchors it to the malar periosteum, parotid fascia, and prelobar fibrous tissue. Cadaver studies comparing superolateral and vertical lifting of the SMAS-platysma complex further emphasize the importance of the vertical vector. Following intervention, Superolateral lifting was found to increase midline platysma dehiscence whereas it actually decreased after a vertical lift.
The SMAS-platysma complex can be mobilized with suture techniques, such as lateral platysma plication sutures or platysmal flap elevation. Even with subplatysmal dissection and release, there are tethering points and retaining ligaments that limit motion of the deeper tissues. These fibers, described as the retinacular cutis, are located in relatively constant spaces and connect dermis down through the subcutaneous tissues, SMAS, and the muscle and periosteum overlying the facial skeleton. They create anchoring points and septations between fat compartments that restrict redraping of the facial tissues. The importance of these retaining ligaments with regard to structure, shadowing, surgical implications, and relation to the facial nerve has been meticulously outlined. Theoretically and conceptually, these zones serve as fulcra around which the pendular descent of soft tissues and skin occurs with aging and gravity.
Ligament Release
The important fibrous attachments to release in a vertical neck lift are the cervical retaining ligaments, the zygomatic cutaneous ligament, and the mandibular cutaneous ligament ( Fig. 5 ). Retaining ligaments exist in the neck that anchor the platysma to the deep fascia of the overlying the SCM, significantly limiting the mobility of the platysma. Limited subplatysmal dissection restricts the degree of neck mobilization and limits the extent of cervical rejuvenation. Releasing the cervical retaining ligaments allows for more significant redraping of the platysmal and midline cervical banding. Cadaver studies have been performed by the senior author (AAJ) comparing suture elevation of the platysma with release of the SMAS-platysma complex in a deep plane dissection extending into the neck. The deep plane dissection in this study included release of the cervical retaining ligaments. This study demonstrated there was a 554% greater redraping of submental platysmal laxity with the extended deep plane technique compared with SMAS-platysmal plication. There are several important clinical implications of these data. First, retaining ligament release has the advantage of minimizing the need for midline platysmal plication. The senior author has demonstrated this in a cohort of 323 patients, where using a greater lateral platysmal release with deep plane surgery reduced the rate of platysmal plication to 13%. Other investigators have claimed that they have completely eliminated the need for midline platysmoplasty with greater lateral release of the platysma but it is the authors’ experience that banding and redundancy associated with more advanced aged necks require midline platysmal reduction and plication combined with lateral platysmal release and elevation.
Midline plication
Limiting midline platysmal plication has further benefits in the vertical neck lift. Midline platysmal tightening directly counteracts the superior lifting of the neck tissues, thereby limiting the degree of potential improvement in the neck and jawline ( Fig. 6 ). Siwani and Friedman quantified this in their cadaveric dissections, showing that the addition of platysma plication in facelift reduced the amount of total lift at points along the jawline by approximately 40%. Further disadvantages of midline approaches include an additional incision, increased operative time, and increased recovery time and, most importantly, fullness and irregularities in the submentum. Midline platysma binding pulls the redundant platysma into the suprahyoid submentum, adding bulk, and potentially creates postsurgical irregularities that are difficult to correct. Adding bulk to this region also minimizes the desired definition of the neck in the cervicomental angle around the hyoid, as described by Ellenbogen.
Zygomatic-cutaneous ligaments
The zygomatic-cutaneous ligaments penetrate the upper border of the SMAS and bind it solidly to the zygoma. Their release is necessary to allow for vertical elevation of the SMAS-platysma complex from the neck to the inferior cheek (along the jawline) and into the upper cheek where the ligaments reside. Biomechnical studies have shown the zygomatic ligaments not only are the strongest ligament of the face but also have the least elongation or stretch. Because of how tightly they tether the skin, their release is also required to prevent bunching in the periorbital region when redraping redundant skin from the neck vertically into the midface and removing it in the temporal region. The necessity of ligamentous release to limit bunching and improve drapage was originally described by McGregor in the 1950s.
Mandibular cutaneous ligaments
The mandibular cutaneous ligaments, although often overlooked, can have significant implications in neck lifting surgery. The mandibular ligament is an osteocutaneous ligament that arises from the anterior third of the mandible and inserts directly into the dermis. Langevin and colleagues reported the dimensions of the ligament measuring 2 cm horizontally and 1.2 cm vertically, positioned 4.5 cm anterior to the angle of the mandible. The clinical importance of this ligamentous complex in rhytidectomy surgery was originally described by Furnas, who noted that their release was required to adequately redrape the prejowl sulcus that is anterior to the jowl. He further noted that the cutaneous extension of this ligament causes skin indentations that can be magnified after rhytidectomy, ultimately causing patient dissatisfaction.
In vertical neck lifting, the authors have noted that the mandibular ligaments can also limit submental rejuvenation. The senior author has been measuring the clinical skin tethering effect of the mandibular ligament along the mandibular margin in 75 consecutive patients. This ligament limits motion of the skin along the jawline on average 5 cm posterior to the symphysis (Andrew A. Jacono, MD, personal communications, 2013). This tethering limits mobilization and redraping of the submental skin directly inferior and anterior to the mandibular ligament as it is lifted vertically. This results in anterior submental redundancy and recurrent neck ptosis in the early postoperative period ( Fig. 7 ). When this occurs, a secondary procedure is often required, such as tuck-up neck lift surgery or a variety of other direct neck excision procedures. These sequelae are more problematic in necks with greater skin redundancy. As a guide, the authors use Baker’s classification of neck aging, which grades progressive aging from I to IV. Class III patients with moderate cervical skin laxity and poor neck skin elasticity (usually in their late 50s–60s) and class IV patients with severe deep skin neck laxity and folds below the level of the cricoid (usually in their late 60s–70s) are most at risk for the mandibular ligaments limiting neck skin redraping.









