Introduction
Surgery remains a mainstay of treatment for lower extremity varicosities. Surgery may be as minimal as a local phlebectomy, as discussed in Chapter 8 , or as invasive as subfascial endoscopic perforator surgery or stripping of great and small saphenous veins combined with phlebectomy. Surgery must be tailored to the patient’s problem. The role of noninvasive testing prior to embarking on surgical correction cannot be overemphasized. This chapter will provide a brief explanation of the major ablative surgical options that may be appropriate in the treatment of patients with lower extremity venous disease.
Stripping of Great and Small Saphenous Veins
•
Basic concepts, indications and patient selection
Most symptoms in chronic venous disease are due to reflux. For the vast majority of patients treated by experienced clinicians, duplex scanning has replaced all other forms of venous testing, including qualitative assessment of reflux. Patients are tested in the standing position on the upper step of a two-step platform by asking them to stand normally but relaxed and with most of their weight on the leg opposite the leg being interrogated.
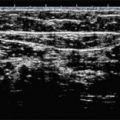
The great saphenous vein (GSV) is imaged with the patient facing the technologist and the study leg slightly forward and externally rotated. The vein is examined for dilation, compressibility, and echogenicity in the transverse orientation. The longitudinal view is also assessed, and thickness of the vein wall, valvular changes or any echogenicity are documented ( Figs 10.1–10.5 ). The operator tests for reflux in the axial vein and perforating veins using color flow, and also uses the pulsed Doppler with the probe in longitudinal orientation to test for reflux in the saphenofemoral junction, the common femoral vein above and below the saphenofemoral junction, and the proximal GSV. The Valsalva maneuver is appropriate for provoking reflux in the groin, but may not provoke reflux inferior to the groin if there is a competent valve in the groin area. Therefore, compression of the leg above and below the segment being interrogated is used to detect evidence of reflux in the target segment. For example, saphenofemoral and proximal great saphenous reflux may be masked during the Valsalva maneuver by the presence of a competent valve in the proximal common femoral vein. The author tests for this by squeezing the upper thigh between two hands (lateral and medial) while interrogating the proximal GSV with pulsed Doppler and looking for ‘to and fro’ flow. The Valsalva maneuver may also fail to demonstrate reflux in the more inferior segment of the GSV and the practitioner must depend on proximal and distal compression maneuvers to elicit reflux when it is significantly inferior to the saphenofemoral junction.



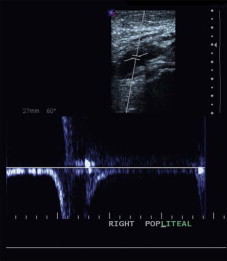
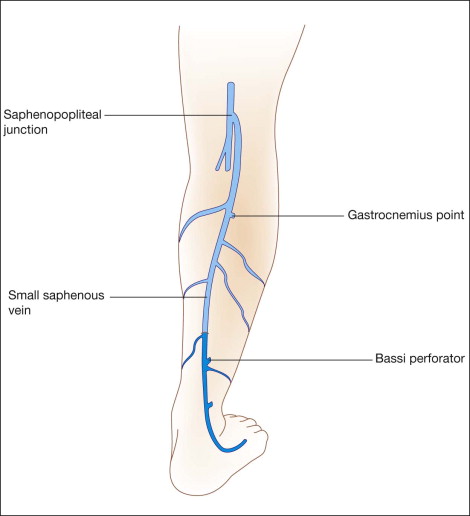
The small saphenous vein (SSV) is examined for dilation and reflux with the patient standing and facing away from the technologist and the popliteal vein is imaged from this approach as well. Examination of the SSV is started at the ankle posterior to the lateral malleolus. The course of the vein is traced proximally where it very quickly drifts to the midline of the calf and can clearly be identified within its superficial fascial compartment. Branches and connections are usually seen in the mid-calf and the operator eventually traces these branches but not until the entire course of the SSV is studied.
The examination is done in the transverse view until the whole course of the vein is mapped. Often the vein will extend proximally past the popliteal fossa and sometimes eventually connects to the GSV in the upper medial thigh or groin as the so-called vein of Giacomini. The SSV is also interrogated in the longitudinal view near the popliteal fossa to document the saphenopopliteal junction. This is a critical step since the SSV may empty into a gastrocnemius branch, which then enters the popliteal fossa. If this is not well understood and observed by the surgeon, important errors can occur and precipitate damage and/or thrombosis of the deep venous system at the time of ablative treatments. The small diameter of the SSV may make it difficult to interrogate with pulsed Doppler or color flow in longitudinal orientation and occasionally this must be performed in transverse orientation.
Careful documentation is required of reflux, valve anatomy and any vessel defects in the common femoral and popliteal veins, with the operator specifically looking for evidence of previously unsuspected deep venous abnormalities, which if present dictate a conventional supine duplex scan of the entire deep venous system. Evidence of significant chronic abnormalities in the deep vein system would not necessarily preclude any planned ablation of the superficial veins but further consideration and discussion with the patient may be necessary.
Correction of superficial venous insufficiency in the presence of deep venous insufficiency may improve the patient’s clinical degree of disability but does not obviate the necessity of wearing appropriate heavy compression stockings. This must be carefully explained to the patient since many patients assume that surgery will render the wearing of these hose unnecessary. Stockings are the best treatment and prophylaxis for deep venous insufficiency, and long-term compliance is the key to success, especially postoperatively.
Being physically present to conduct the exam with the technologist is important to the surgeon’s understanding of the patient’s pathophysiology and to the eventual success of any contemplated operation. Readers interested in a more detailed description of diagnostic standards may wish to consult Mattos and Sumner or Nicolaides.
•
Stripping procedures
The first description of ‘stripping’ of the GSV is generally credited to Babcock. This operation is most commonly considered for patients with primary varicose veins, usually clusters of varicose branches of the GSV adjacent to (and probably communicating with) the various named perforating veins connecting the deep and superficial veins of the medial leg. The strategy of this approach is to ablate the major axial conduit through which venous hypertension is transmitted from the level of the right atrium to the superficial veins of the leg in patients with venous valvular incompetence. Furthermore, ablation of the axial vein theoretically leads to thrombotic occlusion of any perforating veins that communicate directly with the GSV. However, the effectiveness of stripping for perforator ablation is less certain, especially below the knee, where the major axially directed vein that connects with the Cockett perforating veins is the posterior arch (Leonardo) vein, which is not ablated by a conventional stripping operation ( Fig. 10.6 ).
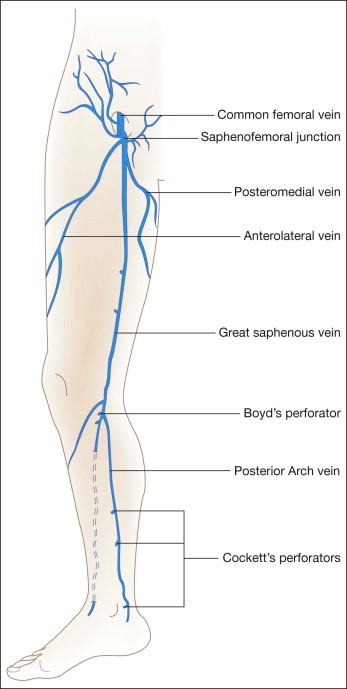
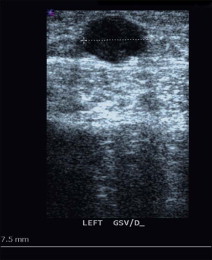
Some surgeons use thresholds of ≥6 mm in diameter with reflux of at least 0.5 seconds in duration when considering ablation or removal of the axial GSV. However, the ideal patient for classic stripping of the GSV will have: (1) a dilated GSV (≥8 mm in diameter adjacent to the saphenofemoral junction) with saphenofemoral or proximal great saphenous reflux lasting at least 1.5 seconds; (2) clusters of varicose branches in the calf and/or thigh; (3) absence of significant perforating vein reflux; and (4) no evidence of significant changes of deep vein thrombosis (DVT). Removal may still be indicated in certain patients with distal communicating branches off a normal-caliber GSV with reflux, or with dilatation of the GSV without observable reflux. In practice, most patients with symptomatic varicose veins disease have areas of the GSV much larger than 8 mm in diameter and reflux lasting much longer than 1.5 seconds. The location of the lowest connecting perforator, which is often in the distal thigh or very proximal calf, is marked during the duplex examination since removal of the vein below this level is unnecessary and increases the chance of saphenous nerve injury ( Fig. 10.7 ). In practice, it is rarely necessary to remove the GSV below the upper calf as is discussed in more detail below.
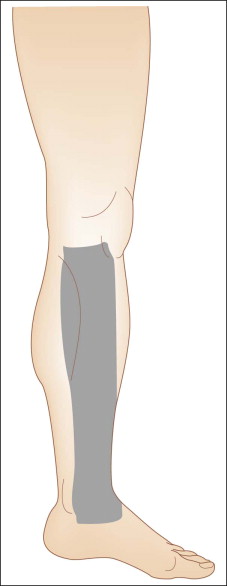
Small saphenous vein (SSV) stripping is performed less often and when it is performed, it may be limited to a segment and not the entire SSV. The superior termination of the SSV is variable ( Fig. 10.8 ) and must be clearly delineated at the time of any diagnostic imaging study to provide sufficient information on which therapeutic decisions may be based. It may be useful to re-image the patient just before surgery and to mark the location of the SSV and its termination at and above the knee to allow accurate placement of incisions. This may even be performed in the operating room with the patient prone on the operating table. SSV segments at least 4 mm in diameter with demonstrable reflux can be considered for stripping. It is rarely necessary to remove the distal third of this vein, and normally the vein can be removed to the proximal or mid-calf just below the last major communicating varicosity identified during the duplex examination.
•
Technique
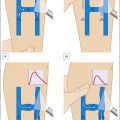
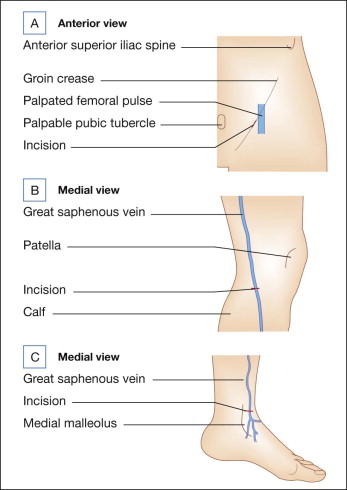
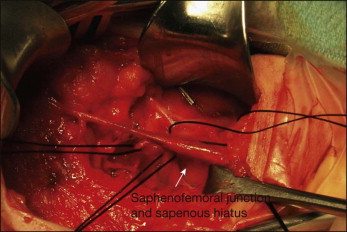
Subarachnoid block (spinal) or general anesthesia is used when classic stripping operations are performed. In the majority of patients, the GSV may be removed using two small incisions. One incision in the groin crease just medial to the femoral pulse usually allows easy exposure of the proximal GSV and saphenofemoral junction ( Fig. 10.9 ). The incision should be large enough to provide adequate exposure to allow a complete and safe procedure, particularly in obese patients, but is usually 3 cm or less in length. The incision should not be made inferior to the groin crease since an inappropriately inferior incision would make control of branches other than the GSV more difficult.
It is appropriate to obtain control of the GSV near the saphenofemoral junction, but to not ligate the vein at this point for reasons that will become apparent later. First, the operator may attempt to identify all other branches, most often including the anterolateral saphenous, external pudendal, superficial epigastric, and circumflex iliac branches ( Fig. 10.10 ). Each of these latter branches is then divided and attempts made to ligate each of their primary branches as well to reduce the risk of persistent or recurrent communication between the deep and superficial venous systems in the groin. The posteromedial aspect of the common femoral vein is inspected, with frequent attendant identification and ligation of a small (2–4 mm) branch in this area that might contribute to recurrences. At the completion of this portion of the operation, the axial GSV is the only remaining unligated branch at the saphenofemoral junction.
The authors have noted that it was necessary to remove only part of the GSV in a majority of more than 1500 patients. In many such cases, the vein may be removed from upper calf to groin using a second incision placed medially just inferior to the knee instead of at the medial malleolus. Use of the retrograde pin stripping technique as described by Oesch (see Chapter 11 ) may allow even more limited surgical trauma to the patient, but still allow adequate removal of abnormal axial GSV ( Fig. 10.11 ). The key is appropriate preoperative documentation by duplex scan of the venous anatomy. In many patients, dilatation, reflux, and incompetent perforators will end at or just below the knee. There is no need to remove any more of the normal vein without incompetent associated perforators and this more limited approach reduces the risk of saphenous nerve injury. Failure of the surgeon to be present at the diagnostic duplex scan venous evaluation makes this essential operative decision difficult to make. When the entire GSV is dilated with reflux, it is necessary to remove the entire axial GSV. The vein can be identified through an incision at the anterior aspect of the medial malleolus. By dissecting carefully on the top of the vein and carefully cleaning it posteriorly, the risk of saphenous nerve injury can be minimized.