Venous Imaging/Duplex Ultrasound
 INTRODUCTION
INTRODUCTION
Proper diagnosis of venous system disease often requires both functional and anatomic information about the venous circulation. Functional tests such as the maximum venous outflow (MVO), the venous refilling time (VRT), and the calf muscle pump ejection fraction (MPEF) (see Chapter 9) are extremely useful as measures of whole leg or regional venous function but can detect only regionally significant reflux or a significant impediment to venous outflow. Anatomic imaging of the venous system does not assess overall hemodynamic function but can detect even very small amounts of local and regional reflux and can visualize both obstructing and nonobstructing thrombus.
Successful imaging of the deep venous system requires a thorough knowledge of venous anatomy and physiology, as well as meticulous attention to detail. The most useful modalities available for venous imaging are contrast venography, magnetic resonance imaging (MRI), and most importantly, Duplex ultrasound, which has become the “gold standard” of venous imaging (Table 10-1).1–3 Superficial venous imaging can be performed by modern duplex ultrasound with resolution as clear as 1 mm. A detailed protocol for its use is described in this chapter.
TABLE 10-1
Venous Imaging Methods
Contrast venography
Magnetic resonance imaging (MRI)
Radionuclide venography
Spiral CT scan
Radiolabeled fibrinogen
Radiolabeled monoclonal antibody to fibrin
Duplex imaging (the gold standard)
Nonultrasound Radiologic Procedures
Many techniques have been employed historically to evaluate the venous system. As technology improves, the development of less-invasive techniques has come to surpass previously employed invasive techniques. An understanding of the history of venous imaging is important to the physician treating venous disease.
CONTRAST VENOGRAPHY Contrast venography is neither absolutely sensitive nor specific in the diagnosis of venous pathology, but prior to the introduction of duplex ultrasound, it was the standard to which all other diagnostic tests were compared. It is no longer the standard and is reviewed here to give historical perspective. Duplex ultrasound has replaced contrast venography in the vast majority of clinical situations.
Deep and superficial venous thrombosis and venous insufficiency may be evaluated by contrast venography, although deep venous visualization is typically intended. Digital subtraction venography can be performed for even more superb images. Superficial veins and varices are imaged by direct injection of a radiopaque contrast material into the veins of interest. After a tourniquet is placed around the lower leg in order to occlude the superficial, but not the deep, veins, contrast material is injected into a superficial dorsal foot vein. The contrast passes through perforating veins into the deep venous system. Thrombus appears either as a filling defect outlined by contrast or as a “cutoff” lesion stopping the flow of contrast (Figure 10-1). Reflux is detected when contrast flows backward through failed valves into a more distal segment of the vein.
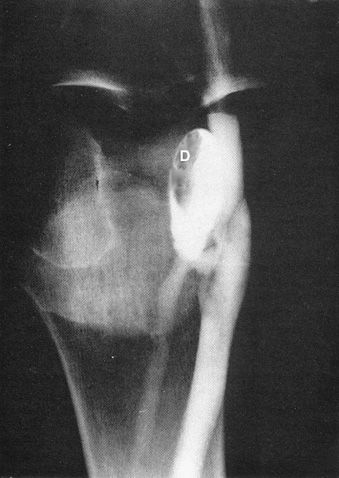
![]() FIGURE 10-1 Contrast venography demonstrating a filling defect (D) typical of a thrombus.
FIGURE 10-1 Contrast venography demonstrating a filling defect (D) typical of a thrombus.
If whole leg deep vein reflux is suspected, it may be confirmed by injection of contrast into the common femoral vein with the patient in the standing position. A complete reflux examination of the deep system is laborious, requiring passage of a catheter proximally from the saphenopopliteal junction (SPJ) all the way to the groin. With the patient standing, contrast is injected into each venous segment. Contrast venography is an invasive technique, with a significant morbidity and mortality. Apart from being painful, there is a risk that extravasation of dye into the dorsum of the foot may cause sloughing of tissue.4 At least 4 percent of patients develop venous thrombosis after venography.5 Anaphylactic reactions to contrast material occur in 3 percent of patients and are associated with a substantial mortality.6
MAGNETIC RESONANCE IMAGING Magnetic resonance imaging offers another method for the evaluation of venous pathology. Spin echo and gradient recalled acquisition in steady state (GRASS) images can reliably detect thrombus in deep veins of the calf, thigh, and pelvis.7 Duplex ultrasound, the standard for venous imaging, is limited by inaccuracy when assessing the pelvic and distal veins and in diagnosing a new thrombosis in the postthrombotic limb. MRI and sonographic elasticity imaging are more recent techniques that have shown promise in overcoming these limitations.8 MRI is also particularly useful because unsuspected nonvascular causes for leg pain and edema often may be seen on the MRI scan when the clinical presentation erroneously suggests venous insufficiency or venous obstruction.
RADIONUCLIDE VENOGRAPHY Radiolabeled substances used in scintigraphic lung scanning may be injected into the foot in the manner usually employed for contrast venography. The leg, thigh, and pelvis may be scanned as the radionuclide ascends through the venous circulation to the lungs. The resulting images are of low contrast and are sometimes difficult to read, but at some institutions, they are routinely performed as a part of every scintigraphic lung perfusion scan. If positive, the nuclear venogram is nearly as reliable as a standard contrast study. A negative nuclear venogram cannot rule out deep venous thrombosis (DVT) and should rarely be trusted as evidence against the diagnosis.
SPIRAL CT SCAN The spiral computed tomography (CT) scan can provide very high-resolution images of vascular structures and gives early promise for peripheral venous imaging, but the need for contrast material makes it a less attractive modality than MRI. It is used commonly for chest imaging.
RADIOLABELED FIBRINOGEN If fibrinogen labeled with radioactive iodine (I-131) is injected into a patient with acute DVT, radiolabeled fibrinogen is incorporated into the developing thrombus. Radioactive “hot spots” may be imaged with a gamma camera or a simple counter may be used to demonstrate the localization of radioactivity at sites within the legs and pelvis. Radiolabeled fibrinogen can detect both acutely forming thrombus and subacute fully formed thrombus but cannot detect chronic thrombus that has been in place for several months. The technique is of limited modern value for two major reasons: several days are required to incorporate detectable amounts of radioisotope within a developing thrombus, and fibrinogen is a human blood product that comes with an unavoidable risk of infection. It is not possible to distinguish between superficial venous thrombosis and DVT using this method, as even a superficial chemical phlebitis due to sclerotherapy gives a positive fibrinogen scan.9
RADIOLABELED MONOCLONAL ANTIBODY TO FIBRIN Radiolabeled fibrinogen scanning is primarily of historical interest, but radiolabeled monoclonal antibodies to mature and immature thrombus have shown promise as a more rapid and more reliable test for venous thrombosis and pulmonary thromboembolism.10
DUPLEX IMAGING
The availability of inexpensive ultrasound equipment has made it much easier to diagnose and treat venous pathology in the office. B-mode (or time-delay) ultrasound forms a grayscale picture based upon the time delay of ultrasonic pulses reflected from deep structures. Structures that absorb, transmit, or scatter ultrasonic waves appear as dark areas, whereas structures that reflect the waves back to the transducer appear as white areas in the image. Vessel walls reflect ultrasound, while blood flowing in a vessel absorbs and scatters ultrasound in all directions; thus, the normal vessel appears as a dark-filled, white-walled structure. Nonflowing blood and thrombus are somewhat ultrasonically reflective, although less so than the vessel wall; thus, they appear as heterogeneous areas of gray echogenicity within the vessel.
A duplex scanner is the combination of a B-mode ultrasound transducer with a pulse wave (PW) Doppler transducer built in. The scanner screen can be set to display just the B-mode image, or just a time plot of the Doppler flow velocity, or both at the same time. The Doppler information can also be heard through the speakers, exactly like the sound from a handheld Doppler transducer. Color flow imaging converts the Doppler information to visually colorize areas of the B-mode image in which flow has been detected. Vessels with flow are colored red for flow in one direction and blue for flow in the other, with a graduated color scale to reflect the speed of the flow (Figure 10-2). Color flow systems are significantly easier to use than are gray-scale systems and can help the examination go much faster, but most skilled examiners are of the opinion that color does not really increase the intrinsic sensitivity or specificity of the B-mode duplex scan. Incompetent small perforating veins, however, may be nearly impossible to detect without color flow.
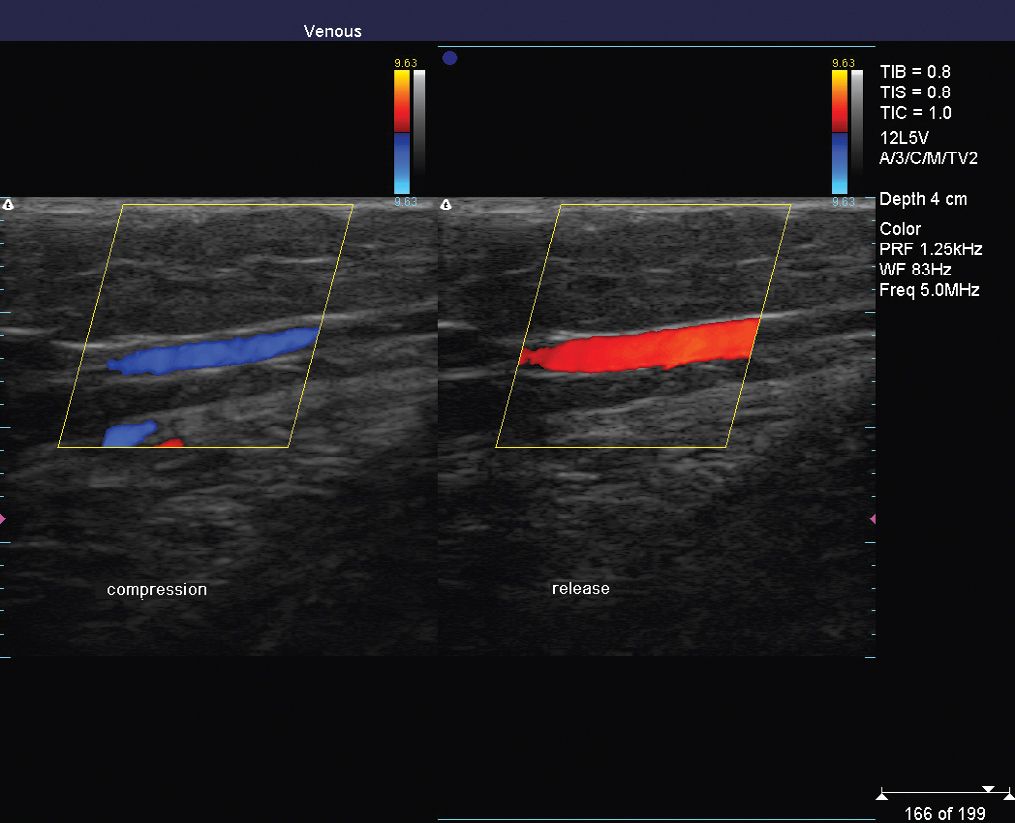
![]() FIGURE 10-2 Color flow Duplex image showing flow in opposite directions as represented by red and blue coloration.
FIGURE 10-2 Color flow Duplex image showing flow in opposite directions as represented by red and blue coloration.
Modern color flow duplex ultrasound equipment can provide flow information at the same time that it gives surprisingly high-resolution views of both deep and superficial venous systems, including delicate valves, small perforating veins, and even reticular veins as small as 1 mm in diameter. Using the duplex scanner, it is possible to elucidate venous pathophysiology with great confidence. Venous thrombosis is readily detected and the anatomic pathways of normal and aberrant flow in the deep and superficial venous systems lie fully exposed.
Lower extremity examinations are best performed using solid-state linear array transducers, which have no moving parts within the transducer. Much older models have a fluid-filled head in which the transducer mechanically rotates but the images are inferior. These devices have all but been abandoned. Most modern ultrasound devices, particularly the portable laptop footprint variety, have variable frequency transducers that can change frequencies through a range of typically 5–12 MHz. Higher frequencies are used for superficial vessels and lower frequencies are used for deeper vessels and for obese patients. Multiple frequencies are necessary because the depth at which clear images can be seen is a function of the frequency. Low transducer frequencies not only permit the sound to reach deeper structures but also yield poorer near-field images of superficial structures. Newest high-resolution computers utilizing high-frequency transducers allow examination of veins as small as 0.75 mm. Newest Duplex units are tiny and relatively inexpensive and are indispensable for evaluation of the superficial venous system. By packing 30 and 40 components into a single electronic chip, newer technology will soon enable ultrasound equipment manufacturers to develop compact devices that shrink console-sized equipment from laptop into handheld units. The smallest unit on the market is the NanoMaxx (Sonosite, Bothell, WA) and measures 14.1″ L × 8.2″ H × 2.3″ W (35.8 cm L × 20.8 cm H × 5.8 cm W) with an LCD touchscreen display of 8.4″ (21.3 cm) diagonal.
Technique for Identification of Thrombus
Although thrombus sometimes is clearly seen within the veins, thrombus may be present without being directly visible. The diagnosis of intravascular thrombus depends upon the fact that a direct downward pressure readily collapses normal veins. This pressure is placed on the vein with the ultrasound transducer. For a normal vein, walls will coapt (compress together completely) and the vein will disappear on the scan display, indicating the absence of thrombus. This is often referred to as the vein “winking” at the examiner. A vein that does not compress completely along with echogenic signals in the lumen usually indicates the presence of thrombus (Figure 10-3). This is the hallmark of testing for thrombus by Duplex ultrasound. Compression to observe complete collapse in a normal vein is performed repeatedly along the entire course of the vein with the transducer held in a transverse plane. When the transducer is held longitudinally, some areas of thrombus may be missed because the vein may not be visualized in its entirety.
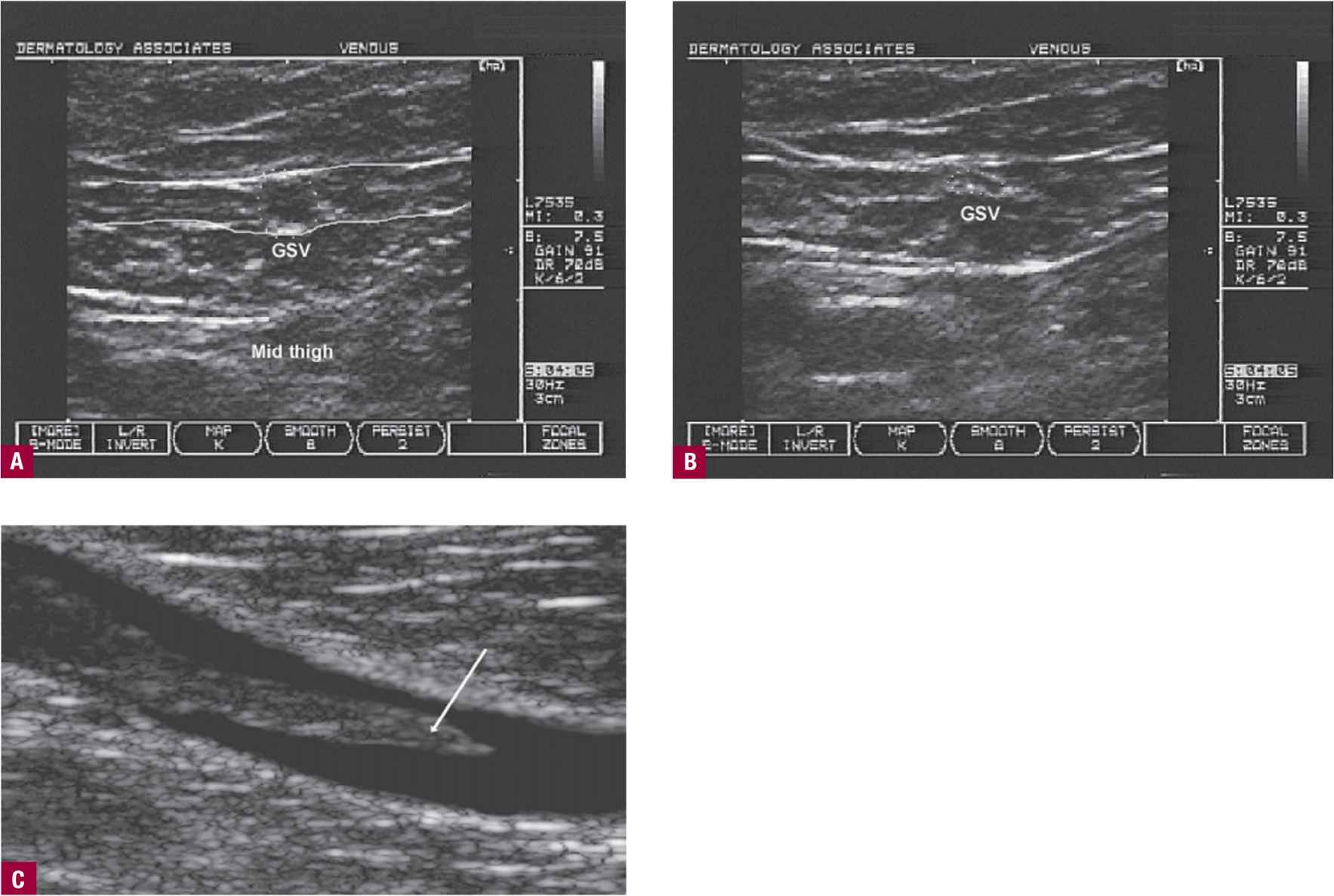
![]() FIGURE 10-3 Detection of thrombus by duplex ultrasound. A. A vein in cross section. The superficial fascia surrounding the great saphenous vein (GSV) is enhanced in white, showing as two parallel white lines above and below the GSV (round dark circle in the middle). B. Compression of that vein shows disappearance; therefore, no thrombus is present. C. Compression of a deep vein shows inability to compress with echogenic lumen. This is a sign of thrombus. The tip of the thrombus is indicated with an arrow. This is a longitudinal view, which would be confirmed by a transverse view.
FIGURE 10-3 Detection of thrombus by duplex ultrasound. A. A vein in cross section. The superficial fascia surrounding the great saphenous vein (GSV) is enhanced in white, showing as two parallel white lines above and below the GSV (round dark circle in the middle). B. Compression of that vein shows disappearance; therefore, no thrombus is present. C. Compression of a deep vein shows inability to compress with echogenic lumen. This is a sign of thrombus. The tip of the thrombus is indicated with an arrow. This is a longitudinal view, which would be confirmed by a transverse view.
Technique for Diagnosis of Reflux
Reflux is diagnosed by placing the transducer over the vessel in a longitudinal plane and observing the Doppler signal in the vessels while (with the free hand) the distal leg is momentarily compressed and released to increase the cephalad movement of blood (Figure 10-4). Functional valves permit flow only in the antegrade direction, but normal vessels can demonstrate brief retrograde flow due to slow closing of valves. Retrograde flow of duration greater than half second is considered pathologic reflux and reflux that lasts more than 2 s is hemodynamically significant. Reflux can also be seen in the transverse view but requires an expert examiner. Quantification of reflux volume and flow velocity requires measurement of cross-sectional flow and is beyond the scope of this text.
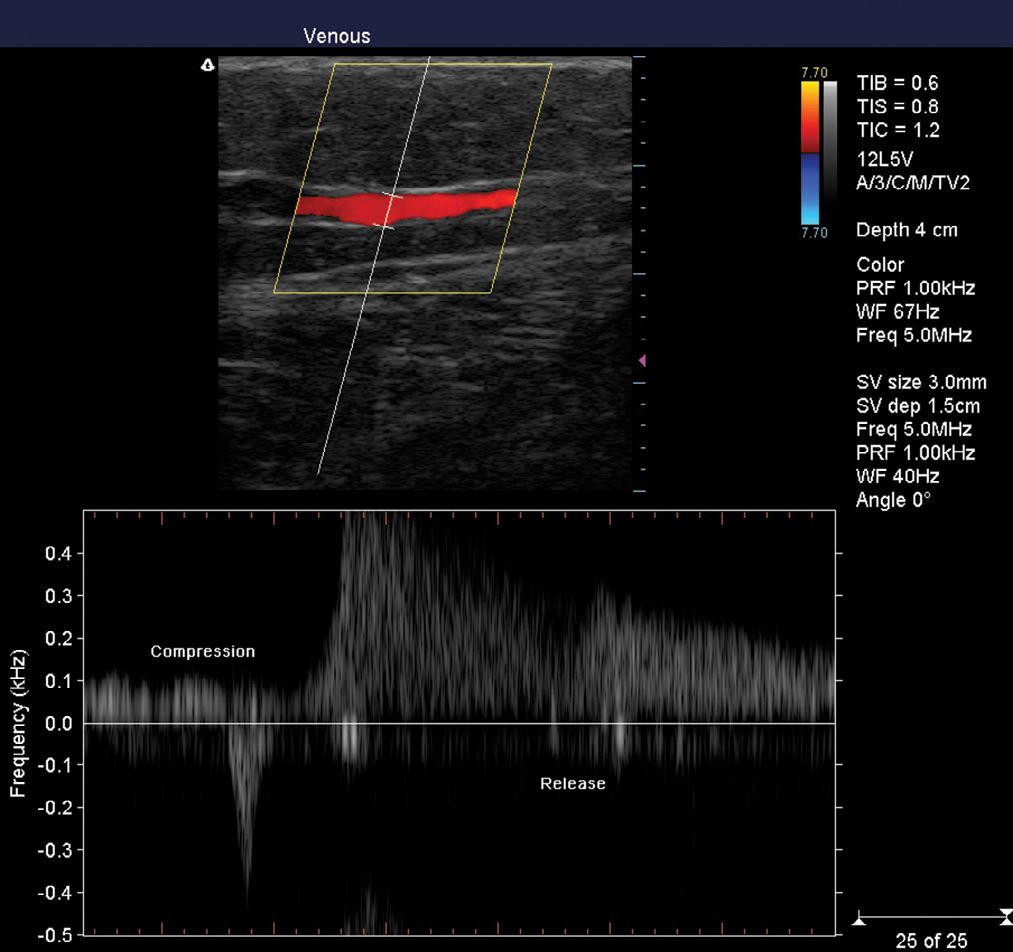
![]() FIGURE 10-4 Testing for reflux. A spectral image is added, which shows the PWD (pulse-wave Doppler) signal of flow. Distal compression shows flow away from the transducer, while release demonstrates flow toward the transducer. Unlike the handheld Doppler, this method allows exact visual assessment of reflux location.
FIGURE 10-4 Testing for reflux. A spectral image is added, which shows the PWD (pulse-wave Doppler) signal of flow. Distal compression shows flow away from the transducer, while release demonstrates flow toward the transducer. Unlike the handheld Doppler, this method allows exact visual assessment of reflux location.
The Complete Duplex Examination
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


