Common Patterns of Abnormal Veins: Guide and Summary by Region
 COMMON PATTERNS OF ABNORMAL VEINS: GUIDE AND SUMMARY BY REGION
COMMON PATTERNS OF ABNORMAL VEINS: GUIDE AND SUMMARY BY REGION
Regional Anatomy of Varices
To build up venous insufficiency diagnostic skills, a regional approach to the frequently and commonly observed anatomical patterns can be useful. Artificially dividing the leg into eight quadrants—lateral, medial, anterior, and posterior, both above and below the knee—is the approach for this chapter (Figure 5-1). The goal is to provide both the novice and experienced phlebologist a visual guide to the common (and occasionally less common) pattern of abnormal veins that one is likely to encounter in everyday practice. A regional approach, while allowing for a “cookbook” type reference, leads to some unavoidable repetition in the discussion and presentation, because many veins extend through different regions or have tributaries that cross many boundaries. Clinical photographs accompanied by simplified diagrams and tables can facilitate rapid identification of the root causes of an unfamiliar pattern of reflux, but there is no substitute for a complete understanding of normal venous anatomy.
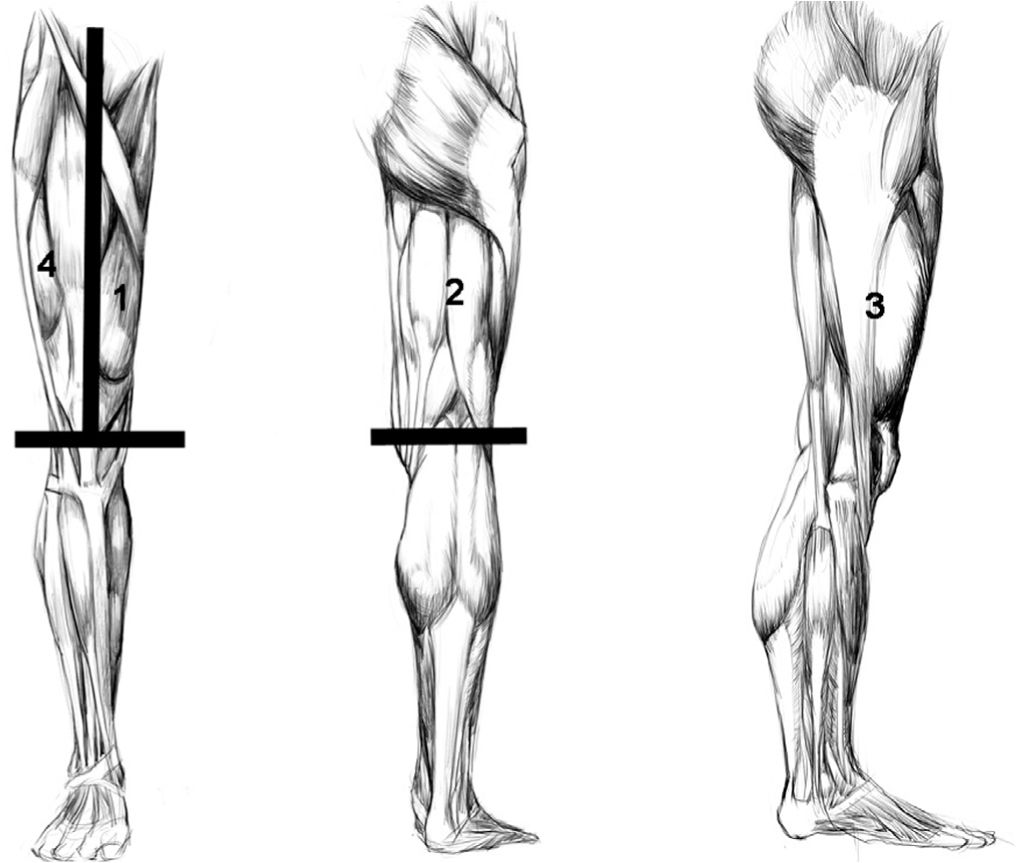
![]() FIGURE 5-1 Overview of the Quadrants of the Upper Thigh: 1. Medial Thigh. 2. Posterior Thigh. 3. Lateral Thigh. 4. Anterior Thigh.
FIGURE 5-1 Overview of the Quadrants of the Upper Thigh: 1. Medial Thigh. 2. Posterior Thigh. 3. Lateral Thigh. 4. Anterior Thigh.
MEDIAL THIGH
1. Pudendal. Most proximally, visualization of blue reticular to 3–4 mm varicose veins can be seen extending from external genitalia (Table 5-1). These indicate reflux through the pudendal tributary of the great saphenous vein (GSV). These genital veins, when varicose, may cause pain during sexual intercourse as they become engorged with increased blood flow. Overall pain is usually worse during the progesterone phase of the menstrual cycle, a common theme of medical history. In early stages of pudendal reflux, the saphenofemoral junction (SFJ) is not involved and treatment is easily performed (Figure 5-2). Pudendal varicosities arising without associated saphenous reflux typically course only several centimeters on the proximal medial thigh. They are typically not associated with varicosities below the mid-thigh. Years after treatment, reflux may occur within the GSV beginning at the SFJ. It should be emphasized to the patients that this is not related to the previous treatment but represents a natural progression of venous disease and is almost predictable if left untreated.

![]() FIGURE 5-2 Pudendal vein varicosities on the uppermost medial thigh extending upward to the genitalia. Rapid response to sclerotherapy or phlebectomy is typical.
FIGURE 5-2 Pudendal vein varicosities on the uppermost medial thigh extending upward to the genitalia. Rapid response to sclerotherapy or phlebectomy is typical.
TABLE 5-1
Region 1—Medial Thigh
Pudendal vein
Incompetent saphenofemoral junction
Hidden reflux at saphenofemoral junction (only palpable on standing)
Superficial axial branch veins (medial tributaries) of GSV
Hunterian perforator connection—mid-thigh
Distal saccular saphenous vein dilation (just above knee)
Resistant telangiectatic matting (just above knee)
2. Bulging GSV at inguinal fold from SFJ reflux. Although rare, long-standing reflux at the SFJ in a thin individual may allow visualization of a flesh-colored spongy bulge, which is the incompetent SFJ. We have seen this spongy area in very thin individuals even when there is no reflux. Duplex confirmation of the reflux state is recommended. With a superficial GSV, it is imperative that great care is taken when placing tumescent or local anesthesia for endovenous techniques so as not to place the anesthesia within the vein. Duplex visualization while placing the anesthesia is highly recommended.
3. Hidden GSV reflux. Because of its depth in the proximal thigh, the GSV is usually not visible in the medial upper thigh region even when it carries high-grade reflux from a widely incompetent SFJ. Reflux may originate early on in younger patients from the subterminal valve and the terminal end of the saphenous vein may still be small. Duplex ultrasound examination in this region is essential if a proper diagnosis and treatment plan are to be made. The GSV may be palpable only with the patient standing.
4. Superficial tributaries of the GSV. Visible veins on the medial portion of the thigh are often superficial tributaries of the GSV that accept reflux from the GSV below and proximally (Figure 5-3). Typically, these veins are seen on the lower half of the medial thigh. Visualization by Duplex ultrasound shows the clear origin point at a superficial fascial gap at the point of termination of the tributary. Novices incorrectly assume that the varicose vein at the medial thigh surface represents either the GSV or the originating point of reflux. These varicosities represent the primary branches off of the main trunk (GSV). A solitary varicose vein in the medial thigh rarely represents a very superficial GSV. In this case, it is a varicose GSV trunk rather than a primary tributary.

![]() FIGURE 5-3 Large varicosity beginning on the upper thigh extending downwards (beginning from a main branch varicosity of the GSV).
FIGURE 5-3 Large varicosity beginning on the upper thigh extending downwards (beginning from a main branch varicosity of the GSV).
5. Hunterian perforator. Varicose veins that become palpable or visible in the mid-medial thigh are typically due to terminal or subterminal saphenofemoral incompetence, but they also rarely result solely from reflux through a thigh perforator such as a Hunterian perforator. The Hunterian reflux scenario is typically caused by reflux through the femoral vein (formerly referred to incorrectly as the superficial femoral vein) and often results in recurrence through other perforators after treatment. These dilated veins may not only be portions of the GSV, but also be accessory saphenous veins that pursue a parallel course (Figure 5-4). Reflux below the medial thigh has also been attributed to failed Dodd’s or other unnamed perforators. Typically, these patients have at least one or two incompetent valves in the deep system proximal to the perforator incompetence. Relative to saphenofemoral incompetence, this scenario is rare, comprising less than 5 percent of patients initially diagnosed with varicose veins on the medial thigh. Treatment of the superficial reflux is still performed, but the patient is informed that deep vein reflux may lead to other incompetent perforators and more superficial varicosities may develop during ensuing years.

![]() FIGURE 5-4 Large varicosity on the lower medial thigh from Hunterian perforator insufficiency; Duplex examinations showing origin of perforator incompetence in Hunterian canal are shown in Chapters 2 and 10.
FIGURE 5-4 Large varicosity on the lower medial thigh from Hunterian perforator insufficiency; Duplex examinations showing origin of perforator incompetence in Hunterian canal are shown in Chapters 2 and 10.
6. Distal segment saccular GSV dilatation. On the most distal portion of the medial thigh, just above the knee, the GSV may become more superficial with coursing posteriorly. The GSV may be apparent as an enlarged bulbous segment, particularly from examining from the back of the leg. Superficial phebitis in this area can produce a painful palpable mass of surprising size. The most common cause, as previously discussed, is reflux from higher in the thigh (Figure 5-5).
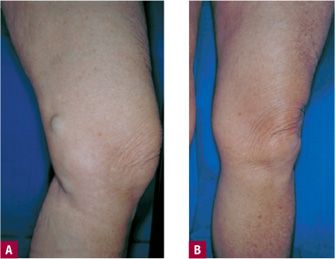
![]() FIGURE 5-5 A. Saccular GSV dilatation above the knee. This vein is usually a branch of the GSV, but rarely, as in this case, is the GSV itself in a superficial location. B. Excellent results after saphenofemoral ligation followed by ambulatory phlebectomy (seen here at 2 months).
FIGURE 5-5 A. Saccular GSV dilatation above the knee. This vein is usually a branch of the GSV, but rarely, as in this case, is the GSV itself in a superficial location. B. Excellent results after saphenofemoral ligation followed by ambulatory phlebectomy (seen here at 2 months).
7. Resistant telangiectasias. The medial thigh just above the knee can be the site of telangiectasias that are persistent and slow responders to treatment. As a result, this region has been referred to as the bane of the phlebologist because slow response, telangiectatic matting, and pigmentation are more common side effects after treatment in this location. Although saphenous system reflux is typically responsible for these vessels, they are occasionally fed by reticular veins originating from the lateral venous system (LVS) via peripatellar veins. New telangiectasias in this area are common when drainage pathways below are ligated, removed, or sclerosed while there remains a source of high-pressure reflux from above (Figure 5-6). Even when no source of reflux can be found for telangiectasias in this area, they may be resistant to treatment. When Duplex ultrasound fails to identify any source of reflux, it is possible that the telangiectasias may have resulted from local injury, with resulting angioneogenesis. This may occur particularly with higher concentrations of sclerosing agents that cause more inflammation at the time of treatment. Using the lowest concentration of a detergent solution or a milder solution such as glycerin is typically helpful. Hypothetically, relative oxygen deprivation during sleeping in the lateral position with knees pressed together may further stimulate angio-neogenesis via the wound healing mechanism. The authors anticipate the use of anti-angiogenesis topicals to mitigate this problem, but in the meantime use of topical steroids immediately after treating this area may be of benefit.
![]() FIGURE 5-6 Resistant telangiectasias on the medial thigh above the knee: the most troublesome region for persistent failure or recurrence after sclerotherapy. It may occur even after GSV reflux is totally eliminated.
FIGURE 5-6 Resistant telangiectasias on the medial thigh above the knee: the most troublesome region for persistent failure or recurrence after sclerotherapy. It may occur even after GSV reflux is totally eliminated.
POSTERIOR THIGH
1. Superficial gluteal. The most prevalent pattern of veins on the posterior thigh is a central zig-zagging reticular vein whose origin may be in the gluteal region (Table 5-2). It often runs just below the dermis, appearing immediately below the gluteal fold and is thought to be a superficial branch of the inferior gluteal vein. This reticular vein often terminates into a branch of the LVS in the postero-lateral portion of the popliteal fossa (Figure 5-7). Multiple telangiectasias often arise from these reticular veins.

![]() FIGURE 5-7 Reticular varicosity originating from superficial gluteal venous network with a possible contribution from posterior thigh perforating veins.
FIGURE 5-7 Reticular varicosity originating from superficial gluteal venous network with a possible contribution from posterior thigh perforating veins.
TABLE 5-2
Region 2—Posterior Thigh
Superficial gluteal
S-shaped reticular vein of posterior thigh
Posterior thigh perforators emptying into LVS
S-shaped reticular vein of posterior thigh
Giacomini vein
Incompetent sapheno-popliteal junction
Great saphenous vein (rarely)
2. Posterior thigh perforators emptying into LVS. This is the most common cause for a zig-zagging reticular vein on the posterior thigh that can both mimic and contribute to a reticular vein–telangiectatic web complex of the lateral subdermal venous plexus or system (LVS). Named posterolateral thigh perforator (PLTP) veins, these have been shown to connect with the posterior thigh deep veins about 3–8 cm deep that are occasionally seen on Duplex ultrasound to join tributaries of both femoral veins. The connections are often so small, however, that they cannot be seen on Duplex examination until visualized by tracing the path of injected foamed sclerosing solution. Some of these PLTP veins give rise to superficial tributaries that extend to the lower lateral and posterior thigh, whereas some give rise to tributaries alongside the small saphenous vein (SSV) and the anterior arch of the GSV.1 On the posterior lateral portion of the distal posterior thigh lie the multiple reticular veins of the LVS that can communicate with the PLTP. These interconnect with the smaller reticular varicosities that populate the popliteal fossa. The exact position of these is quite variable. When coursing within 2 cm of the popliteal fossa, reflux originating from the SSV—popliteal vein junction—must be excluded by Duplex examination before proceeding with the treatment of these veins (Figure 5-8).

![]() FIGURE 5-8 Posterior thigh perforators leading to large reticular varicosities and telangiectasias. This lower posterior thigh pattern responds extremely well to sclerotherapy.
FIGURE 5-8 Posterior thigh perforators leading to large reticular varicosities and telangiectasias. This lower posterior thigh pattern responds extremely well to sclerotherapy.
3. S-shaped reticular vein of posterior thigh. This reticular vein is visually observed snaking along the posterior thigh typically resulting from reflux from PLTP or from gluteal branches (Figure 5-9). It may also be considered a posterior component of the LVS. It is important to treat this varicosity when present for successful elimination of the LVS.
![]() FIGURE 5-9 S-shaped reticular vein on posterior thigh connecting with lateral venous system (LVS). This pattern is the most common on the posterior thigh and often accounts for pain during prolonged sitting. Arrow indicates possible connection with posterior thigh perforating veins.
FIGURE 5-9 S-shaped reticular vein on posterior thigh connecting with lateral venous system (LVS). This pattern is the most common on the posterior thigh and often accounts for pain during prolonged sitting. Arrow indicates possible connection with posterior thigh perforating veins.
4. Giacomini vein. This misunderstood but frequently invoked vein is merely an anastomic or communicating vein between the GSV and the SSV. It has quite a variable anatomic position. Typically, it is seen in the medial aspect of the posterior thigh coursing to the posterior thigh. There may be multiple communicating veins that connect GSV with SSV, but it is only called the Giacomini vein when it is located in the lower posterior thigh.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




