Physiologic and Other Tests for Venous Evaluation
 INTRODUCTION
INTRODUCTION
When symptoms of venous pathology are recognized or suspected, the underlying etiology can be rapidly assessed by visual examination according to patterns discussed in Chapter 5. Duplex ultrasound can confirm the physical examination via direct visualization of varicosities below the skin surface; however, careful diagnostic evaluation is necessary if one is to understand the particular venous hemodynamics of an individual patient. These tests are important to understand in terms of venous physiology. Although Duplex ultrasound can identify sites of valvular incompetence, photoplethysmography (PPG) and other forms of plethysmography offer a simple, reproducible technique to examine the physiologic significance of those findings and to correlate them with the patient’s symptoms. The historical importance of PPG is important enough to include in this text. It need not be reiterated that the continuous wave Doppler is analogous to the stethoscope, the plethysmographic test analogous to an electrocardiograph (EKG), and the duplex ultrasound equivalent to an echocardiogram. The availability of small, compact, high-resolution ultrasound machinery has made the Duplex ultrasound exam the new standard of care.
The performance and interpretation of diagnostic tests must be guided by knowledge of the pathophysiology underlying a patient’s clinical problem. For example, if a patient has signs and symptoms of pulmonary embolism (PE), failure to demonstrate deep venous thrombosis (DVT) (by any means) carries little clinical weight. In contrast, for a patient without signs of PE but with clinical signs of proximal DVT (pain and swelling of the leg extending well above the knee), the demonstration of a normal color-flow duplex examination is a reasonably reliable indicator of some other nonthrombotic etiology.
Blood Tests
Blood tests are rarely helpful in the evaluation of venous pathology. Most patients with deep venous thrombosis and PE have normal protime (PT) and activated partial thromboplastin time (APTT). A low white blood cell (WBC) count lowers the likelihood of an infectious process and raises the likelihood of DVT or PE, but an elevated WBC count is nonspecific because both normal and elevated WBC counts are common in patients with deep venous thrombosis.1 Both chronic venous insufficiency (venous congestion due to reflux) and DVT can mimic leg cellulitis, and true cellulitis is a frequent complication of both conditions.2
As D-dimer is a breakdown product of the lysis of cross-linked fibrin clots, plasma D-dimer levels have been investigated as potential aids to the diagnosis of DVT and PE. The literature suggests that about 10 percent of patients with symptoms of PE and a negative D-dimer screen (level less than 500 ng/ml) will have a positive pulmonary angiogram, while about 30 percent of similar patients with a positive D-dimer screen will have a positive angiogram.3
Functional Tests
Several important functional tests have proven in the past to be useful in helping to assess the condition of the superficial and deep venous systems (Table 9-1). Most important of these is the venous refilling time (VRT). The VRT is the time required for the leg to refill with blood after being emptied. A short VRT indicates early refilling. Early refilling most often occurs when valve damage in the deep or superficial veins allows venous blood to reflux downward into the extremity from retrograde venous flow, but it can also result from outflow obstruction or from increased arterial inflow due to arteriovenous malformations.
TABLE 9-1
Physiologic Venous Measurements of Plethysmography
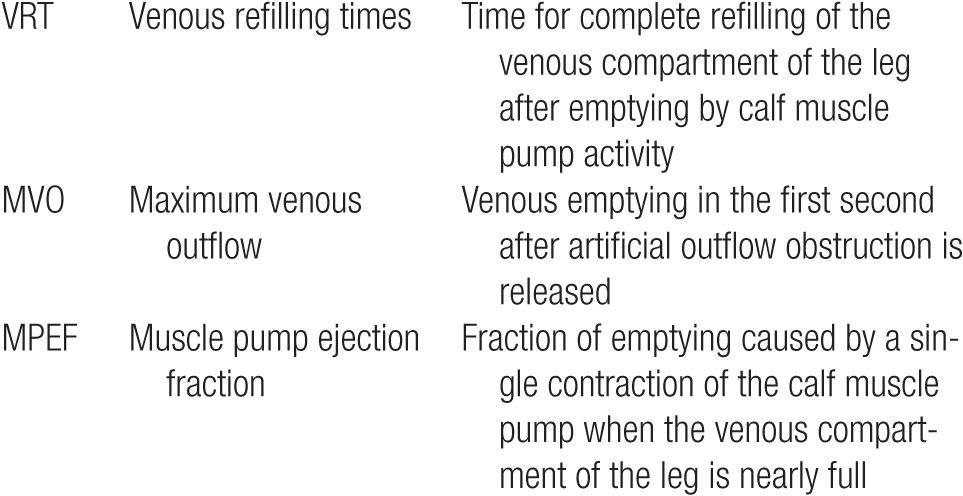
Two other commonly performed functional tests are of secondary importance. The fraction of blood that is pumped out of the calf with each exercise of the calf muscle is called the muscle pump ejection fraction (MPEF). The MPEF is decreased when there is a failure of the calf muscle pump mechanism, which can reflect muscle wasting, outflow obstruction, or widespread valve failure. When venous outflow from the lower leg is temporarily obstructed with a tourniquet, the fraction of blood that exits in the first second after tourniquet removal is the maximum venous outflow (MVO). A reduced MVO indicates venous outflow obstruction.
Ambulatory Venous Pressure
All of these functional parameters can be measured using a variety of different methods. The gold standard for functional testing of the lower extremity venous system is ambulatory venous pressure (AVP) monitoring. AVP tracings are obtained by placing a catheter into a superficial vein of the lower leg. Pressure changes are recorded while the patient exercises the calf muscle pump by walking, rising up on tiptoe, or performing ankle dorsiflexion movements. The recorded pressure tracings reflect the functional condition of the venous system (Figure 9-1). In a normal leg, each pumping cycle lowers the pressure, as blood is pumped inward and upward. Under normal conditions, 6–10 pumping cycles are sufficient to achieve a maximal reduction in pressure. With rest, the pressure normally rises again slowly as the leg is refilled, reaching a maximum in a healthy leg within 2–5 min. Direct measurement of the AVP is the most reliable means to detect abnormal venous function but is rarely used in clinical practice because of its invasive nature. Instead, a variety of plethysmographic methods are used to approximate the results of AVP monitoring.
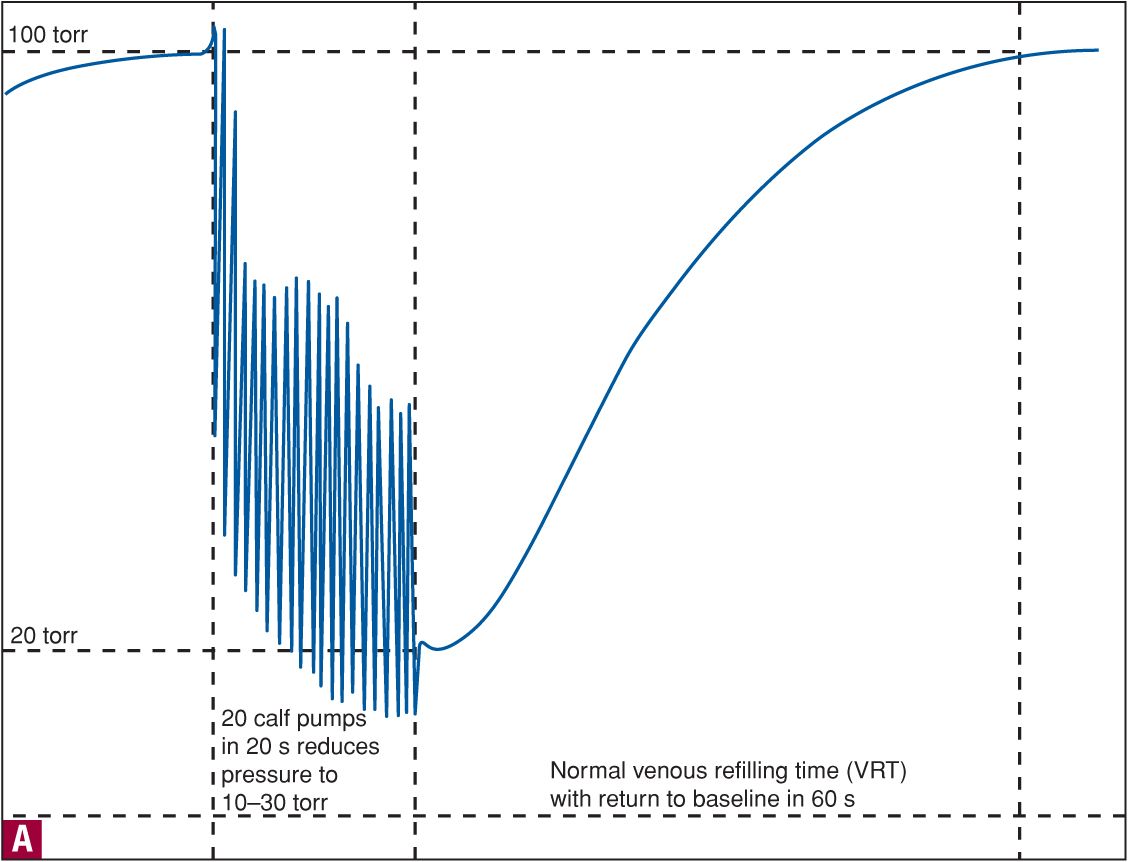
![]() FIGURE 9-1 A. Normal ambulatory venous pressure tracing. B. Ambulatory venous pressure in a patient with venous insufficiency.
FIGURE 9-1 A. Normal ambulatory venous pressure tracing. B. Ambulatory venous pressure in a patient with venous insufficiency.
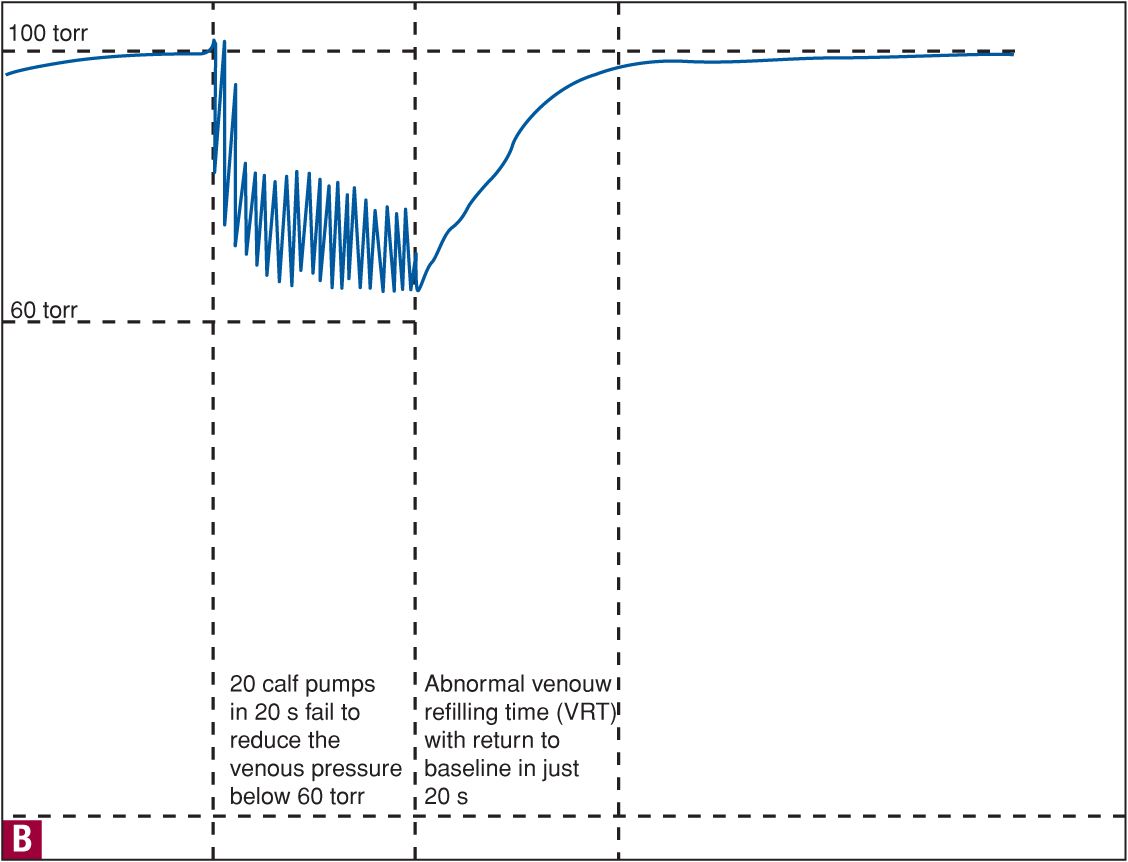
Plethysmography (D-PPG)
The term “plethysmography” describes a number of techniques used to measure pressure or volume changes directly or indirectly. A plethysmograph consists of a mechanism to sense a change within the lower leg and a modifying unit (transducer), which translates changes from a displacement sensing device into electrical energy that is then recorded. Each type of unit measures a different physical parameter in order to detect increased inflow or reduced outflow in the extremity being tested (Table 9-2). Impedance plethysmography (IPG) records changes in the characteristic impedance (electrical resistance) of the extremity. Strain-gauge plethysmography (SGPG) measures a change in the circumference of the calf by sensing tension changes in a wire or strap encircling the leg. PPG and the minor variant of PPG known as light reflection rheography (LRR) measure changes in light absorption within dermal capillaries.4 Pneumoplethysmography (PNPG) and air plethysmography (APG) depend upon direct measurement of changes in calf circumference or calf volume using an air bladder. The VRT and the MPEF can be measured using PPG or any other plethysmographic method, but the measurement of MVO requires a direct volumetric or pressure sensing method, such as SGPG, IPG, PNPG, or APG.
TABLE 9-2
Different Forms of Plethysmography
Despite the fact that it cannot be used to measure MVO, PPG was the most popular method for assessing venous function because it was inexpensive and easy to perform and could be used even by an examiner of limited experience.5,6 With PPG, a single photoelectric light source illuminates a small area of skin and an adjacent photoelectric sensor measures the reflectance of light.7 Near-infrared (940 nm) is well suited for optimal measurement of skin blood content because epidermal melanin absorption at this wavelength is limited to 15 percent of emitted light.
For any type of PPG examination, the patient sits on a chair in a relaxed position, with the knees bent at a 110°–120° angle. A small probe containing light-emitting and sensing diodes is taped to the medial aspect of the lower leg about 8–10 cm above the medial malleolus. The leg is allowed to fill for several minutes and the patient then dorsiflexes the foot 8–10 times, activating the calf muscle pump to empty the venous system. As the skin venous plexus empties, it causes increased reflectance of light because less hemoglobin remains to absorb light. A tracing is made of the changes in reflected light from the skin under the probe. After the calf muscle pumping ceases, blood refills the skin plexus, increasing amounts of light are absorbed as blood fills venules, and the PPG tracing returns to its initial resting value. The surface vessel filling time (PPG refill time) correlates very well with direct invasive pressure measurements of venous refilling.8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


