Venous Anatomy
 INTRODUCTION
INTRODUCTION
This text conforms to an international standard nomenclature known as the Venous Consensus Conference Classification that last met in 1994.1 Updated nomenclature was adopted in 2002 by an International Interdisciplinary Consensus committee and further elaborated upon in 2005.2,3 In keeping with the updated nomenclature, the term “great saphenous vein” (GSV) will be used for the vessel previously referred to as the “greater saphenous vein” or “long saphenous vein.” The term “small saphenous vein” (SSV) will be used for the vessel previously referred to as the “lesser saphenous vein” (LSV) or sometimes referred to in recent texts as the “short saphenous vein.” The previous use of LSV was often a source of confusion with the lateral venous system (LVS) described later. Veins that penetrate the fascia and connect together the deep and superficial systems are termed perforator veins. Many perforating veins have had recent name changes to reflect anatomic position rather than the physician originally describing them.
Veins that connect to other veins within the same fascial plane are referred to as communicating veins. The principal deep vein of the thigh is termed the “femoral vein,” which, together with the deep femoral vein (DFV), is termed as the “common femoral vein” under the new nomenclature and was previously referred to as the superficial femoral vein. Under the new nomenclature the principle deep veins of the thigh are the femoral vein (FV) and deep femoral vein (DFV). These two veins join just distal to the inguinal ligament to form the common femoral vein (CFV). The femoral vein (FV) was previously referred to as the “superficial femoral vein” which caused confusion since it is not a superficial vein and has led to death or disability for many patients with deep vein thrombosis. A summary of the updated nomenclature is included in Table 2-1. Important changes are listed for convenience in Table 2-2.
TABLE 2-1
Outline of Major Standard Nomenclature of Venous Anatomy of the Leg with Abbreviations
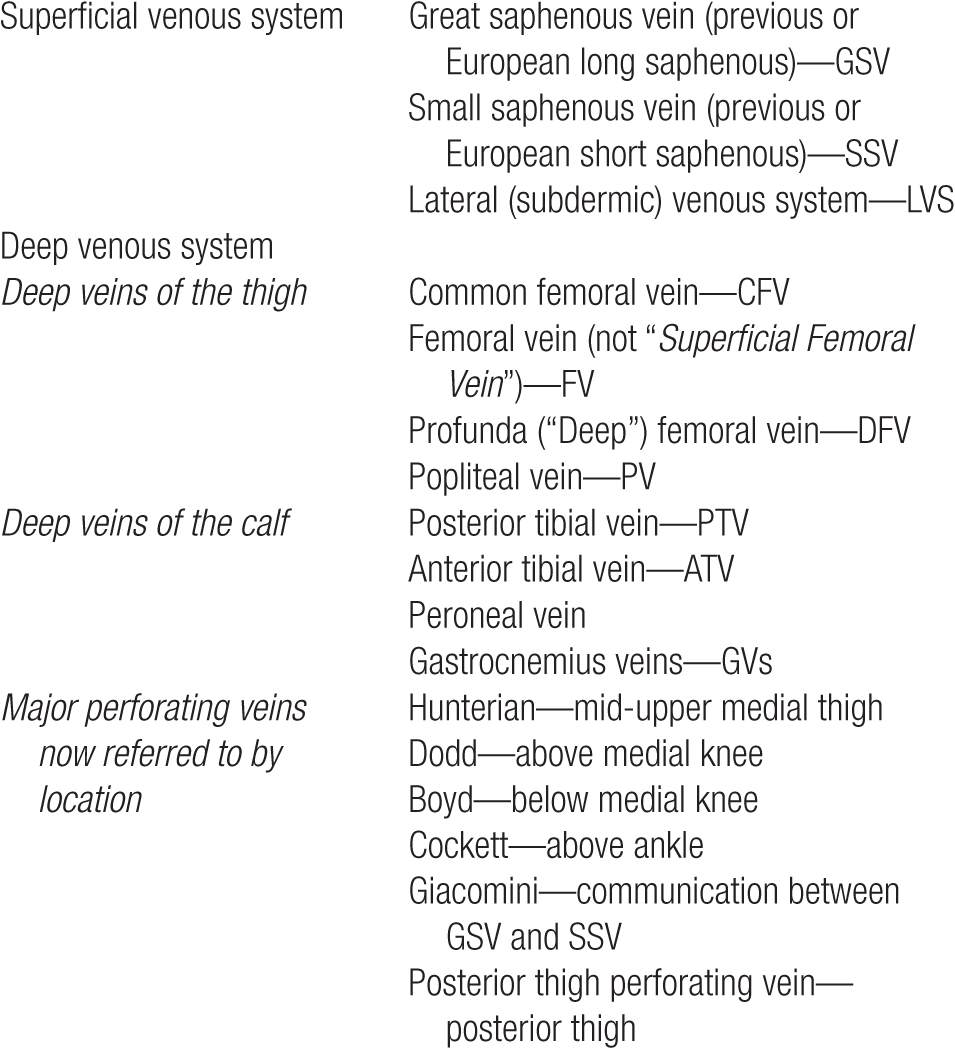
TABLE 2-2
Summary of Important Changes in Vein Anatomy Terminology
 ANATOMY OVERVIEW
ANATOMY OVERVIEW
The peripheral venous system functions both as a reservoir to hold extra blood and as a conduit to return blood from the periphery to the heart and lungs. Unlike arteries, which always possess three well-defined layers (a thin intima, a well-developed muscular media, and a fibrous adventitia), the smallest veins are composed of a single tissue layer. Only the largest veins possess internal elastic membranes, and at best, this layer is thin and unevenly distributed, providing little buttress against high internal pressures. The correct functioning of the venous system depends upon a complex series of valves and pumps that are individually frail and prone to malfunction, yet the system as a whole performs remarkably well under extremely adverse conditions.
Primary collecting veins of the lower extremity are passive thin-walled reservoirs that are enormously distensible. Most are suprafascial, surrounded by loosely bound alveolar and fatty tissue that is easily displaced. These suprafascial collecting veins can dilate to accommodate large volumes of blood with little increase in back pressure, so that the volume of blood sequestered within the venous system at any moment can vary by a factor of 2 or more without interfering with the normal function of the veins. Suprafascial collecting veins belong to the superficial venous system. Outflow from collecting veins is via “secondary” or “conduit” veins that have thicker walls and are less distensible. Most of these veins are subfascial and are surrounded by tissues that are dense and tightly bound. These subfascial veins belong to the deep venous system.
 FASCIAL ENVELOPE
FASCIAL ENVELOPE
The lower limb has a deep and superficial fascia to contain the high-pressure calf muscle pump and support the deep venous system. The deep fascia is a dense fibrous membrane investing the entire lower limb like an elastic stocking and serves as a functional boundary between deep and superficial veins. It is attached to the superficial fibers of the muscles it covers. It is normally thin over the gastrocnemius muscles and is absent only over the perforating veins and fossa ovalis, the latter being protected by the cribiform fascia. Because the deep fascia surrounds the muscles of the limb and is relatively inextensible, contraction of the muscles causes a rise in pressure to all structures within its compartment.
The superficial fascia is composed of two layers: a superficial layer of loculated fatty tissue (Camper’s fascia) and a deep layer of collagen and elastic tissue providing stronger support (Scarpa’s fascia). The superficial fascia is homologous with Scarpa’s fascia of the anterior abdominal wall and may be considered as a single unit.4 The superficial fascia in four-legged animals is said to provide a firmer support than that found in bipeds. The support of the superficial fascia may partly explain why varicose veins affect humans but not quadrupeds.
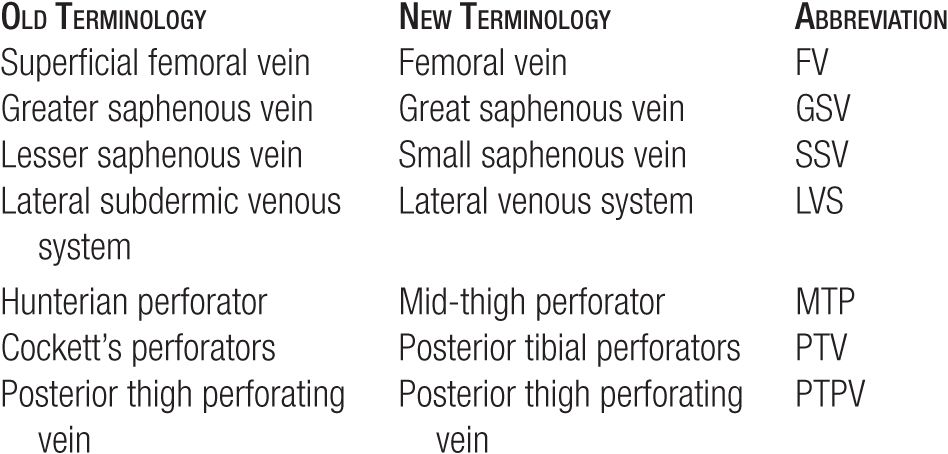
The superficial fascia covers and supports the saphenous trunks (Figure 2-1), but tributaries to the saphenous veins are superficial to this fascia. Because they are not within its support, tributaries to the GSV are usually more grossly dilated than the GSV trunk itself, even in the presence of proximal high venous pressure.5
![]() FIGURE 2-1 Superficial fascia covers the saphenous trunk of the great saphenous vein (GSV) seen in this longitudinal view under Duplex ultrasound. A valve is present in the central dilatation; arrows indicate the fascia.
FIGURE 2-1 Superficial fascia covers the saphenous trunk of the great saphenous vein (GSV) seen in this longitudinal view under Duplex ultrasound. A valve is present in the central dilatation; arrows indicate the fascia.
Although the preceding description seems simple, connections between the superficial and deep venous systems and their fascial coverings are actually very complicated. Detailed anatomic studies by Raivio6 show an extreme variability in the connections between deep and superficial systems.
The Deep Venous System
No matter what pathway is taken, all venous blood is eventually received by the deep venous system on its way back to the right atrium of the heart. In most cases, there are five major named branches to the deep venous system of the lower extremity: three below the knee and two above the knee. The principal deep venous trunk of the leg is called the popliteal vein (PV) from below the knee until it passes upward and anteriorly through the adductor canal in the distal thigh. The PV then changes its name to the femoral vein (FV) (formerly superficial femoral) for the remainder of its course in the thigh.
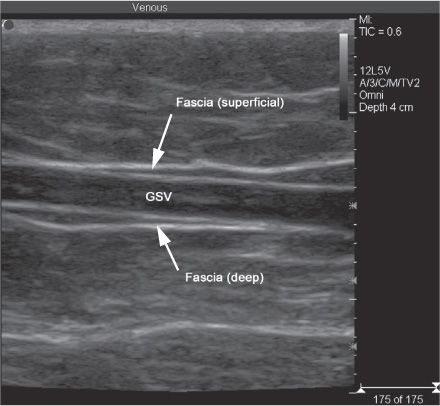
DEEP VEINS OF THE CALF In the lower leg, there are three groups of deep veins: the anterior tibial vein (ATV), draining the dorsum of the foot, the posterior tibial vein (PTV) (Figure 2-2), draining the sole of the foot, and the peroneal vein, draining the lateral aspect of the foot. From the ankle, the ATV passes upward anterolaterally to the interosseous membrane, the PTV passes upward posteromedially beneath the medial edge of the tibia, and the peroneal vein passes upward posteriorly through the calf. Venous sinusoids within the calf muscle coalesce to form soleal and gastrocnemius intramuscular venous plexi, which usually join the peroneal vein in the mid-calf. In most patients, each one of these is actually a pair of veins flanking an artery of the same name; thus, there are actually six named deep veins below the knee in a typical patient (Figures 2-3 and 2-4). Just below the knee, the ATV and PTVs join with the peroneal veins at the popliteal trifurcation to become the single large PV.
![]() FIGURE 2-2 Posterior tibial veins. Duplex image of posterior tibial veins (blue) between which the posterior tibial artery lies. Abnormalities in flow can be easily discerned by this method. (Digital image from Sonos 1000, Agilent Technologies, formerly Hewlett Packard.)
FIGURE 2-2 Posterior tibial veins. Duplex image of posterior tibial veins (blue) between which the posterior tibial artery lies. Abnormalities in flow can be easily discerned by this method. (Digital image from Sonos 1000, Agilent Technologies, formerly Hewlett Packard.)
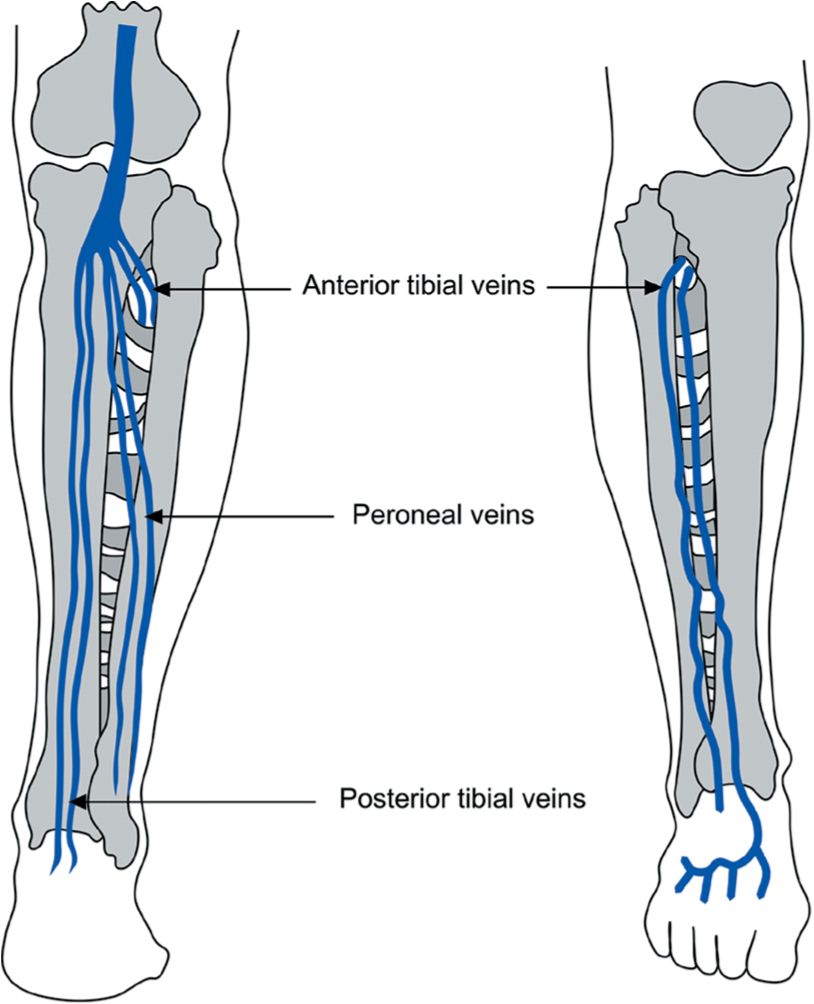
![]() FIGURE 2-3 Deep veins of the calf, anterior and posterior views.
FIGURE 2-3 Deep veins of the calf, anterior and posterior views.
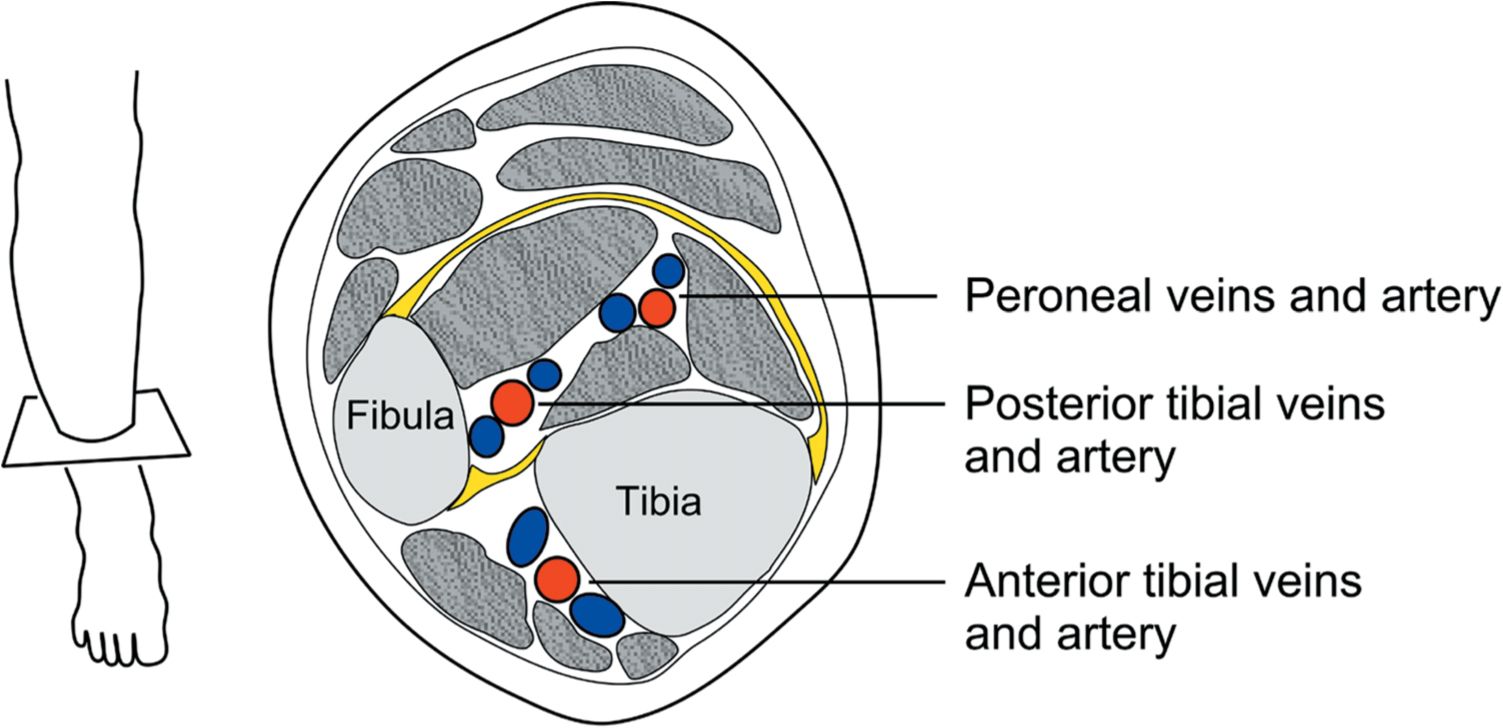
![]() FIGURE 2-4 Deep veins of the calf seen in cross section.
FIGURE 2-4 Deep veins of the calf seen in cross section.
DEEP VEINS OF THE THIGH From the trifurcation, the PV courses proximally behind the knee and then passes anteromedially in the distal thigh into the adductor canal. This canal carries the FV and artery from a posterior position at the knee all the way to an anterior position just below the femoral triangle at the groin. The adductor canal is also known as the sartorial canal and (especially at its upper extent) may be referred to as the canal of Hunter.
As the PV passes above the knee, it changes its name to the FV, the largest and longest deep vein of the lower extremity. This important deep vein is sometimes incorrectly referred to as the “superficial femoral vein” in an attempt to distinguish it from the profunda femora, or DFV. The DFV is a short, stubby vein that usually has its origin in terminal muscle tributaries within the deep muscles of the lateral thigh but may communicate with the PV in up to 10 percent of patients. In the proximal thigh, the FV and the DFV join together to form the common femoral vein (CFV), which passes upward above the groin crease to become the iliac vein (Figure 2-5).
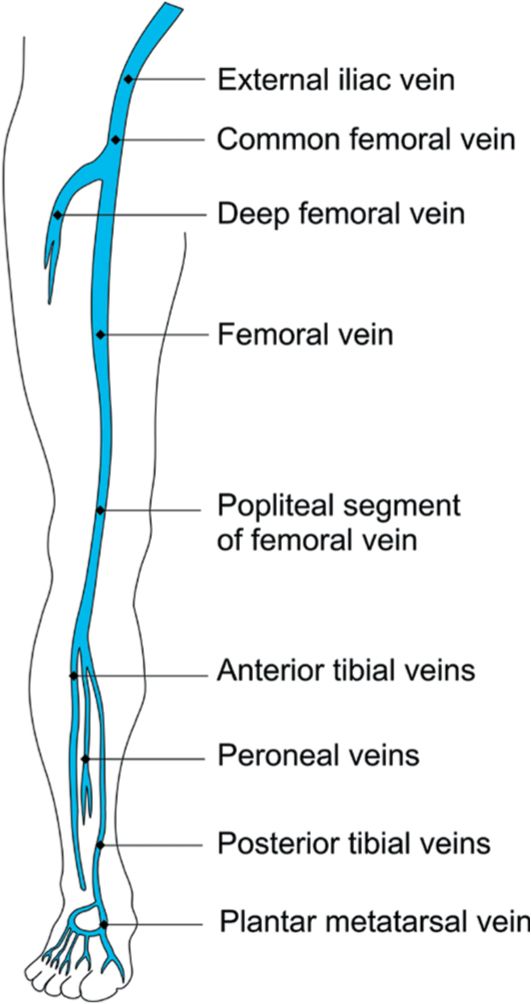
![]() FIGURE 2-5 Major deep veins of the leg.
FIGURE 2-5 Major deep veins of the leg.
It cannot be overemphasized that the misleading and incorrect term “superficial femoral vein” should not be used, as the FV is a deep vein and is not part of the superficial venous system. The incorrect term does not appear in any definitive anatomic atlas, yet has come into common use in vascular laboratory and radiology practice.7 Because inexperienced clinicians often have the impression that thrombus in the “superficial femoral vein” is a superficial rather than deep vein thrombosis, they may view such thrombus as less of a threat to the patient than it actually is. Confusion arising from use of the inappropriate name thus continues to be responsible for many cases of clinical mismanagement and even death. Fortunately, the name has officially changed from superficial femoral to FV.
Superficial Venous System
The superficial venous system (Figure 2-6) includes three major divisions: the great saphenous, the small saphenous, and the lateral venous system (LVS, previously known as the LSVS). Each of these divisions contains multiple collateral veins (accessory, anastamotic, tributary, or communicating veins) and multiple points of connection that normally carry flow from the superficial to the deep system (perforating veins). Every point of connection between the superficial and the deep system is a potential point of leakage that can give rise to retrograde flow. Even tiny, unnamed veins without important connections can become dilated and tortuous when exposed to elevated venous pressures, and it is useless to pursue the identification of all but the major points of reflux. Despite the multiple variations, the vast majority of superficial vessels do belong to one of these three major divisions. The largest of these divisions is the great saphenous system (Figure 2-7).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


