Upper lid blepharoplasty is a common procedure for restoration and rejuvenation of the upper eyelids that can be performed safely and reliably. Understanding the anatomy and aging process of the brow–upper lid aesthetic unit along with properly assessing the excesses and deficiencies of the periorbital region helps to formulate an appropriate surgical plan. Volume deficiency in the aging upper lid may require corrective augmentation. Preexisting asymmetries and ptosis need to be identified and discussed before surgery. Standardized photography along with a candid discussion regarding patients’ desired outcomes and realistic expectations are essential to a successful outcome.
Key points
- •
The brow and upper lid are assessed as a continuous aesthetic unit.
- •
Upper lid aging is due to tissue descent and laxity as well as volumetric changes associated with bony orbital remodeling and the involution of orbital fat.
- •
Graded approach to upper lid blepharoplasty is important with restoration or augmentation of volume to avoid an unnatural, hollowed appearance.
- •
Careful preoperative planning as well as understanding and managing patients’ expectations are keys to a successful postoperative outcome.
Upper lid blepharoplasty is one of the most common facial plastic surgeries performed, which can be done for functional or aesthetic indications. Successful upper lid blepharoplasty requires the surgeon to develop a clear understanding of the relevant periorbital anatomy, especially the relationship between the brow and the upper lid, as well as the anatomic changes that occur during the aging process. Current thoughts on eyelid aging involve not only tissue descent and laxity but also total orbital volume loss. This volume loss involves both bone and soft tissue around the eye and results in brow descent, especially temporally, along with lateral hooding of the upper lid skin. The loss of brow and eyelid volume creates relative skin excess in the upper lid contributing to dermatochalasis.
Traditionally, blepharoplasty techniques focused on the excision of excessive eyelid skin, muscle, and fat. However, these subtractive techniques may result in eyelids that appear hollow and unnatural with a deep superior sulcus and excessive tarsal platform show. Contemporary approaches to upper lid blepharoplasty have evolved with more appropriate tissue resection and repositioning, aimed at restoration of the upper eyelids to appear balanced and youthful. The ultimate goal of upper lid blepharoplasty is the restoration and rejuvenation of youthful upper eyelid topography.
Periorbital anatomy
Brow Anatomy
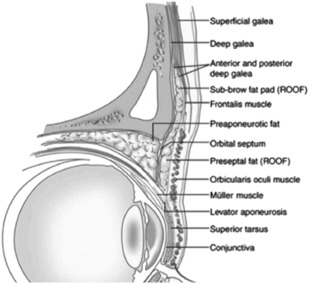
Understanding the upper eyelid anatomy and its relationship with the brow is crucial to performing a successful upper lid blepharoplasty. The upper lids are assessed as a continuous aesthetic unit with the brow given the intricate interaction between the brow and upper eyelid. The brow is composed of hair-bearing skin and soft tissue that cover the superior orbital rim. Deep to the hair-bearing skin lies the corrugator supercilii muscle, which acts as a brow depressor along with the procerus muscle medially at the glabella and the orbicularis oculi muscle interdigitating through the area. The frontalis muscle, absent laterally, acts as the lone brow elevator. The subciliary brow transitions into the upper eyelid at the arcus marginalis on the superior orbital rim. Deep to the orbital orbicularis muscle and frontalis muscle, the retro-orbicularis oculi fat (ROOF) fat pad provides fullness of the brow and upper lid region ( Fig. 1 ). Traditionally, resection of the ROOF was considered an important adjunct in upper lid blepharoplasty. However, ROOF sculpting enhances an atrophic appearance to the upper lid, which accentuates hollowing seen with aging. Modern blepharoplasty approaches have generally shifted focus to retaining or even augmenting volume in this region.
Upper Lid Anatomy
The upper eyelid is often divided into anterior and posterior lamellae with the orbital septum separating the two compartments. The anterior lamella is composed of the skin and orbicularis oculi muscle. The skin of the upper eyelid is very thin and contains few sebaceous and adnexal structures. The orbicularis oculi muscle lies immediately deep to the skin with no intervening subcutaneous fat. The orbicularis muscle is further divided into the orbital, preseptal, and pretarsal segments. The orbital component is the outer most portion of the muscle and lies over the superior orbital rim and deep to the brow. The orbital orbicularis muscle fibers interlink with the corrugator supercilii acting as a brow depressor and opposing the frontalis muscle superiorly. The orbital orbicularis lies unopposed laterally at the tail of the brow contributing to the involutional descent of the lateral brow. The preseptal portion of the orbicularis lies between the brow and tarsal region superficial to the orbital septum, and the pretarsal orbicularis directly overlies the tarsus. The preseptal and pretarsal components are often referred to as the palpebral portion of the orbicularis muscle and are important in active tear drainage and involuntary blinking.
The orbital septum is a thin adventitial layer of connective tissue that separates the anterior and posterior lamellae. The orbital septum lies deep to the preseptal orbicularis oculi muscle and originates from the arcus marginalis at the superior orbital rim, fusing onto the levator aponeurosis and tarsal plate inferiorly. It acts as a retaining layer for the orbital fat and is an important anatomic barrier and surgical landmark during blepharoplasty.
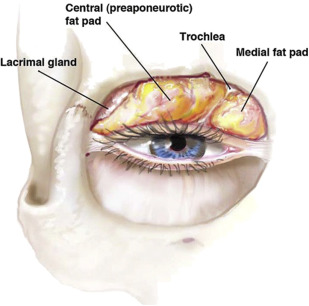
The orbital fat is located immediately posterior to the orbital septum and anterior to the levator aponeurosis. There are 2 fat compartments within the upper eyelid: the nasal or medial fat pad and central or middle fat pad ( Fig. 2 ). A layer of thin fibrous sheet and the trochlea of superior oblique separate the two compartments. The nasal fat pad is whiter and denser than the central fat pad and can help distinguish the origin of the fat during blepharoplasty. The central fat is also called the preaponeurotic fat as it overlies the levator aponeurosis. Identifying the preaponeurotic fat in upper lid blepharoplasty helps orient the surgeon to the location of the levator aponeurosis and helps prevent unintended injury to the upper lid elevator. The lateral third of the orbit is occupied by the lacrimal gland, which normally lies within the lacrimal fossa. Lacrimal gland prolapse, however, is commonly seen with aging. The lacrimal gland must not be mistaken for fat and inadvertently excised during surgery. In the functional blepharoplasty population, moderate gland prolapse is noted in up to 60% of patients, which may be corrected with suture repositioning.
The posterior lamella is composed of the levator palpebrae superioris and levator aponeurosis (superiorly), tarsus (inferiorly), Müller muscle, and conjunctiva. The levator palpebrae superioris and its associated aponeurosis is the main retractor of the upper eyelid. The levator aponeurosis inserts onto the inferior two-thirds of the tarsus with anterior fibers attaching to the orbicularis muscle and skin forming the supratarsal crease. The Müller muscle is a sympathetically innervated smooth muscle that acts as an accessory lid elevator originating from the undersurface of the levator muscle at the muscle-aponeurotic junction and inserting into the superior tarsus. The Müller muscle provides 1.5 to 2.0 mm of upper lid elevation. The tarsus is a dense band of fibrous connective tissue that acts as the structural support along the inferior portion of the eyelid. The upper lid tarsal plate measures approximately 10 to 12 mm in height at the midpupillary line and tapers across its 30-mm width. The palpebral conjunctiva is tightly adherent to the tarsus and Müller muscle and apposes the globe, wiping the cornea with each blink.
Periorbital anatomy
Brow Anatomy
Understanding the upper eyelid anatomy and its relationship with the brow is crucial to performing a successful upper lid blepharoplasty. The upper lids are assessed as a continuous aesthetic unit with the brow given the intricate interaction between the brow and upper eyelid. The brow is composed of hair-bearing skin and soft tissue that cover the superior orbital rim. Deep to the hair-bearing skin lies the corrugator supercilii muscle, which acts as a brow depressor along with the procerus muscle medially at the glabella and the orbicularis oculi muscle interdigitating through the area. The frontalis muscle, absent laterally, acts as the lone brow elevator. The subciliary brow transitions into the upper eyelid at the arcus marginalis on the superior orbital rim. Deep to the orbital orbicularis muscle and frontalis muscle, the retro-orbicularis oculi fat (ROOF) fat pad provides fullness of the brow and upper lid region ( Fig. 1 ). Traditionally, resection of the ROOF was considered an important adjunct in upper lid blepharoplasty. However, ROOF sculpting enhances an atrophic appearance to the upper lid, which accentuates hollowing seen with aging. Modern blepharoplasty approaches have generally shifted focus to retaining or even augmenting volume in this region.
Upper Lid Anatomy
The upper eyelid is often divided into anterior and posterior lamellae with the orbital septum separating the two compartments. The anterior lamella is composed of the skin and orbicularis oculi muscle. The skin of the upper eyelid is very thin and contains few sebaceous and adnexal structures. The orbicularis oculi muscle lies immediately deep to the skin with no intervening subcutaneous fat. The orbicularis muscle is further divided into the orbital, preseptal, and pretarsal segments. The orbital component is the outer most portion of the muscle and lies over the superior orbital rim and deep to the brow. The orbital orbicularis muscle fibers interlink with the corrugator supercilii acting as a brow depressor and opposing the frontalis muscle superiorly. The orbital orbicularis lies unopposed laterally at the tail of the brow contributing to the involutional descent of the lateral brow. The preseptal portion of the orbicularis lies between the brow and tarsal region superficial to the orbital septum, and the pretarsal orbicularis directly overlies the tarsus. The preseptal and pretarsal components are often referred to as the palpebral portion of the orbicularis muscle and are important in active tear drainage and involuntary blinking.
The orbital septum is a thin adventitial layer of connective tissue that separates the anterior and posterior lamellae. The orbital septum lies deep to the preseptal orbicularis oculi muscle and originates from the arcus marginalis at the superior orbital rim, fusing onto the levator aponeurosis and tarsal plate inferiorly. It acts as a retaining layer for the orbital fat and is an important anatomic barrier and surgical landmark during blepharoplasty.
The orbital fat is located immediately posterior to the orbital septum and anterior to the levator aponeurosis. There are 2 fat compartments within the upper eyelid: the nasal or medial fat pad and central or middle fat pad ( Fig. 2 ). A layer of thin fibrous sheet and the trochlea of superior oblique separate the two compartments. The nasal fat pad is whiter and denser than the central fat pad and can help distinguish the origin of the fat during blepharoplasty. The central fat is also called the preaponeurotic fat as it overlies the levator aponeurosis. Identifying the preaponeurotic fat in upper lid blepharoplasty helps orient the surgeon to the location of the levator aponeurosis and helps prevent unintended injury to the upper lid elevator. The lateral third of the orbit is occupied by the lacrimal gland, which normally lies within the lacrimal fossa. Lacrimal gland prolapse, however, is commonly seen with aging. The lacrimal gland must not be mistaken for fat and inadvertently excised during surgery. In the functional blepharoplasty population, moderate gland prolapse is noted in up to 60% of patients, which may be corrected with suture repositioning.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





