Nevus lipomatosus846
Piezogenic pedal papules847
Lipoblastoma847
Lipofibromatosis848
Hemosiderotic fibrolipomatous tumor848
Pseudolipomatosis cutis848
Lipoma and lipomatosis848
Angiolipoma849
Adenolipoma850
Chondroid lipoma850
Ossifying lipoma851
Sclerotic (fibroma-like) lipoma851
Spindle-cell lipoma851
Pleomorphic lipoma852
Hibernoma853
Atypical subcutaneous fatty tumors853
Liposarcoma853
The role of subcutaneous fat and the consequences of its increase and decrease have received little attention in the dermatological literature until comparatively recently.1. and 2. There are two types of adipose tissue, white and brown, that have different roles in energy metabolism. Most tumors of fat are derived from white adipocytes, but the rare hibernoma is derived from brown adipose tissue. The lipoma is by far the most common tumor of fat.
In addition to mature adipocytes, subcutaneous and soft tissue fat contain an admixture of small blood vessels, nerve tissue, fibroblasts, and adipocyte precursor cells known as preadipocytes. 2 Each of these constituent cells may give rise to tumors.
Recently, Resnik and Kutzner have drawn attention to an earlier observation that may be misinterpreted by pathologists unaware of this change: 3 both normal adipocytes and fat cells found in lipomas and liposarcomas may have an intranuclear vacuole, which had been called ‘Lochkern’ (German; Loch = hole and Kern = nucleus). Variants of this phenomenon have been described. 3
The tumors of fat are a histologically diverse group. Fortunately, most have well-established diagnostic criteria and present no difficulty in diagnosis. However, there are three benign fatty tumors – spindle-cell lipoma, sclerotic lipoma, and pleomorphic lipoma – which may cause diagnostic problems, sometimes leading to a mistaken diagnosis of liposarcoma.
Lipomatous tumors of different types appear to harbor CD34+ interstitial dendritic cells. Clonal expansion of the CD34+ cells may account for the development of spindle-cell lipomas and the spindle-cell component in some dedifferentiated liposarcomas.4. and 5.
Most tumors of fat, excluding angiolipomas, have specific aberrations of their karyotype. On this basis, it has been suggested that angiolipomas (see below) are not true lipomas, but a hamartoma of blood vessels and fat. 6
NEVUS LIPOMATOSUS
Nevus lipomatosus, also known by the complicated term ‘nevus lipomatosus cutaneus superficialis (Hoffmann–Zurhelle)’,7. and 8. is a rare type of connective tissue nevus characterized by the presence of mature adipose tissue in the dermis. It is found as plaques or solitary lesions, or in an extremely rare generalized form.
The plaque type has aggregations of flesh-colored or yellow papules and nodules which are present at birth, or which develop in the first two decades of life. 9 There is a predilection for the pelvic girdle, particularly the gluteal region. Other sites, such as the face and scalp, are rarely involved.10.11.12. and 13. Lesions are usually unilateral, and sometimes in a linear or zosteriform arrangement. The surface of most lesions is smooth, although it may be verrucous or dimpled. 14 Surface comedones have been noted occasionally. Lesions usually develop insidiously, but later become reasonably stable. There is one report with an associated chromosomal abnormality, a deletion of 2p24. 15
The colocalization of nevus lipomatosus and lipedematous scalp (see below) has been reported. 13
The solitary form consists of isolated papules or nodules, anywhere on the body, but with a predilection for the trunk. 16 They may not appear until the fifth decade. They usually have a broader base than the common skin tag (acrochordon), but there are some who doubt the existence of the solitary form, preferring to regard them as skin tags or ‘pedunculated lipofibromas’.7. and 17.
There are reports of more generalized body involvement with a markedly folded skin surface (‘Michelin man’ appearance).18.19. and 20. The generalized form needs to be distinguished from the abnormal fat distribution, which occurs particularly in the buttock region, in congenital disorders of glycosylation (CDG). 21 Folds of fat hang down from the buttocks in CDG-1a (OMIM 212065). 21
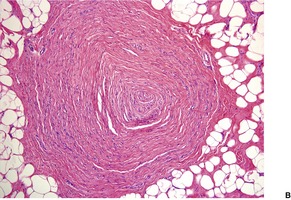
Histopathology7. and 22.
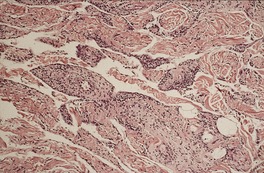
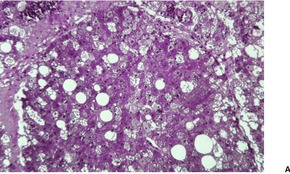
The basic abnormality is the presence of varying amounts of mature adipose tissue in the dermis, often not connecting with the fat of the underlying subcutis. The fat can constitute from less than 10% to 70% of the lesion. When there is only a small amount of fat, it is usually localized around the subpapillary blood vessels. Some authors have indicated a requirement for fat to be present in the papillary dermis in solitary cases to distinguish them from skin tags, 22 but this feature is not always present, even in the plaque variant (Fig. 35.1).
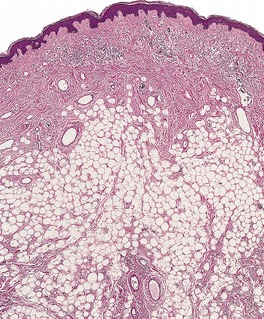 |
| Fig. 35.1 Nevus lipomatosus. Mature fat cells replace much of the dermis. Sometimes they extend to the undersurface of the epidermis. (H & E) |
There are also abnormalities in the other connective tissue components of the dermis, 7 including some thickening of the collagen bundles. 23 In about half of the cases the deeper elastic tissue is increased, although there may be a reduction in elastic fibers superficially. There is an increase in the number of fibroblasts in the papillary dermis, and also of mononuclear cells, including mast cells, elsewhere in the dermis. Blood vessels are increased in the papillary dermis, and subjacent to this there may be some ectatic vessels. In one case, the vessels were so pronounced that a diagnosis of an associated angiokeratoma was made (on biopsy). 24 Vessels are also increased in the ectopic dermal fat. Pilosebaceous follicles are often reduced, but in one report they were hypertrophic. 25 The presence of folliculosebaceous cystic hamartomas and, in one case, a dermoid cyst within a giant nevus lipomatosus is difficult to explain on histogenetic grounds.26. and 27.
The epidermal changes are variable. There is often some undulation with acanthosis and even mild papillomatosis, 28 and there may be mild hyperpigmentation of the basal layer. The changes may resemble those of an epidermal nevus. Dilated follicular ostia will be present, if there are comedones clinically.
Nevus lipomatosus should be distinguished from old nevocellular nevi, in which there may be large amounts of fat and sometimes only small areas of nevus cells. Focal dermal hypoplasia also has fat in the dermis, but in this condition there is extreme attenuation of collagen as well as vast clinical differences. The dermal variant of spindle-cell lipoma has more spindle-shaped cells present as well as a fibromucinous stroma.
PIEZOGENIC PEDAL PAPULES
In piezogenic pedal papules there are usually multiple small papulonodules on the heels31.32.33.34.35. and 36. which have a tendency to disappear when pressure is relieved from the heels. 36 Although most are painless and small, 37 there are a few reports of a painful variant.32.33.34. and 38. This entity has recently been reported in one-third of a group of patients with Ehlers–Danlos syndrome and in the Prader–Willi syndrome.35. and 39.
Piezogenic pedal papules are thought to represent pressure-induced herniations of the subcutaneous fat through acquired or inherited defects in the connective tissue of the heel.35.40. and 41.
Similar lesions (piezogenic wrist papules) have been reported on the wrist. 42 A case of piezogenic palmar papules has been reported. 43 It was due to a subcutaneous lipoma that herniated into the dermis at several points. 43
Infantile pedal papules, congenital adipose plantar nodules, 44congenital fibrolipomatous hamartoma45.46.47. and 48. all refer to the same entity (OMIM 609808), which differs slightly from piezogenic pedal papules. Infantile pedal papules present at birth or in infancy as painless, symmetric nodules on the medial aspect of the heel. 49 Autosomal dominant inheritance was present in three family members from two generations. 50 Most cases are sporadic. In a recent study, they were found in 5.9% of newborns and 39.4% of infants. 51 They were not biopsied.
Histopathology33. and 34.
There is thickening of the dermis in the painful variant, with loss of the normal small fat compartments in the lower dermis and subcutis. These appear to coalesce as a result of degeneration of the thin fibrous septa.33.35. and 36. There may also be protrusion of these enlarged fat lobules into the dermis. 34 In infantile pedal papules, reported under several names (see above), there are well-defined lobules of mature fat in the mid and deep dermis, mostly in a periadnexal distribution.44. and 45. Mucinous deposits are often present at the periphery of the lesion and within fat lobules. 52 Similar histological findings (clusters of adipocytes around eccrine ducts) are present as a consequence of fibrous amniotic bands producing strictures of the lower legs. 53
LIPOBLASTOMA
Lipoblastoma is a rare, benign tumor of infants and young children, thought to be related to fetal white fat.54.55.56.57. and 58. It may also occur in adolescents and young adults. 59 Most lipoblastomas occur on the proximal extremities, trunk, and head and neck. 60 Rare sites include the scrotum and vulva.60.61. and 62. Some earlier reports of liposarcoma in infants probably included examples of this entity. 63 Chung and Enzinger delineated a circumscribed, usually superficial type, and a less common diffuse form, often in the deeper soft tissues, analogous to diffuse lipomatosis. 56 In one study of 14 cases, 6 were of the circumscribed type and 8 were diffuse and ill defined (lipoblastomatosis), 64 while in another study of 25 cases, 11 were circumscribed (discrete) and 14 were diffuse. 65 Lipoblastoma/lipoblastomatosis behaves in a benign fashion, although local recurrence sometimes occurs. 65 No metastases have been reported.
Cytogenetic studies have shown that the majority of lipoblastomas have rearrangements of 8q11–13, with similar numbers showing polysomy of chromosome 8.59. and 66. Many other abnormalities have been reported, including cases with a complex or even normal karyotype.60. and 67. The altered gene is PLAG1, an oncogene which encodes a zinc-finger protein involved in transcriptional regulation.60. and 67. The oncogenic capability of PLAG1 is mediated, in part, by the IGF-II mitogenic signaling pathway. 68 This gene also plays a role in other human tumors, such as hepatoblastoma and acute myeloid leukemia. 68
Lipoblastomas are light yellow to tan-yellow tumors, averaging 5 cm in greatest diameter, with focal gelatinous areas on the cut surface. Larger variants have been reported. 60 They are usually thinly encapsulated.
The treatment of choice for the localized variant is complete yet conservative surgical excision, 58 while for the diffuse variant complete excision may not be possible. Local recurrence has been reported in up to 22% of patients, especially with incompletely excised lesions of the lipoblastomatosis (diffuse) subtype. 69
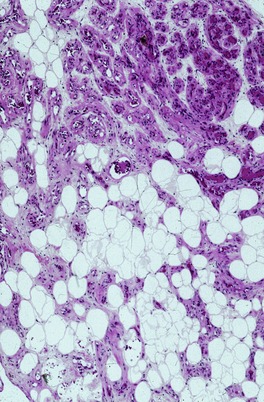
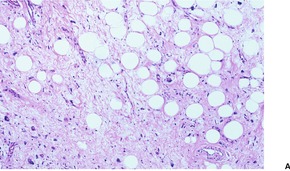
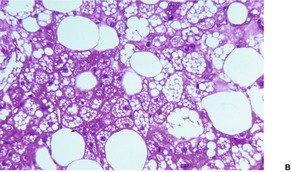
Histopathology56
The tumor is lobulated, with thin, well-vascularized connective tissue septa. The lobules contain mature fat cells, intermingled with spindle-shaped mesenchymal cells and various types of lipoblasts. These cells may be univacuolated, resembling signet-ring cells, multivacuolated, or granular resembling hibernoma cells (Fig. 35.2). In contrast to liposarcoma, there are no mitoses or nuclear atypia in the lipoblasts. There is often a plexiform capillary pattern in the lobules, and patchy myxoid stroma containing mucopolysaccharides. The myxoid matrix is sometimes a predominant feature. 59 In one report, the cells stained positively for vimentin, but not for CD34, smooth muscle actin, and desmin. 61 Other reports have shown that the stellate to spindled cells within the myxoid matrix are positive for S100 protein, CD10, desmin, and CD34. 70
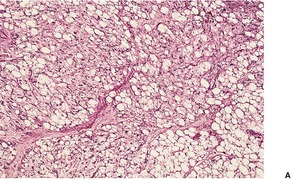 |
 |
| Fig. 35.2 Lipoblastoma. (A) The tumor is composed of mature fat cells, spindle-shaped mesenchymal cells, and a few cells with granular cytoplasm. (B) A higher power view of the same lesion. (H & E) |
LIPOFIBROMATOSIS
Lipofibromatosis is a rare pediatric neoplasm, with a propensity for the hands and feet, which occurs in the subcutis and deep soft tissues. 73 It may be present at birth. Similar cases have been diagnosed in the past as infantile fibromatosis, fibrous hamartoma of infancy, and fibrosing lipoblastoma. Regrowth or persistence of the tumor is common following incomplete excision. 73
Histopathology
There is abundant adipose tissue, typically comprising more than 50% of the specimen, dissected by thickened septa containing a spindled fibroblastic element. 73 These cells sometimes show a fascicular growth pattern and limited mitotic activity. Small collections of univacuolated cells are often present at the interface between the fat and the fibroblastic element. Rare pigmented cells have been described. 73
HEMOSIDEROTIC FIBROLIPOMATOUS TUMOR
This tumor, reported by Browne and Fletcher in 2006 (with English spelling of two of the words in the title), 74 is the same entity as a hemosiderotic fibrohistiocytic lipomatous lesion reported a few years earlier. 75 Although originally regarded as reactive in nature (sometimes to trauma), it is now thought to be neoplastic because of its infiltrative border and local recurrence in some cases. No metastasis has been reported. 74
Most cases have been reported in the ankle/foot region, but unlike lipofibromatosis, there is a predilection for middle-aged and elderly individuals. 74 Lesions range in size from 1 to 13 cm. They are situated in the superficial soft tissues/subcutis. Grossly the lesions are fatty/gelatinous or lipoma-like.
Although Folpe and Weiss have regarded this lesion as a precursor of pleomorphic hyalinizing angiectatic tumor, 76 this concept is not supported by Browne and Fletcher. 74
Histopathology
This tumor has varying proportions of mature adipocytes and fibroblastic spindle cells, associated with usually abundant deposits of hemosiderin, found predominantly in macrophages within the spindle-cell component. 74 The adipocytic component has a partly lobular configuration which is traversed by spindle-cell septa of variable size. 77 Often the spindle cells form nodules within the fat. The spindle cells are arranged in fascicles and there may be focal myxoid change in this component. Sometimes the spindle cells infiltrate the fat in a honeycomb pattern, reminiscent of dermatofibrosarcoma protuberans. 74
Inflammatory cells are scattered through each lesion. They are mainly lymphocytes and plasma cells with a few mast cells and eosinophils. Osteoclastic giant cells are often present. The hemosiderin is largely confined to the cellular fibrous septa and spindle-cell nodules.
Of the nine cases tested in the series reported by Browne and Fletcher, seven showed strong positivity for CD34 in the spindle-cell component. In all 10 cases examined, the spindle cells were negative for SMA, desmin, CD68, and S100 protein. 74
PSEUDOLIPOMATOSIS CUTIS
The term ‘pseudolipomatosis cutis’ was coined by Trotter and Crawford for the incidental finding of grouped and coalescent spaces in the dermis resembling fatty infiltration. 78 Similar changes have been reported in acrodermatitis chronica atrophicans (see p. 580) and in a case of psoriasis (see p. 79). 79 Although Trotter and Crawford regarded these spaces as artifactual, subsequent correspondence refuted this suggestion in favor of a prelymphatic origin. 79
LIPOMA AND LIPOMATOSIS
Lipomas are relatively common, usually asymptomatic, subcutaneous tumors with a predilection for the upper trunk, upper extremities, thighs, and neck of individuals in the fifth and sixth decades. 80 Lesions on the finger are very rare.81.82. and 83. A deep variant arising on the forehead has been described. 84 Intramuscular lipomas may occur at other sites. 85 Lipomas account for 90% or more of tumors of fat seen in most laboratories. They are soft, often mobile, encapsulated tumors of varying size, but averaging 3–5 cm in diameter. ‘Giant’ variants have been recorded. 86 Blunt trauma has been suggested as an etiological factor in some cases, but pseudo-lipomas from prolapse of fat may be difficult to distinguish from true lipomas in these circumstances.87. and 88. Multiple lipomas have developed after total body electron beam therapy. 89 Ectopic axillary breast tissue may mimic a lipoma. 90
There are several distinct clinical syndromes in which disfiguring masses of mature adipose tissue develop in the subcutaneous tissues. They are discussed in some detail by Allen. 91 In benign symmetric lipomatosis (multiple symmetric lipomatosis/Madelung’s disease/Launois–Bensaude syndrome – OMIM 151800), the tumors develop on the neck, back, and upper trunk, with a predilection for middle-aged men.92.93.94.95.96.97. and 98. Variants involving the hands, 99 the thighs, 100 or the feet101 have been reported. The distinction between obesity and localized (zonal) variants of the buttocks and thighs is often problematic in females. 102 Familial cases have also been recorded, but no pattern of inheritance has been delineated. Some cases have been associated with the mitochondrial DNA syndromes. 103 Various metabolic abnormalities may occur in this condition,104. and 105. and there is sometimes alcohol-related liver disease, suggesting that alcoholism may be a trigger.102.106.107.108. and 109. A case with lipoatrophy of the face, mimicking HAART-related lipodystrophy (see below), has been reported. 110 In familial multiple lipomatosis,106.111.112. and 113. multiple discrete, usually asymptomatic, lipomas develop on the forearms, trunk, and thighs in the third decade. Non-symmetrical lesions may be present. 114 An autosomal dominant inheritance has been proposed, despite the predominance in males. The gene map locus is 12q14.3. Reciprocal translocations have been reported in the lipomas that develop in familial multiple lipomatosis (OMIM 151900). The masses are encapsulated and vary from a few millimeters to 5 cm or more in diameter. In adiposis dolorosa (Dercum’s disease – OMIM 103200) there are painful, circumscribed or diffuse fatty deposits with a predilection for the lower legs, abdomen, and buttocks.115. and 116. There may be obesity, weakness, and mental disturbances. Familial cases related to an autosomal dominant gene with variable expressivity have been reported.117. and 118. Juxta-articular fatty deposits, resembling those seen in adiposis dolorosa, have been reported in a patient receiving long-term treatment with high doses of corticosteroids. 119Diffuse lipomatosis63.120.121. and 122. consists of infiltrating masses of mature adipose tissue, extensively involving part of a limb or the trunk, with onset before 2 years of age. It has been associated with tuberous sclerosis. 120 In encephalocraniocutaneous lipomatosis123.124.125. and 126. there are subcutaneous lipomas on the scalp with overlying alopecia, as well as cranial and ocular abnormalities. The cutaneous component has been called ‘nevus psiloliparus’.127.128. and 129. Infiltrating lipoma of the face130 is another variant of this hamartomatous condition. The term has also been used for intermuscular and intramuscular lipomas. 131 Other variants of infiltrating lipoma occur. 132Lipedematous scalp refers to a thickening of the subcutaneous fat of the scalp, leading to a clinically thickened and soft scalp.133. and 134. It may present as an alopecia (see p. 431).
The use of protease inhibitors in the treatment of human immunodeficiency virus type 1 (HIV-1) may be associated with several abnormalities of fat including subcutaneous lipomas, 135 angiolipomas, 136 peripheral lipodystrophy (see p. 471), and benign symmetrical lipomatosis. 135 Multiple lipomas have developed in a patient undergoing highly active anti-retroviral therapy (HAART) that did not include a protease inhibitor. 137
Nearly a half of all lipomas have an abnormal karyotype, characterized by rearrangements of three different chromosome regions: 12q14–q15, 6p21, and 13q12–q14. Translocations involving the long arm of chromosome 12 and chromosome 3 (band q27–28) are a common finding, but other chromosome bands may be involved in the translocation. 138 At the molecular level, 12q14–q15 rearrangements affect the high-mobility-group (HMG) protein gene HMGIC. Other mesenchymal tumors share abnormalities of this or related genes. 138
Although surgical extirpation is the usual method of treatment, liposuction and the injections of phosphatidylcholine have also been used.139.140. and 141. Dramatic reduction in the size of a lipoma has occurred in a patient commenced on statin therapy. 142 In adiposis dolorosa (Dercum’s disease) intravenous lidocaine, and low-dose, daily prednisolone have helped in some cases. Improvement has been reported with the combined use of infliximab and methotrexate. 143 Surgical debulking has produced an acceptable cosmetic result in a patient with lipedematous alopecia. 144
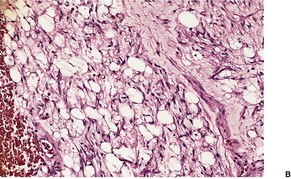
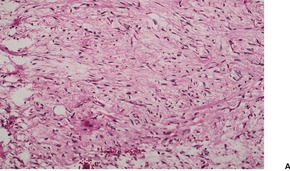
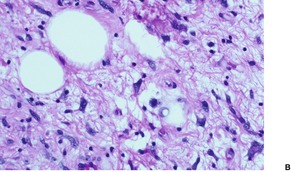
Histopathology
Lipomas are composed of sheets of mature fat dissected by thin, incomplete fibrous septa containing a few blood vessels. A fibrous capsule is present. Variants with increased stromal fibrous tissue (fibrolipomas) are found. In neural fibrolipoma (fibrolipomatous hamartoma of nerve, neural lipofibromatous hamartoma145), fibrofatty tissue surrounds and infiltrates a nerve and/or its small branches (Fig. 35.3).146. and 147. If blood vessels constitute more than 5% of the mass, the lesion is best regarded as an angiolipoma (see below). Eccrine sweat ducts are rarely present. Such variants have been termed adenolipomas (see below). The admixture of smooth muscle and fat constitutes a myolipoma. Rarely, the lipomatous component is mildly atypical. 148 A unique case with myxoid change and synovial metaplasia has been reported. 149 Membranous fat necrosis is another rare secondary change. 150 Abundant fat may be present in some mixed tumors of the skin (chondroid syringoma). 151
 |
 |
| Fig. 35.3 (A) Neural fibrolipoma (fibrolipomatous hamartoma of nerve). (B) Mature fat surrounds and to a lesser extent infiltrates a nerve. (H & E) |
The changes produced by treatment with phosphatidylcholine injections (see above) are similar to factitial panniculitis. In the first few days there is a lobular neutrophilic infiltrate with partially destroyed fat cells. Lymphocytes are present 10 days after treatment and by 2 months there are lipophages and septal fibrosis. 140 Granulomas and pseudomembranous change have also been seen. 141
The histological appearances of the various lipomatosis syndromes are similar, except for the absence of a capsule and increased fibrous tissue in multiple symmetrical lipomatosis, and the ‘infiltrative’ properties of the fat in diffuse lipomatosis. Granulomatous panniculitis has been found in a painful mass in Dercum’s disease, although most reports have shown normal fat. 115
ANGIOLIPOMA
Angiolipomas are subcutaneous tumors of the extremities and trunk; they comprise approximately 10% of tumors of fat.153.154. and 155. They are often multiple, with the first tumors appearing just after puberty.153. and 156. A family history is found in about 10% of cases (OMIM 206550), but no pattern of inheritance has been proposed. A history of previous trauma to the site or the therapeutic use of protease inhibitors is rarely elicited.136. and 157. Numerous angiolipomas appeared in a young adult male with familial angiolipomatosis upon starting anabolic steroids. 158 Mild pain or discomfort is often noted when pressure is applied or the lesions are moved; 159 the pain appears to be related to the vascularity of the lesions.
Subcutaneous angiolipomas have a normal karyotype, setting them apart from most other tumors of fat, including lipomas. 160 For this reason, they have been regarded as a hamartoma of blood vessels and fat, rather than a true tumor of fat. 6
Subcutaneous angiolipomas must be distinguished from the infiltrating angiolipoma, which is a solitary lesion of the deep soft tissues.161. and 162. It will not be discussed further.
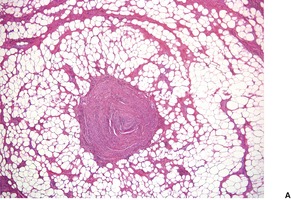
Histopathology153.154. and 163.
Angiolipomas have a thin fibrous capsule with incomplete fibrous septa extending into the lesion, dividing it into lobules of different size. They are composed of variable proportions of fatty tissue and blood vessels (Fig. 35.4). The fat cells are mature, with a single vacuole and an eccentric nucleus. The vascular component, which comprises 5–50% or more of the tumor, consists of groups of capillaries and occasional vessels of larger caliber. 163 Only sparse fat cells were present in the lesion reported as a cellular angiolipoma, 164 which was composed almost entirely of small vessels. In the usual type of angiolipoma there are prominent pericytes around the vessels. 154 Erythrocytes are present within the lumen, and scattered fibrin thrombi are easily found. In one report, hemorrhagic infarction of the fat was present in association with numerous fibrin thrombi and disseminated intravascular coagulation. 165
 |
| Fig. 35.4 Angiolipoma. Mature fat cells are admixed with small blood vessels. (H & E) |
Several cases with a myxoid stroma have been reported (angiomyxolipoma).166.167. and 168. In one case, the cells in the myxoid area expressed CD34. 168 This entity is probably a variant of what has been called dendritic fibromyxolipoma (see p. 851). This tumor shares cytogenetic changes with lipoma, spindle-cell/pleomorphic lipoma and myxoma, setting it apart from the angiolipoma, which has a normal karyotype. 169
There are numerous mast cells throughout the tumor. 170 Bodian stains for small nerves have been consistently negative, but large myelinated nerves have been found in the surrounding connective tissue. 163 About a third of cases express androgen receptors. 158
The finding of a cutaneous melanoma that metastasized to an angiolipoma appears to have been a fortuitous event. 171
Electron microscopy
ADENOLIPOMA
This rare microscopic variant of lipoma, characterized by mature fat admixed with eccrine glands, was first reported in 1993. 172 It is probably an analogue of adenolipomas reported in other organs. 173 The cutaneous variant occurs in the dermis or subcutis with a predilection for the thigh. 173 The lip was involved in one case. 174
On gross examination, they have a soft, yellow, lobulated appearance, often surrounded by a thin capsule. 173
Histopathology
Adenolipoma is characterized by lobules of mature adipose tissue admixed with normal-appearing eccrine glands in varying proportions. Some entrapped eccrine glands show cystic change. A case has been reported in which there was a cystic apocrine component admixed with fat. 173 The authors acknowledged that this tumor, which they called ‘apocrine cystic adenolipoma’ could represent entrapment of epithelial structures within a lipoma. A hyperplastic apocrine gland component was also present in a fatty tumor called ‘cutaneous myxolipoma with glandular differentiation’. 175 Interestingly, a 6p21 chromosomal rearrangement was present. 175
CHONDROID LIPOMA
The chondroid variant of lipogenic tumor was described by Meis and Enzinger in 1993. 176 The lesion is usually deep seated, although subcutaneous variants occur. It has a predilection for females. The lower extremity is the most common location. Its histogenesis is disputed. One view is that the lesion is composed only of white adipocytes, but the other view suggests that the cells have features of embryonal fat and, to a lesser extent, embryonal cartilage. 177 A cytogenetic study has shown a three-way translocation between chromosomes 1, 2, and 5 together with an 11;16 translocation with a breakpoint in 11q13. 178
Chondroid lipomas are firm yellow tumors averaging 3–5 cm in diameter.
Histopathology
The tumors are lobulated, with a thin capsule.176.177. and 179. There are multivacuolated tumor cells within a chondromyxoid matrix. In addition, there are clusters of mature adipocytes with a single vacuole that occupies most of the cytoplasm. The cells contain glycogen and fat. The stroma is strongly metachromatic with toluidine blue at pH 4.0.
Electron microscopy179
The tumor cells have numerous lipid vacuoles of varying size in the cytoplasm. There are glycogen granules, mitochondria, and pinocytotic vesicles. The cells are set in a flocculent stroma, with cartilage demonstrable in some areas. 177
OSSIFYING LIPOMA
Ossification is another change that can be seen in lipomas. Only 25 cases of this rare phenomenon had been reported by late 2007. 180 They arise in the subcutaneous and deeper fat of the trunk, the extremities or the head and neck region. 180 No recurrences have been recorded. Ossification may be secondary to the long duration of the underlying lipoma.
SCLEROTIC (FIBROMA-LIKE) LIPOMA
Sclerotic lipoma, first described by Zelger and colleagues in 1997, is a further rare variant of lipoma. 181 It shows prominent stromal sclerosis. It is more common in males. There is a predilection for the distal extremities, particularly the fingers.181. and 182. The scalp has also been involved. 183 Excision is usually curative. 182
Histopathology
Sclerotic fibromas are circumscribed nodules in the subcutis with a prominent sclerotic stroma, sometimes in a storiform arrangement. The spindled and stellate-shaped cells are cytologically bland with rare, if any, mitoses. 182 There is a resemblance to fibrolipoma or sclerotic fibroma (circumscribed storiform collagenoma), depending on the amount of admixed fat. The number of adipocytes varies from case to case and in different parts of the same tumor. Small foci containing numerous spindle-shaped to stellate cells may be found. The fibrous spindle-cell lipoma has abundant fibrous stroma; sclerosis is not a feature. 184
Immunohistochemistry shows staining for vimentin and also for S100 protein at the margins of the adipocytes. 181 In a large series of 21 cases, the non-lipogenic tumor cells were immunoreactive for CD99 (6 of 6 cases), CD34 (6 of 8 cases), S100 protein (4 of 7 cases), and smooth muscle actin (2 of 6 cases). 182
SPINDLE-CELL LIPOMA
Spindle-cell lipoma is a slow-growing benign tumor of the subcutis. It primarily affects the shoulders, upper back, and back of the neck of men in the fifth to seventh decades.185. and 186. Fewer than 10% of cases occur in women. 187 Uncommonly, the tumors arise on the extremities, 185 lower trunk, 188 oral cavity, 187 and the head.189. and 190. They are generally painless. Multiple lesions are rare; the clinical presentation of such cases may mimic symmetrical lipomatosis (see above). 191 Some cases are familial. 191 Cytogenetic studies generally show monosomy 16 or partial loss of 16q, a finding distinct from liposarcoma. 6 Anomalies of chromosome 13 have also been reported. 192 There is a view that spindle-cell lipoma and pleomorphic lipoma form a spectrum of adipose tumors, which is supported by the finding of similar cytogenetic abnormalities.193. and 194.
Macroscopically, the tumors are soft, oval, lobular masses with an average diameter of 5 cm. They are yellow or gray-yellow in color, and sometimes have a glistening or mucoid appearance on the cut surface.
Histopathology185.188. and 195.
Spindle-cell lipomas are usually circumscribed unencapsulated tumors of the subcutis, although occasionally they are poorly delimited and extend into the dermis or underlying tissues. A variant confined to the dermis (dermal spindle-cell lipoma) has been reported.194.196. and 197. They are composed of a variable mixture of spindle cells and adipose tissue (Fig. 35.5). Sometimes the proliferation of spindle cells is localized. The spindle cells are usually small and elongated and arranged haphazardly. Occasionally they may show a palisaded or fascicular pattern in some areas. A few spindle cells may show small cytoplasmic vacuoles. There is no increase in mitoses, although there may be some nuclear variability. The spindle cells are separated by variable amounts of collagen. Sometimes this stroma shows focal myxomatous change, which stains positively for acid mucopolysaccharides. The tumor reported as dendritic fibromyxolipoma is probably the same adipocytic lesion as reported as vascular myxolipoma (angiomyxolipoma).77. and 166. In many ways, this tumor resembles a spindle-cell lipoma with stromal myxoid areas.
 |
 |
| Fig. 35.5 (A) Spindle-cell lipoma. (B) The tumor is composed of fat cells, fibrous tissue, and scattered spindle-shaped cells. (H & E) |
The intervening fat cells are mature and univacuolated, resembling normal fat. There are no lipoblasts present. In about 10% of consultation cases, fat constitutes less than 5% of the tumor. Such cases can pose diagnostic difficulties because of the dearth of fat. 198 The terms ‘low-fat’ and ‘fat-free’ spindle-cell lipoma have been proposed for these variants. 198 A few tumors have a prominent vascular pattern, 199and this may resemble a lymphangioma or hemangiopericytoma in some areas. 185 The lipomatous hemangiopericytoma is a deep-seated tumor and will not be considered further. 77 At other times there are irregular and branching spaces with villiform connective tissue projections, giving a striking angiomatoid appearance.77. and 200. This is the so-called ‘pseudoangiomatous variant’ (Fig. 35.6). A few inflammatory cells may be found in the walls of these vessels. Mast cells are usually present throughout the stroma. Extramedullary hematopoiesis has been reported in one case. 201 The cytoplasm of the spindle cells stains for vimentin186 and CD34.5.202. and 203. Some factor XIIIa-positive stromal cells are also present. 4 In one series all 22 cases expressed androgen receptors, while in conventional lipomas, 70% were positive, but the staining was often weak. 204
 |
| Fig. 35.6 Spindle-cell lipoma. This is the pseudoangiomatous variant with vascular-like spaces of irregular shape. (H & E) |
In the past, spindle-cell lipoma was sometimes confused histologically with liposarcoma and other spindle-cell sarcomas. The absence of multivacuolated lipoblasts and lack of significant nuclear atypia excludes liposarcoma.
PLEOMORPHIC LIPOMA
Pleomorphic (giant-cell) lipoma is a benign tumor of adipose tissue with atypical histological features that may lead to a misdiagnosis of liposarcoma.205. and 206. It presents as a soft subcutaneous mass, averaging 5 cm in diameter. A case confined to the dermis has been reported. 207 Pleomorphic lipoma has a predilection for the shoulders, back of the neck, back205. and 208. and, less frequently, the face and thighs209 of middle-aged to elderly males. 205 Pleomorphic lipomas resemble spindle-cell lipomas cytogenetically with a consistent loss of chromosome 16q material. 6 For this reason, these two entities are often regarded as forming a spectrum of related adipose tumors. 194 Macroscopically, the tumor resembles a lipoma, although gelatinous gray areas may be present on the cut surface. Some of the reported cases of atypical lipoma are examples of this entity.210. and 211.
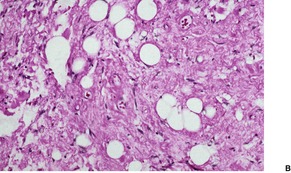
Histopathology205. and 209.
These circumscribed tumors have an intricate mixture of mature adipose tissue, collagen, and myxoid areas interspersed with cellular foci of varying amounts. In addition to lipoblast-like cells, the tumor includes spindle and giant cells, the latter being both uninucleate and multinucleate in type (Fig. 35.7). There are variable numbers of giant cells with marginally placed and often overlapping nuclei, the so-called ‘floret giant cells’. Sometimes the nuclei of some giant cells are smudgy, with indistinct chromatin. Mitoses are rare. Focal collections of lymphocytes and plasma cells are often found within the tumor. A variant with pseudopapillary structures resembling those seen in pseudoangiomatous spindle-cell lipoma (see above) has been described. 212
 |
 |
 |
| Fig. 35.7 (A) Pleomorphic lipoma. (B) Some fat cells have hyperchromatic nuclei with a smudgy appearance. There are no mitoses. (C) Another case showing many hyperchromatic and bizarre nuclei. (H & E) |
At times the pleomorphic lipoma is a circumscribed nodule within an otherwise typical lipoma. Areas resembling spindle-cell lipoma may sometimes be present within pleomorphic lipomas. As in spindle-cell lipoma, there are CD34+ and factor XIIIa+ stromal cells. 4
HIBERNOMA
Hibernoma is a rare benign tumor of the subcutaneous214 and deeper soft tissues, 215 generally considered to arise from brown fat. It is found in the scapular area, axilla, 216 lower neck214 and, less commonly, in the thigh,217. and 218. abdominal wall, 219 and retroperitoneum. 220 It grows slowly. There may be increased warmth over the area. 221 Cytogenetic studies have shown rearrangements in the 11q13 region, frequently including deletions in the region between PLCB3 and PPP1A, leading to loss of the MEN1 gene.178. and 222. In addition, abnormalities involving chromosome 10q22 have been reported. 6
Grossly, hibernomas are tan-brown lobulated tumors, averaging 10 cm in diameter. Several possible malignant variants have been reported, but these have been disputed by others.214. and 223.
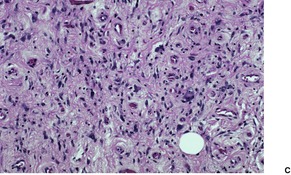
Histopathology214. and 219.
The tumors are thinly encapsulated, and divided into lobules by thin septa. There are usually prominent blood vessels in the septa and lobules; in one case with possible endocrine activity217 they assumed a prominent sinusoidal pattern.
There are three cell types with transitional forms. 220 These include large, coarsely vacuolated cells with multiple vacuoles, univacuolated cells, and smaller cells with granular cytoplasm (Fig. 35.8). Vacuoles stain with oil red O in frozen sections. Lipofuscin pigment is also present. 224 There is often a prominent nucleolus, but there are no mitoses.
 |
 |
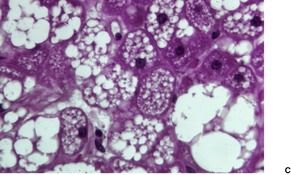 |
| Fig. 35.8 (A) Hibernoma. (B) Some cells are coarsely vacuolated while others have a ‘granular’ cytoplasm. (C) A high power view of the cells. (H & E) |
ATYPICAL SUBCUTANEOUS FATTY TUMORS
This category of fatty tumors is not a distinct entity, but the name given by Allen and colleagues to borderline lesions seen in a consultation practice. 226 The term ‘atypical lipomatous tumor’ is also used. 227 It comprises a histological spectrum ranging from atypical fibrolipomas, through various mixed spindle-cell and pleomorphic lipoma patterns, to tumors indistinguishable from dedifferentiated liposarcomas.226. and 228. Of interest is the extremely good prognosis of atypical lesions confined to the subcutaneous fat, despite sometimes alarming histological features, including the presence of lipoblasts. 226 Local recurrence can occur.
The use of cytogenetics has allowed better, and often specific, characterization of tumors in this group. 229
LIPOSARCOMA
Liposarcoma is the most common soft tissue tumor accounting for 16–18% of all malignant soft tissue sarcomas. 230 Only rarely do they arise in the subcutis or dermis, although they may eventually extend into it from below.231.232. and 233. Accordingly, they will be considered only briefly. They have a predilection for the thighs and buttocks, but may sometimes involve the head and neck234. and 235. or upper extremities. They arise in older adults, and are exceedingly rare in children.63. and 236. Although a few cases have developed in patients with multiple lipomas, liposarcomas are not thought to arise from pre-existing lipomas.231. and 237. They are often large and non-encapsulated, varying in color from yellow to gray, to gray-white. There may be some firmer areas and gelatinous foci in the generally soft tissue.
In 1998, primary liposarcoma of the skin (dermis) was described. 238 Four of the seven cases arose on the scalp. The median age of the patients was 72 years. Local recurrence occurred in two patients, but no metastases or disease-related deaths were recorded. 238 Since that time, a purely intradermal pleomorphic liposarcoma has been reported on the nose of an elderly female, 239 and Fletcher and colleagues have reviewed a series of 57 cases of pleomorphic liposarcoma 16 of which were superficial (dermal or subcutaneous). 240 Only two of these superficial lesions metastasized. 240
Cytogenetic studies have shown clonal karyotypic abnormalities, which often correlate with the histological subtype. 241 For example, the myxoid liposarcoma often demonstrates a reciprocal translocation t(12;16)(q13;p11) that fuses the DDIT3 (CHOP) gene with FUS.241.242.243.244.245.246. and 247. An EWSR1-DDIT3 fusion transcript has rarely been described in myxoid liposarcoma. 247 A similar chromosomal abnormality has been found in the round cell liposarcoma, suggesting that this variant is a poorly differentiated form of myxoid liposarcoma.248. and 249. The well-differentiated liposarcoma (including sclerosing, inflammatory and dedifferentiated variants) is characterized by ring or long marker chromosomes derived from chromosome 12.246. and 250. These long and/or ring chromosome markers are composed of 12q13–q15 amplicons with a constant amplification of the MDM2 gene and frequently CDK4.251.252.253. and 254. Immunohistochemistry can be used to detect these markers, allowing differentiation from lipomas and in the case of the dedifferentiated variants from other pleomorphic sarcomas (see below).229.251. and 255. The pleomorphic liposarcoma has complex karyotypes. 256
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








