Introduction652
INTRODUCTION
Class Crustacea
Lobsters, crabs, shrimps
Class Diplopoda
Millipedes
Class Chilopoda
Centipedes
Class Arachnida
Class Insecta
ARACHNIDS
SCORPION AND SPIDER BITES
Histopathology
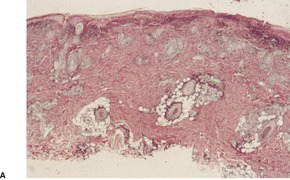
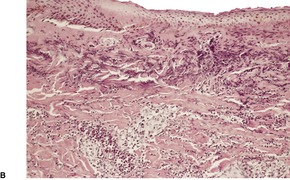
Fig. 30.1
TICK BITES
Histopathology
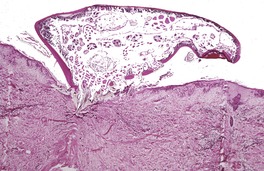
Fig. 30.2
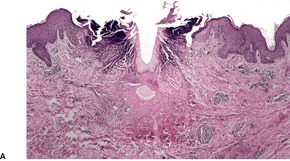
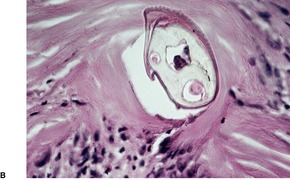
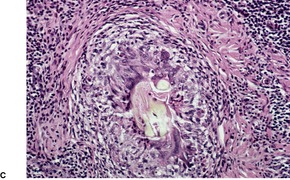
Fig. 30.3
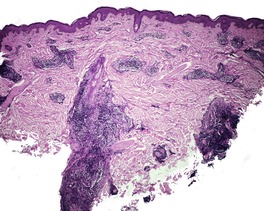
Fig. 30.4
DEMODICOSIS
Histopathology
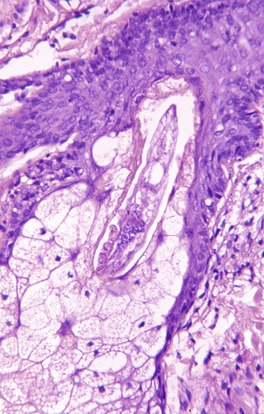
Fig. 30.5
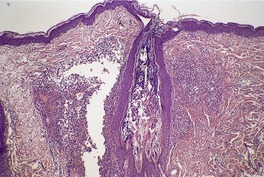
Fig. 30.6
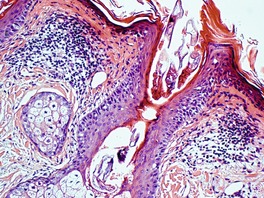
Fig. 30.7
SCABIES

Fig. 30.8
Immunological features
Histopathology
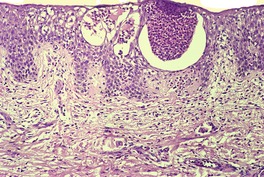
Fig. 30.9
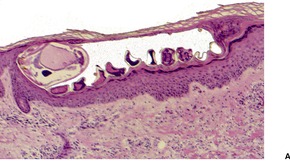
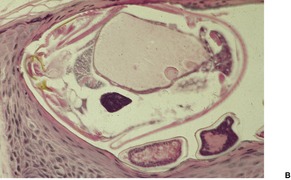
Fig. 30.10
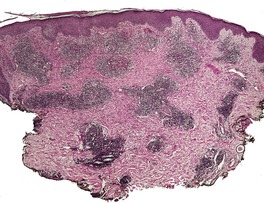
Fig. 30.11
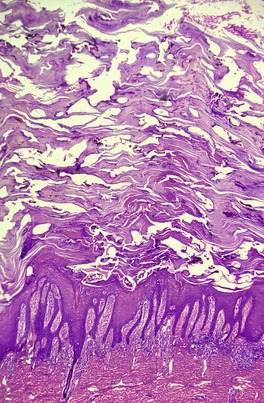
Fig. 30.12
CHEYLETIELLA DERMATITIS
Histopathology
OTHER MITE LESIONS
Histopathology
INSECTS
HUMAN LICE (PEDICULOSIS)
Histopathology
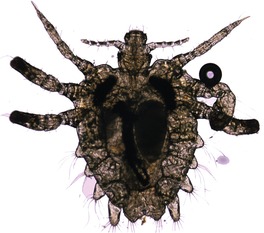
Fig. 30.13

Fig. 30.14
BEDBUGS
Histopathology
MYIASIS
Histopathology
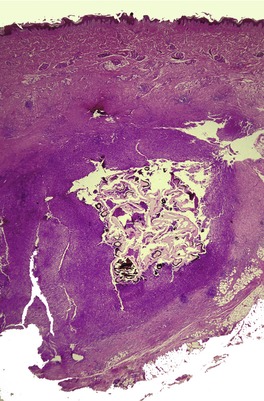
Fig. 30.15
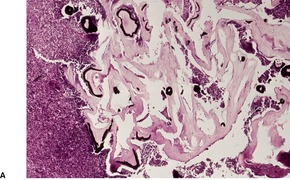
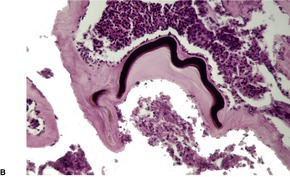
Fig. 30.16
TUNGIASIS
Histopathology
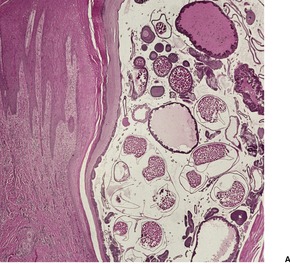
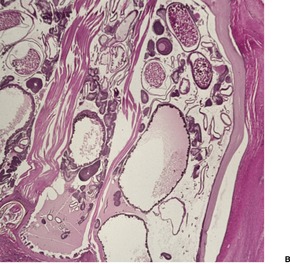
Fig. 30.17
OTHER INSECT BITES
Histopathology
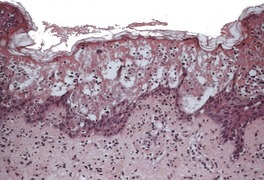
Fig. 30.18
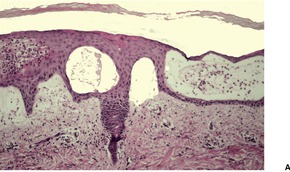
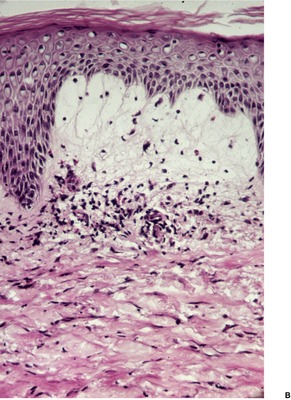
Fig. 30.19
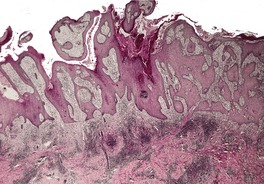
Fig. 30.20
EXAGGERATED BITE REACTIONS
Histopathology351
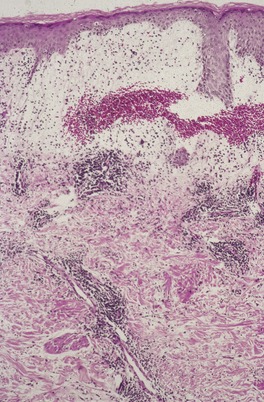
Fig. 30.21
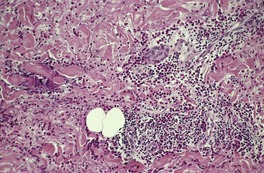
Fig. 30.22
MOSQUITO HYPERSENSITIVITY
Histopathology
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Arthropod-induced diseases
The phylum Arthropoda, which accounts for approximately 75% of animal species, is one of the most important sources of human pathogens.1. and 2. As well as acting as vectors of bacteria, viruses, rickettsiae, chlamydiae, spirochetes, protozoa, and helminths, arthropods may also produce lesions at their portal of entry into the skin. Furthermore, immunological reactions to the parasite or its parts may result in more widely disseminated cutaneous lesions. Specific examples of arthropod-related diseases include mosquito-borne diseases such as malaria, dengue, and viral encephalitides, fly-borne diseases such as leishmaniasis, bartonellosis, and sleeping sickness, and tick-associated diseases such as Rocky Mountain spotted fever, Lyme disease, and tick paralysis. Other examples include mite-borne disease such as scrub typhus, bug-borne disease as seen in Chagas’ disease, and flea-borne disease as occurs in endemic typhus and the plague. 3
There are five major classes of arthropods.4. and 5. The class Insecta is the largest group, although the class Arachnida, which includes ticks, spiders, and mites, is probably of greater dermatopathological interest. The class Crustacea, which includes lobsters, crabs, and shrimps, and the classes Diplopoda and Chilopoda, which include millipedes and centipedes respectively, are not of major dermatopathological importance and will not be considered in detail. They may produce local reactions at the site of contact. These include erythema, urticaria, and purpura in the case of millipedes and centipedes. 6 A brief classification of the arthropods is given in Table 30.1. Mention should also be made of the comprehensive monograph on arthropods and the skin by Alexander7 and the review on venomous arthropods by Vetter and Visscher. 8 Steen et al have reviewed arthropods in dermatology. 9
Scorpions
Spiders
Ticks
Demodex
Sarcoptes
Cheyletiella
Miscellaneous mites
Sucking lice (Anoplura)
Bugs (Hemiptera)
Flies, mosquitoes, sandflies (Diptera)
Fleas (Siphonaptera)
Beetles (Coleoptera)
Moths and butterflies (Lepidoptera)
Bees, wasps, hornets (Hymenoptera)
Finally, mention should be made of Morgellons disease, the name given by Sir Thomas Browne in 1674 to the cutaneous dysesthesia, also termed delusional parasitosis.10. and 11. Patients often present with ‘fibers’ or presumptive parasites removed from the skin seeking laboratory confirmation.12.13.14. and 15. It is a quite common disorder.16. and 17.
Scorpion venom may produce throbbing indurated lesions at the site of attack, usually on acral parts. Erythema, purpura, bullae, necrosis, ulcers, lymphadenitis, and systemic symptoms may develop. 4
Local necrosis may be produced at the site of spider bites; in some cases, e.g. following the bite of a black widow spider (usually Latrodectus mactans), severe systemic symptoms and even death may result. 18 The genus Loxosceles (which includes the brown recluse spider Loxosceles reclusa) may produce a local lesion with quite extensive necrosis, hemorrhage, blistering, and ulceration.19.20.21.22.23.24. and 25. This has been called ‘necrotizing arachnidism’.26. and 27. Not all necrotic lesions on exposed areas are spider bites. 28 A chronic pyoderma gangrenosum-like reaction has also been reported.29. and 30. The diagnosis of loxoscelism can be made by swabbing the lesion and using a specific enzyme-linked immunosorbent assay to detect the venom. 31 A diagnosis of loxoscelism is rarely based on the identification of the spider. 32 Less severe reactions, such as erythema and edema, are more usual with other species of spiders. 33 Sometimes spider leg spines may dislodge in the skin producing a mild erythematous response. 34 An excellent review of spider bites has been published by Wong and colleagues. 35
The efficacy of various treatments for the brown recluse spider venom has been trialed using a rabbit model. No change in eschar size was produced by any of the treatments used. 36 Tetracyclines may be useful in treating cutaneous loxoscelism. 37
The appearances change from a neutrophilic vasculitis with hemorrhage, through a phase with arterial wall necrosis, to eschar-covered ulceration and subcutaneous necrosis. 19 There are usually eosinophils in the accompanying inflammatory infiltrate. The term ‘necrotizing arachnidism’ is given to the necrotic lesions produced by some spider bites (Fig. 30.1).38.39. and 40.
(A) Necrotizing arachnidism. (B) There is epidermal and superficial dermal necrosis. (H & E)
The systemic reaction which uncommonly follows the bite of Loxosceles reclusa, is a necrotizing vasculitis with red cell extravasation but no epidermal necrosis. 41
Ticks are blood-sucking arachnids that attach to many vertebrates. They are important as hosts and transmitters of a wide range of diseases.42. and 43. After the mosquito, they are the second most common vectors of human infectious diseases in the world. 44 Their salivary secretions may produce systemic toxemia and their embedded mouthparts may produce a local erythematous lesion or a more persistent granulomatous or nodular response. 45 Unusual reactions include panniculitis, 46 localized alopecia, 47 papular urticaria, bullae, and hemorrhage. There are two major families of ticks, soft ticks (Argasidae) and hard ticks (Ixodidae). More than 90 species of ticks, both hard- and soft-bodied varieties, have been identified in Australia. 48 Soft ticks (Ornithodoros species) 49 are generally not perceived by the victim, although hard ticks – of which there are several genera, including Ixodes, Amblyomma, and Dermacentor – are eventually noticed because they remain attached for days and slowly engorge with blood. Amblyomma americanus, the lone star tick, is the most common species of this genus found in the United States. 44 Attempts to remove the tick may cause the embedded mouthparts to separate and remain in the tissue. Successful removal of all parts of a tick is vital to minimize significant medical consequences. 48 Multiple pruritic papules due to the partially burrowed larvae of the lone star tick are rarely reported.44. and 50.
In acute lesions there is an intradermal cavity, below which the mouthparts may be seen (Fig. 30.2). There is often a tract of ‘necrosis’ on either side, and in the first few days intense extravasation of fibrin may be seen in relation to vessels. 45 Fibrin thrombi are sometimes present in dermal capillaries. 51 This pattern of hyaline thrombi has been likened to type I (monoclonal) cryoglobulinemia.52. and 53. A moderately dense, predominantly perivascular infiltrate of neutrophils, lymphocytes, plasma cells, and histiocytes is present, with a variable admixture of eosinophils. 54 Neutrophils are sometimes prominent in recent bites. A reaction resembling erythema elevatum diutinum (also interpreted as localized chronic fibrosing vasculitis) followed a tick bite in one individual. 55 The diagnosis may be difficult if tick mouthparts are not seen (Fig. 30.3). A panniculitis, with a preponderance of neutrophils in the infiltrate, may occur. 46
A tick in situ. (H & E)
(A) A tick-bite reaction. (B) Mouthparts are present in the dermis. (C) Another case with a granulomatous reaction to a retained tick. (H & E)
In chronic persistent lesions there is a diffuse superficial and deep infiltrate which includes all the cells found in acute lesions, but usually with many fewer neutrophils and more lymphocytes (Fig. 30.4). Cutaneous lymphoid hyperplasia, either of the T-cell or the B-cell type, may develop. 47 There may be occasional giant cells, dermal fibrosis, and even granuloma formation. 56 The epidermis may show acanthosis or pseudoepitheliomatous hyperplasia.
A persistent tick-bite reaction. The appearances resemble other persistent arthropod bite reactions. (H & E)
Erythema chronicum migrans (Lyme disease), which follows the bite of Ixodes, has been shown to be caused by a spirochete transmitted by the tick. 57 It is considered with other spirochetal diseases in Chapter 24 (p. 579).
Two species of follicle mites are found as normal inhabitants of human skin:58.59.60.61.62.63.64.65.66.67.68. and 69. Demodex folliculorum lives mainly in the hair follicles and Demodex brevis in the sebaceous glands. The larger of the two, Demodex folliculorum, measures about 0.4 mm in length. Mites of this species are often aggregated in a follicle, whereas D. brevis is usually solitary. 60 The mites have been found in 10% of routine skin biopsies (from all sites), and in 12% of all follicles examined in these same biopsies. 61 They are common in basal cell carcinomas removed from the eyelids. 70 They are not increased in pregnancy. 71 The face is most often involved, although D. brevis has a wider distribution. 67 Genital lesions are rare. 72 Although increased numbers of mites are found in sections of rosacea and in subclinical forms of folliculitis, this does not prove a causal relationship.73.74. and 75. It is generally accepted that Demodex mites are not etiologically involved in the usual form of rosacea, although they may possibly play a role in the granulomatous form, in which extrafollicular mites are sometimes seen. Demodex may produce a blepharitis62 and so-called ‘rosacea-like’ demodicosis.66.76.77.78.79. and 80. Scalp demodicosis (demodicidosis) mimicking favus has been reported in a child. 81Demodex has been incriminated as a cause of localized pustular folliculitis of the face,63.78.82. and 83. facial plaques, 84 and of a more widespread eruption in patients with an immunosuppressed state.85.86.87.88. and 89. Refractory Demodex folliculitis may also occur in children with leukemia. 90 However, mite density is not always increased in immunosuppressed patients.80.91. and 92. They are increased in hemodialysis patients but the increase is not statistically significant. 93 Mite density is increased in patients receiving phototherapy. 94 The mites themselves may produce local immunosuppression, allowing them to survive. 95 This theory is based on the finding that Demodex mites appear to increase lymphocyte apoptosis in infested skin. 95 Recently, a rosacea-like demodicosis was reported as a complication of the use of pimecrolimus for the treatment of seborrheic dermatitis. 96 Otophyma is a rare complication of rosaceous lymphedema of the ear associated with Demodex infestation. 97
Facial erythema with follicular plugging (pityriasis folliculorum) is another manifestation of Demodex infestation. 98 The third clinical form of demodicosis in humans, demodicosis gravis, presents a clinical picture similar to severe granulomatous rosacea. 99
The effects of Demodex infestation include follicular dilatation, the presence of dense homogeneous eosinophilic material surrounding the mites, folliculitis, 100 and perifollicular chronic inflammation (Fig. 30.5 and Fig. 30.6). Tiny follicular spicules resulting from the combination of follicular hyperkeratosis and protruding mites have been reported (Fig. 30.7).101. and 102. There are several reports of a granulomatous reaction to extrafollicular Demodex, usually in granulomatous or pustular rosacea.64. and 65. In demodicosis gravis, there are many dermal granulomas containing mite remnants partly phagocytosed by foreign-body giant cells. There may also be central necrosis. 99
A Demodex mite in the lower sebaceous duct. (H & E)
Demodex perifolliculitis. There are numerous mites in the follicle. (H & E)
Pityriasis (demodex) folliculorum. Demodex mites protrude from hair follicles producing small ‘spicules’ on the surface. (H & E)
In rosacea-like demodicosis, up to 10–15 D. folliculorum may be found in individual follicles. 66 Telangiectasia of superficial vessels, perifollicular granulomas, and mild perivascular chronic inflammation may also be seen in this condition.
Scabies is a contagious disease caused by the mite Sarcoptes scabiei var. hominis. It is acquired particularly under conditions of overcrowding and poor personal hygiene, or during sexual contact.103. and 104. Scabies was present in 8.8% of the population in a Brazilian slum. 105 Patients with both minimal disease and only a few mites106 and exaggerated atypical lesions complicating AIDS107.108.109.110.111. and 112. are now being seen, as are patients with inherited disorders of keratinization113. The disease tends to appear in epidemics, which have a cyclical character, recurring at intervals of about 30 years and lasting for about 15 years. 114 The reasons for these cyclic fluctuations are not understood. A new cycle probably commenced in 1993, although there are conflicting reports on the date of commencement of this most recent cycle. 115 Infections are more frequent in the cooler months of the year, possibly related to host overcrowding. 116
Three clinical forms are found: papulovesicular lesions, persistent nodules, and Norwegian (crusted) scabies. The usual lesions are papules and papulovesicles which are intensely pruritic. The vesicles are usually found at the end of very fine wavy dark lines, best seen with the help of a hand lens or by applying a small amount of ink to the surface and removing the excess. 117 These lines represent the excreta-soiled burrows in the horny layer in which the female travels to deposit her eggs. Epiluminescence microscopy enhances the diagnosis of scabies; it gives a low number of false-negative results.118. and 119. Amplification of Sarcoptes DNA in the cutaneous scale, using PCR, has been used to confirm inapparent infection. 120 The application of cyanoacrylate glue (Super Glue) to the skin, followed by a glass slide which is pressed on the suspect skin site, is a recently described method for mite identification. 121
The female mite measures up to 0.4 mm in length and rather less in breadth, whereas the adult male, which dies after copulation, is much smaller (Fig. 30.8). The sites most commonly affected are the interdigital skin folds, the palmar surfaces of the hands and fingers, the wrists, the nipples, the inframammary regions, and the male genitals. The vulva is a rare site. 122 A more generalized eruption is sometimes seen in infants and young children; 123 misdiagnosis is common in this group.124.125. and 126. In addition to the burrows, there is nearly always a secondary rash of small urticarial papules with no mites, which may result from autosensitization.127. and 128. Bullae, resembling bullous pemphigoid, are rarely seen.129.130.131.132. and 133. The presence of circulating antibodies against BP180 and/or BP230 suggests that scabies may induce true bullous pemphigoid. 134
Sarcoptes mite. (×100)
In about 7% of patients, particularly children and young adults, reddish-brown pruritic nodules develop with a predilection for the lower trunk, scrotum, and thighs. 114 These lesions may persist for a year, despite treatment. Mites are rarely found, and this form (persistent nodular scabies) is thought to represent a delayed hypersensitivity reaction similar to that found following some other arthropod bites.
Norwegian (crusted) scabies is a rare contagious form consisting of widespread crusted and secondarily infected hyperkeratotic lesions, found in the mentally and physically debilitated,135.136. and 137. as well as in immunosuppressed patients.112.138.139.140.141.142.143.144.145.146. and 147. This form has also been reported in an otherwise healthy pregnant woman, 148 and in a healthy infant. 149 Norwegian scabies also occurs in patients with epidermolysis bullosa,150. and 151. and in neurological disorders with sensory impairment. 152 There is an extremely heavy infestation with mites. Longitudinal nail splitting has been reported as a consequence of crusted scabies. 153
Human infestation with varieties of Sarcoptes scabiei of animal origin is not uncommon. 154 They produce a self-limiting disease without the presence of burrows.155. and 156. These animal variants are morphologically indistinguishable from the human variant of Sarcoptes scabiei.
The conventional antiscabetics have poor compliance; however, ivermectin, an oral scabicide, is proving a useful substitute.157.158. and 159. Tea tree oil, derived from Melaleuca alternifolia, has recently been found to possess acaricidal activity in vitro. 160
There is some evidence that immunological phenomena are involved in scabies.161.162. and 163. Immediate hypersensitivity may result in the primary lesions, and delayed hypersensitivity in the persistent nodular lesions. Elevated levels of IgE have been found in the serum of some patients with scabies, but the serum IgA is reduced in many with the Norwegian form.164. and 165. IgE has been demonstrated by immunofluorescence in vessel walls in the dermis, 166 IgA and C3 in the stratum corneum, and IgM and/or C3 along the basement membrane in some cases. 167 IgE-containing plasma cells have been found in nodular lesions. 168 In crusted (Norwegian) scabies, there is a predominance of skin-homing cytotoxic (CD8+) T cells and a lack of B cells leading to a defective immune response. This results in uncontrolled growth of the parasite. 169
The histological changes are sufficiently distinctive at least to suggest the diagnosis. 170 There is a superficial and deep infiltrate of lymphocytes, histiocytes, mast cells, 171 and eosinophils, together with some interstitial eosinophils. These features are common to many arthropod reactions. Flame figures and a vasculitis are found, rarely.172. and 173. In addition there are spongiotic foci and spongiotic vesicles within the epidermis, with exocytosis of variable numbers of eosinophils and sometimes neutrophils (Fig. 30.9). Subepidermal bullae, resembling bullous pemphigoid, have been reported.129.130. and 131. Eggs, larvae, mites, and excreta may be seen in the stratum corneum if an obvious burrow is excised (Fig. 30.10).174. and 175. Pink ‘pigtails’, connected to the stratum corneum, and representing egg fragments or casings left behind after the mite hatches, may be present. 176 If the secondary (autosensitization) lesions are biopsied, the picture may not be diagnostic: no mites will be seen, and there is a report which suggests that even eosinophils may be absent. 127 Older lesions may simply show excoriation and overlying scale crusts. 170 Mites may be found in association with cutaneous tumors, either as an incidental phenomenon, or as part of a more widespread infestation. 177
Scabies. There are spongiotic vesicles containing many eosinophils. (H & E)
Scabies. (A) A burrow is present in the stratum corneum. A mite is present at one end with a trail of debris. (B) A higher-power view of the mite. (H & E)
The lesions of persistent nodular scabies resemble those of other persistent bite reactions, with a more dense superficial and deep inflammatory cell infiltrate which includes lymphocytes, macrophages, plasma cells, eosinophils, Langerhans cells, and sometimes atypical mononuclear cells (Fig. 30.11).174. and 178. Lymphoid follicles are sometimes present, and the infiltrate may even extend into the subcutaneous fat. Pseudoepitheliomatous hyperplasia is not a feature. Cases have been published that purportedly resembled cutaneous lymphoma, but the descriptions provided in those instances are not those of lymphoma. 179 Mites are rarely found in routine sections, but if serial sections are studied mite parts can be seen in about 20% of cases. 180 It has been suggested that penetration of mites into the dermis may be responsible for the inflammatory nodules of persistent nodular scabies. 181
Persistent nodular scabies. There is a superficial and deep infiltrate within the dermis. The interstitial eosinophils are not obvious at this magnification. (H & E)
In Norwegian scabies there is a massive orthokeratosis and parakeratosis containing mites in all stages of development (Fig. 30.12). The underlying epidermis shows psoriasiform hyperplasia with focal spongiosis and exocytosis of eosinophils and neutrophils, sometimes producing intraepidermal microabscesses. The dermis contains a superficial and deep infiltrate of chronic inflammatory cells, and usually some interstitial eosinophils.
Norwegian scabies. The thick keratin layer overlying the psoriasiform epidermis contains many mites. (H & E)
Patients with scabies infestation of long duration (>3 months) often have increased numbers of CD30+ cells in the inflammatory infiltrate. 182 The author misdiagnosed lymphomatoid papulosis on a superficial shave biopsy of scabies (some years ago) as a consequence of the large number of CD30+ cells. Hyperplasia of Langerhans cells may also be found. 183
Several species of Cheyletiella, a mite found on dogs, rabbits, and cats, can produce an intensely pruritic dermatitis in humans.184.185. and 186. In animals it produces so-called ‘walking dandruff’. There are erythematous papules and papulovesicles, sometimes grouped, with a predilection for the chest, abdomen, and proximal extremities. 187 Involved areas usually correspond to the sites of close physical contact with the infested pet. 188 The mite is almost never found on humans, and the diagnosis may be confirmed by examining fur brushings of the patient’s pet for the mite.189. and 190. This condition is no longer thought to be synonymous with so-called ‘itchy red bump’ disease (papular dermatitis), a papular pruritic disorder of uncertain histogenesis which was originally reported from Florida, USA (see p. 113).184. and 191. Delayed hypersensitivity mechanisms are thought to play a role in the pathogenesis of the eruption. 192
Sections show focal epidermal spongiosis at the site of the bite. There is a superficial and mid-dermal predominantly perivascular infiltrate composed of lymphocytes, macrophages, and some eosinophils. There are usually some interstitial eosinophils, suggesting an arthropod bite; however, the reaction is more superficial and less inflammatory than the usual arthropod reaction. Vesiculobullous lesions appear to result from both intraepidermal and subepidermal vesiculation although the histology of this rare form often goes unreported. 193
Five other families of mites have been incriminated in the production of cutaneous lesions: Tyroglyphoidea (food mites), Pyemotidae (predacious or grain itch mites), Dermanyssidae (parasitoid or rat mites), Trombiculidae (trombiculid or harvest mites, chiggers), and Tydeidae (sawdust mite).4.5.185. and 194.
Food mites and predacious mites produce erythematous papules, papulovesicles, or urticaria in workers handling certain foods and grain. The lesions may be mistaken for scabies, but there are no burrows. 45 The genera involved include Glycophagus (grocery mite), Acarus (cheese mite), Tyrophagus (copra mite), Pyemotes (grain itch mite), and Tyroglyphus.45.155. and 195. The house dust mite Dermatophagoides pteronyssinus and related species are widely distributed in bedding and clothing, and may play a role in producing or exacerbating chronic dermatitis.196. and 197.
The parasitoid mites may produce papular urticaria in people employed in grain stores or living in places harboring rats.198. and 199. Pet rabbits may be infected by the mite Listrophorus gibbus, which can produce a papular urticaria in the handler. 200 Various birds, including pet gerbils, may harbor mites from the family Dermanyssidae.201.202.203. and 204. The term ‘gamasoidosis’ has been used to describe the human skin disease caused by mites from birds and other animals. 201
The trombiculid mites may produce a severe dermatitis with minute, intensely pruritic red elevations. 205 They have a predilection for the lower legs, groin, and waistline.
The lesions produced by mites other than chiggers resemble those generally seen in mild arthropod reactions, with a superficial and mid-dermal perivascular infiltrate, some interstitial eosinophils and mild epidermal spongiosis. The mite is almost never found. Some neutrophils are usually present in lesions produced by Pyemotes species. 45
Bites by chiggers (Trombicula species) may be centered on hair follicles or in skin having a thin horny layer. A tissue canal or ‘stylostome’ surrounded by a mass of hyaline tissue runs into the malpighian layer. There is usually epidermal spongiosis, dermal edema with some neutrophils, and later a more mixed dermal inflammatory infiltrate, as in other arthropod lesions. A chronic granulomatous response has been described. 45
Pediculosis, which has been known for over 10 000 years, is caused by three types of lice, each having a separate microenvironment. 206 The head louse (Pediculus humanus capitis) infests the hairs of the scalp. It is an increasing problem in many urban communities, 105 with outbreaks particularly in schools,207.208.209.210.211. and 212. although the incidence is declining in some communities. 213 Recent work suggests that fomite transmission is an important source of infestation.214.215. and 216. In some parts of the world, including the United States, Canada, and Australia, public health authorities have adopted a ‘no nit’ policy which results in the immediate dismissal from school of any child found to have lice or eggs (nits) in their hair. As not all nits are viable, and not all children with them have concurrent lice, it has been suggested that the ‘no nit’ policy be replaced with other programs. 217 As the nit sheath is similar in composition to hair, eradication programs will need to take note of this fact. 218 Bug buster kits (fine-toothed combs) are favored in some regions over the use of pediculicides, such as malathion and permethrin.219.220.221.222. and 223. In a comparative trial malathion was found to be superior to permethrin for the treatment of head lice. 224 There is an emerging resistance to pediculicides in some parts of the world. 225 New pediculicides are being trialed. 226
The pubic louse (Phthirus pubis) infests pubic and axillary hair in particular, although there may be colonization of any heavy growth of hair on the trunk and limbs. 227 Occasionally the eyebrows are infested, and very rarely the scalp.228.229.230. and 231. It is more common in the cooler months. 232 The HIV status of the patient does not appear to influence the severity of the infestation. Both the pubic louse and the head louse cement their eggs to hair, forming the minute gritty projection that is known as a nit. Multiple bluish spots (maculae ceruleae) may be found, particularly on the trunk, in persons infested with the pubic louse. 233
The body louse (Pediculus humanus corporis) divides its existence between the host and the host’s clothing, in the seams of which it deposits its eggs.
The lice are blood-suckers but the amount consumed is minimal. 234 The injected saliva may produce an allergic reaction. This hypersensitivity rash, or pediculid, may mimic a viral exanthem. 206 The resulting itching may lead to excoriation or secondary bacterial infection.
A louse may be removed from the body and examined microscopically for confirmation (Fig. 30.13). Nits may also be identified by examining involved hairs (Fig. 30.14).
Crab louse (Phthirus pubis). (×27)
Pediculosis. Hair shaft with an attached egg (nit) of the head louse. (×40)
Bedbugs (Cimicidae) are found usually in dirty and dilapidated housing, associated with unwashed bedlinen. 236 They may also infest wooden seating in public transport. They are notoriously difficult to eliminate. 237
The common bedbug (Cimex lectularius) can produce pruritic, urticarial, vesicular, and even bullous lesions.238. and 239. Anaphylactic reactions and persistent nodular lesions are rare. 240 The distribution of the lesions is influenced by the method of infestation and the wearing of bedclothes. 237 At least six other species may rarely parasitize humans. 241
Urticarial lesions show variable edema of the upper dermis with perivascular lymphocytes, eosinophils, and mast cells. A few interstitial eosinophils are also present. Vesiculobullous lesions show both intraepidermal and subepidermal edema. Hemorrhage may be present in the dermis in bullous lesions. 237
Myiasis is the infestation of live human tissues by the larvae of flies in the order Diptera.242.243.244. and 245. It is said to be the fourth most common travel-associated skin disease.246. and 247. In Central and South America dermal myiasis is usually caused by the ‘human botfly’, Dermatobia hominis.248.249.250.251.252.253.254. and 255. In West and Central Africa the tumbu fly (Cordylobia anthropophaga) is involved.256.257.258.259.260.261. and 262. In one study of a rural community in the Niger Delta, 36% of 150 women, and 20% of 75 infants studied were infected by C. anthropophaga. 263 Other flies, some of them of restricted geographical distribution, can produce myiasis, including species of Parasarcophaga, 264Psychoda, 265Gasterophilus, Hypoderma,266. and 267. Cuterebra,268.269.270.271. and 272. Cochliomyia,273.274. and 275. Chrysomya, 276 and Wohlfahrtia.4. and 277. The larvae of the common housefly Musca domestica may rarely infest the skin of debilitated and extremely neglected patients.278. and 279. The eggs may be transmitted to humans by another insect, such as the mosquito in the case of Dermatobia hominis, or the larvae may burrow into the skin of a suitable host after hatching on the ground or on clothing, as with the tumbu fly. 280 In contrast to botfly larvae that are larger and have abdominal hooklets anchoring them under the skin, the tumbu larvae do not have anchoring hooklets and they can be extruded by squeezing the skin. 280
The larva completes its molts in from about 2 weeks to 3 months or longer, depending on the species. It then works its way out of the skin and falls to the ground, where pupation occurs. This may be noted by the patient.
The lesions have a predilection for exposed surfaces such as the feet and forearms. 281 The scalp is uncommonly involved, while penile involvement is very rare.261.282. and 283. Lesions have a furuncle-like presentation which culminates in ulceration.246.284. and 285. Sometimes there are plaques with draining sinuses. 286 Tissue destruction may result when sites such as the nose are involved. 275 Large inflammatory nodules have been reported in a person with HIV infection. 287 There may be throbbing pain as the lesion enlarges. Ultrasound and dermoscopy can be used to confirm the clinical diagnosis.288. and 289.
Myiasis has been proposed as a risk factor for prion diseases in humans. 290 Prion rods have been identified in both fly larvae and pupae. 290
Treatment may involve three processes: occlusion to deprive the larva of oxygen, removal of the larva by squeezing or a surgical technique, and the use of larvicides such as ivermectin. 245
There is usually a small cavity, in the dermis and sometimes in the subcutaneous tissue, containing the developing larva (Fig. 30.15). Surrounding this is a heavy mixed inflammatory cell infiltrate which includes lymphocytes, histiocytes, occasional foreign-body giant cells and plasma cells, as well as eosinophils; neutrophils are also present near the cavity. 242 There are abundant activated fibroblasts elaborating collagen, which may relate to larval containment. 242 A sinus tract may lead to the surface, with ulceration. Fragments of larva are usually seen within the cavity (Fig. 30.16). It is encased by a thick chitinous cuticle with widely spaced spines on the surface. These spines act as anchoring points to fasten the larva to the skin. 291 This material is polarizable. 292 Beneath the cuticle, layers of striated muscle and internal organs may be seen. 293
Myiasis. Larval parts are present within a subcutaneous cavity, the wall of which contains a heavy inflammatory cell infiltrate. (H & E)
(A) Myiasis. (B) Higher magnification of the case in Fig. 30.15 showing fragments of the larval wall. (H & E)
Immunohistochemical studies have shown that 30% of the cells in the inflammatory infiltrate are cytotoxic CD4-positive T cells that produce a Th2 cytokine pattern. 294
Tungiasis is produced by infestation of the skin by the pregnant female sandflea Tunga penetrans. 295 It occurs in Central and South America, tropical Africa, and Pakistan.296.297.298.299. and 300. In one community in Nigeria, 45% of the population were found to be infested with this parasite, and the median parasite load was six. 301 Close to one hundred parasites have been detected in a patient with Klippel–Trenaunay syndrome. 302 International travel has resulted in its occurrence in many countries.303.304.305.306.307.308. and 309. As the flea is a poor jumper, lesions are usually found on the feet. 301 Penetration into the dermis by the flea produces characteristic single or multiple white papules, and eventually nodules about 1 cm in diameter. 310 Lesions have a central black dot and erythematous margins. The black region corresponds to the posterior portion of the flea. 311 Dermoscopy can be used to confirm the diagnosis.312.313. and 314. On entering the skin the female tunga is about 0.1 cm in diameter, but this increases to 0.6 cm or more as the 150–200 eggs within the abdomen of the gravid female mature. Once the ova have been shed through an opening in the skin and the tunga has died, the nodule usually becomes frankly ulcerated.
A second species of Tunga, T. trimamillata, has been reported in humans from Ecuador. 311 Its preferential hosts are goats, pigs, and cattle.
Surgical removal of the sandflea is the treatment of choice. Topical ivermectin, thiabendazole, and metrifonate have been used. Oral ivermectin is also effective. 315
The diagnosis is made by finding the tunga in the epidermis or dermis, with its characteristic exoskeleton and internal parts, including ova (Fig. 30.17).310. and 316. There is a surrounding mixed inflammatory cell infiltrate of lymphocytes, plasma cells, and eosinophils. A mass of eggs may be seen within the stratum corneum, with underlying epidermal necrosis; in later lesions there is ulceration. 310
Tungiasis. (A) The parasite has penetrated the epidermis and occupies much of the dermis. (B) A further case of the disease. (H & E)
Species within the order Diptera may be responsible for cutaneous lesions other than myiasis. These insects include mosquitoes, gnats, and midges. Mosquitoes may cause urticarial and even bullous lesions in occasional sensitized hosts. They may also cause a life-threatening disorder in patients with Epstein–Barr virus infection (see below).317. and 318. The biting gnats and midges may give urticarial wheals or pruritic papules. 319 Papular urticaria is a common reaction to fleas. Large persistent lesions may develop in patients infected with HIV. 320 A related phenomenon is the development of exuberant lesions in patients with hematological disorders, particularly chronic lymphocytic leukemia (see below).
Beetles (order Coleoptera) can produce slowly forming blisters, necrotizing lesions, or papular urticaria.321.322. and 323. The best known blister beetle is Lytta vesicatoria (the Spanish fly), an insect endemic to southern Europe. 324 The blisters are produced by cantharidin, a substance found in certain beetles. 325 Other families of beetle have a different vesicating toxin in their coelomic fluid, known as pederin, which is released when the beetle is accidentally crushed on the skin. 326 Recently, an outbreak of over 250 cases of a vesicular dermatitis was reported from Australia. 324 It was caused by the genus Paederus (rove beetles). 324 Other outbreaks have been reported from Sri Lanka, 327 South India, 328 and Iran. 329
Some species of moths and butterflies (order Lepidoptera) have larvae (caterpillars) with surface hairs (setae) that may produce urtication on entering the skin. The setae, which contain an urticating toxin (thaumetopoein), may be airborne, producing disease in unsuspecting hosts.330. and 331. Erythematous macules and papules and urticarial wheals may be seen.332.333. and 334. Incidentally, there are more than 165 000 species in the order Lepidoptera, but only 150 are medically important. 335
Moths of the genus Hylesia (found particularly in South America) may produce an intensely pruritic urticarial rash within a few minutes to several hours after contact with the abdominal hairs of the adult female moth. 336
Small erythematous papules may result from the bite of the thrip, a tiny insect in the order Thysanoptera. 337 They are often misdiagnosed as mosquito bites. They may also produce itching without visible lesions. 338 Psocids, very small insects of the order Psocoptera, very rarely cause infestations of humans. 339 One such genus, Liposcelis, is found in old, moldy books and called ‘booklice’. They may cause mild pruritus. 339 One case of infestation associated with onychomycosis has been reported. 340
Severe urticarial edema and even anaphylaxis may follow the stings of species within the order Hymenoptera (bees, wasps, ants, and hornets) in some susceptible individuals.3.341.342. and 343.
There was a recent review on the cutaneous side effects of insect repellents. 344 Despite the widespread use of repellents, complications, such as an irritant contact dermatitis, are quite uncommon. 344
The appearances will depend on many factors, such as the nature of the arthropod, the duration of the lesion, the immunological reaction (immediate or delayed hypersensitivity), the presence of arthropod parts, and the discharge of toxins.
Lesions of papular urticaria show prominent papillary dermal edema and a superficial and deep inflammatory infiltrate, with perivascular accentuation and usually some interstitial eosinophils. Papular and papulovesicular lesions resemble those produced by other arthropods.
Some neutrophils are often present in lesions biopsied in the first day or so, particularly with certain insects. Flea bites usually have some neutrophils in the exudate, as do the necrotizing lesions produced by beetles.
Plasma cells may be prominent, particularly in the deep dermis, in some persistent insect bites; rarely the appearances may simulate a plasmacytoma.
Focal epidermal necrosis is seen with some gnat and beetle bites.319.323. and 345. The vesicular dermatitis associated with the whiplash rove beetle (Paederus), see page 96, is characterized by intraepidermal and suprabasal vesicles and pustules with reticular and confluent necrosis of the epidermis and the superficial zones of the appendages (Fig. 30.18). 324 There are occasional eosinophils in the dermal infiltrate.
Paederus bite reaction. A neutrophilic spongiosis with focal necrosis is present. (H & E) (Photograph kindly provided by Dr Dominic Wood)
Bullous lesions seen in some hosts susceptible to mosquitoes have large intraepidermal vesicles with thin strands of epidermis between the vesicles and prominent edema of the papillary dermis (Fig. 30.19). 346 Intraepidermal vesicles containing eosinophils may be seen in caterpillar dermatitis and in some other bite reactions, particularly at the point of entry of any mouthparts. Moths of the genus Hylesia produce a spongiotic epidermal reaction related to a fine hair shaft implanted by the moth; there is some exocytosis of neutrophils and lymphocytes.
Arthropod bite reaction. (A) Mixed epidermal and subepidermal edema are present. (B) A further case with only subepidermal edema. (H & E)
Other findings that may be seen in persistent insect bite reactions include pseudoepitheliomatous hyperplasia, sometimes quite severe (Fig. 30.20), and atypical dermal infiltrates which may be mistaken for malignant lymphoma.347. and 348. CD30-positive cells may be present, as also occurs in scabies. 349 Langerhans cells, particularly in a perivascular location, are sometime abundant in bite reactions. The dendritic staining pattern of these cells with CD1a helps to differentiate them from Langerhans cell histiocytosis. 350 The presence of a heterogeneous cell population with interstitial eosinophils is a reassuring sign in these rare atypical lesions.
Arthropod bite reaction. There is pronounced pseudoepitheliomatous hyperplasia, an uncommon pattern of reaction. (H & E)
It should be noted that the cnidarians (coelenterates) can produce lesions which mimic both clinically and histologically those produced by arthropods (see p. 642), including the development of persistent nodular lesions.
Exuberant papular and vesiculobullous lesions may develop in patients with leukemia, particularly chronic lymphocytic leukemia, apparently as an exaggerated response to arthropod bites.351.352. and 353. A similar reaction has been reported in association with mantle cell lymphoma.354. and 355. Patients usually do not recall being bitten. The reaction may precede the diagnosis of the hematological disorder. Lesions may persist for many years. 352 Immunodeficiency may play a role in their pathogenesis, as similar lesions have been reported in HIV infection (see above). It has been suggested that the term eosinophilic dermatosis of myeloproliferative disease is more appropriate.356. and 357.
Dapsone has been used successfully in the management. 358
The epidermal changes include eosinophilic spongiosis, vesiculation, and full-thickness necrosis. Both intraepidermal and subepidermal vesicles may be present (Fig. 30.21). There is a superficial and deep perivascular and interstitial infiltrate of lymphocytes and eosinophils of variable density. Flame figures and lymphoid nodules are sometimes seen (Fig. 30.22). A vasculitis, usually of lymphocytic type, may be present.
Exaggerated bite reaction in a patient with chronic lymphocytic leukemia. (H & E)
Exaggerated bite reaction. There are numerous eosinophils and flame figures. (H & E)
The triad of hypersensitivity to mosquito bites, chronic Epstein–Barr virus infection, and natural killer cell leukemia/lymphoma has been reported in recent years, mainly in Japanese children.317.359.360. and 361. Some patients may not express the triad; patients with natural killer cell lymphocytosis have been reported with mosquito hypersensitivity. 318 Death from the hemophagocytic syndrome may occur. 317 Hypersensitivity to mosquito bites, presenting as a hydroa vacciniforme-like eruption in patients with lymphoma, is a closely related phenomenon. 362 Such patients may not have chronic Epstein–Barr virus infection (EBV). 362
The epidermis is usually necrotic. There is underlying dermal edema, particularly in the superficial dermis. There is a leukocytoclastic vasculitis. In addition to the infiltration of neutrophils there are also many lymphocytes. They are large, having irregularly shaped nuclei, and express CD56. 317 In-situ hybridization with the EBER1 probe shows that approximately 5% of infiltrating cells in the skin lesions are positive for EBV. 361
References
Introduction
1. Zhu, YI; Stiller, MJ, Arthropods and skin diseases, Int J Dermatol 41 (2002) 533–549.
2. Jacobson, CC; Abel, EA, Parasitic infestations, J Am Acad Dermatol 56 (2007) 1026–1043.






