Transverse Rectus Abdominis Myocutaneous Flap Reconstruction: the Single-Pedicle, Whole-Muscle Technique
Michael R. Zenn
James W. May Jr.
The transverse rectus abdominis myocutaneous (TRAM) flap has proven itself over the years as the autogenous tissue of choice for breast reconstruction (1). Differences of opinion continue to exist, however, as to the safest and most reliable method of transferring this tissue to the reconstructive site. Similarly, many methods of abdominal wall closure exist. Common goals for any breast reconstructive procedure are (a) safe and well-perfused volume of tissue transferred and (b) minimization of donor-site morbidity. The technique presented has evolved to allow predictability in survival of tissue transferred with minimal donor-site morbidity while affording the opportunity for dramatic abdominal aesthetic improvement.
Several strategies and biases have emerged to meet these goals. When a pedicle procedure is desired, we usually use a single-pedicle, whole-muscle technique while avoiding the use of bipedicle techniques when possible. Rather than attempt to create a very large matching breast, reduction of the opposite breast is encouraged. Most important, we treat the abdomen as if it were the primary reason for the procedure, and, to that end, synthetic mesh is used in most cases (2). Although free TRAM and deep inferior epigastric perforator flaps are often used, patients with adequate tissues in the best-perfused part of the TRAM flap (i.e., zone 1) may be best served with our technique. The whole-muscle technique is fast, reliable, requires no microsurgery, and eliminates patient anxiety about total flap loss. In cases in which the entire abdomen is required or the patient has been irradiated, free flap techniques are preferred. Bipedicle techniques should be reconsidered, given the lesser morbidity of perforator and free flap techniques and the morbidity of loss of both rectus abdominis muscles.
Flap Elevation
In the uncomplicated case, our preference is to leave the donor scar as low as possible on the abdomen. Accordingly, we harvest our flap inferiorly to within 2 cm of the pubis, laterally to the anterior axillary line, and superiorly to include the umbilicus and its perforators (Fig. 52.1). For high-risk patients or large tissue requirements, the design may be moved cephalad, a delay procedure can be considered, or the flap can be elevated as a free tissue transfer (3). It is important when incising the flap to bevel the incisions to include a maximum number of periumbilical perforators and as much subcutaneous tissue as possible. Flaps are elevated above the fascia to the first perforator visualized at the lateral border of the rectus sheath on the pedicle side. The opposite side is elevated to the linea alba. The abdominal wall superiorly is elevated above the fascia to the level of the costal margin. A medial tunnel is created to connect this dissection to the mastectomy defect while avoiding the detachment of the inframammary fold.
For most patients, we prefer to use the contralateral muscle for best breast fullness and ptosis. If one needs more lateral fullness or wants to avoid an epigastric bulge, an ipsilateral muscle pedicle may be used. The decision to use the whole rectus muscle is based on vascular studies by Moon and Taylor, which showed that blood supply through the rectus may exist in multiple branches throughout the width of the rectus muscle (4). Muscle splitting may therefore be hazardous because ultimate perfusion of the TRAM flap may be diminished (5). Although muscle splitting may provide more fascia for primary closure, the remaining muscle, both medially and laterally, likely plays little if any role in abdominal wall function, as it is deinnervated and atrophied (6,7,8,9). Attempting to preserve the entire fascia while harvesting the whole muscle may also be dangerous due to the superficial nature of the blood supply at the muscular inscriptions (4). The use of synthetic mesh for abdominal wall closure allows most of the anterior fascia overlying the rectus muscle to be harvested, ensuring maximal vascularity while speeding flap elevation.
With the use of a small incision in the rectus fascia, the lateral border of the rectus muscle may be identified. In harvesting the whole rectus muscle, it is important to leave 1 to 2 cm of the lateral anterior rectus fascia in the donor site. This will preserve the linea semilunaris ligament and allow a site to secure the mesh during abdominal closure. Preservation of the linea semilunaris is important in maintaining the complex intermuscular relationships that exist in the anterior abdominal wall. The incision is continued to approximately 3 cm below the arcuate line. At this level, the inferior epigastric pedicle can be visualized and spared, while the anterior fascia and rectus abdominis are transversely divided. This is most easily done by placing the dissecting finger between the vascular pedicle and the muscle. The fascia is sharply incised the full width of the muscle to the midline. This allows the muscle to be divided in such a way that more muscle is taken with the flap than fascia. At this point, for surgeons with microsurgery experience, a few minutes are invested to dissect the deep inferior epigastric pedicle and ligate it near its origin, should it be needed later for arterial or venous supercharging. Before medial incision of the rectus sheath, the umbilicus is circumscribed and isolated with a cuff of subcutaneous fat to ensure its viability, especially on the side where no muscle is harvested and perforators will remain. Once that is done, the medial anterior rectus sheath can be safely incised.
The dissection superiorly is continued above the costal margin. Due to the variability of the location of the superior
epigastric pedicle, it is visualized directly and protected during the cephalad 5 cm of elevation. The highest intercostal nerve is identified and divided to ensure rectus muscle atrophy, thus limiting fullness in the epigastric area where the pedicle crosses the chest. The highest intercostal nerve is often found under the costal margin and may require extra dissection there to identify and divide it.
epigastric pedicle, it is visualized directly and protected during the cephalad 5 cm of elevation. The highest intercostal nerve is identified and divided to ensure rectus muscle atrophy, thus limiting fullness in the epigastric area where the pedicle crosses the chest. The highest intercostal nerve is often found under the costal margin and may require extra dissection there to identify and divide it.
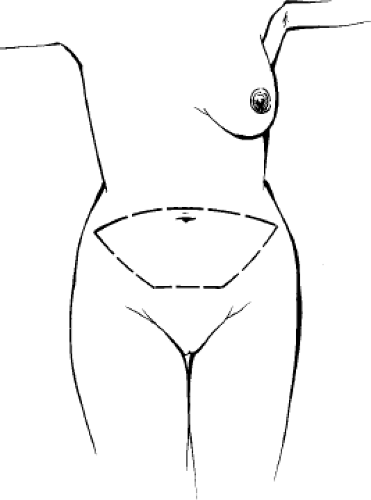 Figure 52.1. Transverse rectus abdominis myocutaneous flap incision ideally placed inferiorly. Modifications are patient dependent.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





