Key Words
topical therapy, corticosteroids, xerosis, steroid, topical application, adverse reaction, wet diseases, reaction management, topical steroids
Topical Therapy
A wide variety of topical medications are available for treating cutaneous disease (see Formulary). Specific medications are covered in detail in the appropriate chapters, and the basic principles of topical treatment are discussed here.
The skin is an important barrier that must be maintained to function properly. Any insult that removes water, lipids, or protein from the epidermis alters the integrity of this barrier and compromises its function. Restoration of the normal epidermal barrier is accomplished with the use of mild soaps and emollient creams and lotions. There is an old and often-repeated rule: “If it is dry, wet it; if it is wet, dry it.”
Dry Diseases.
Dry skin or dry cutaneous lesions have lost water and, in many instances, the epidermal lipids and proteins that help contain epidermal moisture. These substances are replaced with emollient creams and lotions.
Wet Diseases.
Exudative inflammatory diseases leak serum that leaches the complex lipids and proteins from the epidermis. A wet lesion is managed with wet compresses that suppress inflammation and debride crust and serum. Repeated cycles of wetting and drying eventually make the lesion dry. Excessive use of wet dressings causes severe drying and chapping. Once the wet phase of the disease has been controlled, the lipids and proteins must be restored with the use of emollient creams and lotions, and wet compressing should stop.
Emollient Creams and Lotions
Emollient creams and lotions restore water and lipids to the epidermis (see Formulary). Preparations that contain urea (e.g., Carmol 10, 20, 40; Vanamide) or lactic acid (e.g., Lac-Hydrin, AmLactin) have special lubricating properties and may be the most effective. Creams are thicker and more lubricating than lotions; petroleum jelly and mineral oil contain no water.
Lubricating creams and lotions are most effective if applied to moist skin. After bathing is an ideal time to apply moisturizers. Wet the skin and pat it dry, then immediately apply the moisturizer. Emollients should be applied as frequently as necessary to keep the skin soft. Chemicals such as menthol and phenol (e.g., Sarna lotion) are added to lubricating lotions to control pruritus (see Formulary).
Severe Dry Skin (Xerosis)
Dry skin is more severe in the winter months when the humidity is low. “Winter itch” most commonly affects the hands and lower legs. Initially the skin is rough and covered with fine white scales; later, thicker tan or brown scales may appear. The most severely affected skin may be crisscrossed with shallow red fissures. Dry skin may itch or burn. Numerous creams and lotions are available to treat dry skin. They are all effective.
Wet Dressings
Wet dressings, also called compresses, are a valuable aid in the treatment of exudative (wet) skin diseases ( Box 2.1 ). Their importance in topical therapy cannot be overstated.
Acute eczematous inflammation (poison ivy)
Bullous impetigo
Eczematous inflammation with secondary infection (pustules)
Herpes simplex and herpes zoster (vesicular lesions)
Infected exudative lesions of any type
Insect bites
Intertrigo (groin or under breasts)
Nummular eczema (exudative lesions)
Stasis dermatitis (exudative lesions)
Stasis ulcers
Sunburn (blistering stage)
Tinea pedis (vesicular stage or macerated web infections)
The technique for wet compress preparation and application is described in the following list.
- 1.
Obtain a clean, soft cloth such as bedsheeting or shirt material. The cloth need not be new or sterilized. Compress material must be washed at least once daily if it is to be used repeatedly.
- 2.
Fold the cloth so there are at least four to eight layers and cut it to fit an area slightly larger than the area to be treated ( Fig. 2.1 ).
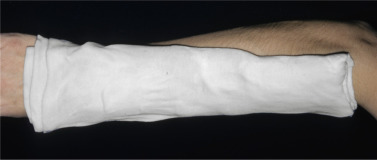
FIG 2.1
Cool wet compresses control acute inflammation.
- 3.
Wet the folded dressings by immersing them in the solution, and wring them out until they are sopping wet (neither running nor just damp).
- 4.
Place the wet compresses on the affected area. Do not pour solution on a wet dressing to keep it wet because this practice increases the concentration of the solution and may cause irritation. Remove the compress and replace it with a new one.
- 5.
Dressings are left in place for 30 minutes to 1 hour. Dressings may be used two to four times a day or continuously. Discontinue the use of wet compresses when the skin becomes dry. Excessive drying causes cracking and fissures.
- •
Antibacterial action: Aluminum acetate, acetic acid, or silver nitrate may be added to the water to provide an antibacterial effect ( Table 2.1 ).
- •
Wound debridement: A wet compress macerates vesicles and crust, helping to debride these materials when the compress is removed.
- •
Inflammation suppression: Compresses have a strong antiinflammatory effect. The evaporative cooling causes constriction of superficial cutaneous vessels, thereby decreasing erythema and the production of serum. Wet compresses control acute inflammatory processes, such as acute poison ivy, faster than either topically applied or orally administered corticosteroids.
- •
Drying: Wet dressings cause the skin to become dry. Wetting something to make it dry seems paradoxical, but the effects of repeated cycles of wetting and drying are observed in lip chapping, caused by lip licking; irritant hand dermatitis, caused by repeated washing; and soggy sock syndrome in children, caused by perspiration.
Topical Corticosteroids
Topical corticosteroids are a powerful tool for treating skin disease. Understanding the correct use of these agents will result in the successful management of a variety of skin problems. Many products are available, but all have basically the same antiinflammatory properties, differing only in strength, base, and price.
Strength
Potency (Groups I Through VII).
The antiinflammatory properties of topical corticosteroids result in part from their ability to induce vasoconstriction of the small blood vessels in the upper dermis. This property is used in an assay procedure to determine the strength of each new product. These products are subsequently tabulated in seven groups, with group I the strongest and group VII the weakest (see the Formulary and the inside front matter of this book). The treatment sections of this book recommend topical steroids by group number rather than by generic or brand name because the agents in each group are essentially equivalent in strength.
Lower concentrations of some brands may have the same effect in vasoconstrictor assays as much higher concentrations of the same product. One study showed that there was no difference in vasoconstriction between Kenalog 0.025%, 0.1%, and 0.5% creams.
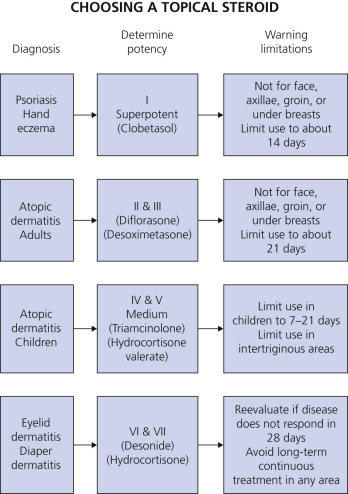
Choosing the Appropriate Strength.
Guidelines for choosing the appropriate strength and brand of topical steroid are presented in Table 2.2 and Fig. 2.2 . The best results are obtained when preparations of adequate strength are used for a specified length of time. Weaker, “safer” strengths often fail to provide adequate control. Patients who do not respond after 1 to 4 weeks of treatment should be reevaluated.
| Groups I–II | Groups III–V | Groups VI–VII |
|---|---|---|
| Psoriasis | Atopic dermatitis | Dermatitis (eyelids) |
| Lichen planus | Nummular eczema | Dermatitis (diaper area) |
| Discoid lupus † | Asteatotic eczema | Mild dermatitis (face) |
| Severe hand eczema | Stasis dermatitis | Mild anal inflammation |
| Poison ivy (severe) | Seborrheic dermatitis | Mild intertrigo |
| Lichen simplex chronicus | Lichen sclerosus et atrophicus (vulva) | |
| Hyperkeratotic eczema | Intertrigo (brief course) | |
| Chapped feet | Tinea (brief course to control inflammation) | |
| Lichen sclerosus et atrophicus (skin) | Scabies (after scabicide) | |
| Alopecia areata | Intertrigo (severe cases) | |
| Nummular eczema (severe) | Anal inflammation (severe cases) | |
| Atopic dermatitis (resistant adult cases) | Severe dermatitis (face) |
* Stop treatment, change to less potent agent, or use intermittent treatment once inflammation is controlled.
Megapotent Topical Steroids (Group I)
Clobetasol propionate, halobetasol propionate, betamethasone dipropionate, and diflorasone diacetate are the most potent topical steroids available. Clobetasol and halobetasol are the most potent and betamethasone and diflorasone are equipotent.
In general, no more than 45 to 60 grams (g) of cream or ointment should be used each week ( Table 2.3 ). Side effects are minimized and efficacy increased when medication is applied once or twice daily for 2 weeks followed by 1 week of rest. This cyclic schedule (pulse dosing) is continued until resolution occurs. Intermittent dosing (e.g., once or twice a week) can lead to a prolonged remission of psoriasis if used after initial clearing. Alternatively, intermittent use of a weaker topical steroid can be used for maintenance. Diflorasone can be used with plastic dressing occlusion; clobetasol, halobetasol, and betamethasone should not be used with occlusive dressings.
| Length of Therapy | Grams Per Week | Use Under Occlusion | |
|---|---|---|---|
| Clobetasol propionate | 14 days | 60 | No |
| Clobetasol scalp solution | 14 days | 50 mL | No |
| Clobetasol foam | 14 days | 50 | No |
| Halobetasol propionate | 14 days | 60 | No |
| Betamethasone dipropionate | Unrestricted | 45 | No |
| Diflorasone diacetate | Unrestricted | Unrestricted | Unrestricted |
Patients must be monitored carefully. Side effects such as skin atrophy and adrenal suppression are a real possibility, especially with unsupervised use of these medications. Refills should be strictly limited. Add the warning “Not to be applied to face, axillae and groin” to prescriptions for treatment of other areas. Explain that prolonged use causes a poststeroid flare of erythema and papules on the face and atrophy in the axillae and groin.
Concentration.
The concentration of steroid listed on the tube cannot be used to compare its strength with other steroids. Some steroids are much more powerful than others and need be present only in small concentrations to produce the maximum effect. Nevertheless, it is difficult to convince some patients that clobetasol cream 0.05% (group I) is more potent than hydrocortisone 1% (group VII).
It is unnecessary to learn many steroid brand names. Familiarity with one preparation from groups II, V, and VII gives you the ability to safely and effectively treat any steroid-responsive skin disease. Most of the topical steroids are fluorinated (i.e., a fluorine atom has been added to the hydrocortisone molecule). Fluorination increases potency and the possibility of side effects. Products such as hydrocortisone valerate cream have increased potency without fluorination; however, side effects are possible with this midpotency steroid.
Compounding.
Avoid having the pharmacist prepare or dilute topical steroid creams. The active ingredient may not be dispersed uniformly, resulting in a cream of variable strength. The cost of pharmacist preparation is generally higher because of the additional labor required. High-quality steroid creams, such as triamcinolone acetonide, are available in large quantities at a low cost.
Generic Versus Brand Names.
Many generic topical steroid formulations are available (e.g., clobetasol propionate, betamethasone valerate, betamethasone dipropionate, fluocinolone acetonide, fluocinonide, hydrocortisone, and triamcinolone acetonide). In many states, generic substitutions by the pharmacist are allowed unless the physician writes “no substitution.” Vasoconstrictor assays have shown large differences in the activity of generic formulations compared with brand-name equivalents: many are inferior, a few are equivalent, and a few are more potent than brand-name equivalents. Many generic topical steroids have vehicles with different ingredients (e.g., preservatives) than brand-name equivalents.
Vehicle
The vehicle, or base, is the substance in which the active ingredient is dispersed. The base determines the rate at which the active ingredient is absorbed through the skin. Components of some bases may cause irritation or allergy.
Creams.
The cream base is a mixture of several different organic chemicals (oils) and water, and it usually contains a preservative. Creams have the following characteristics:
- •
White color and somewhat greasy texture
- •
Components that may cause irritation, stinging, and allergy
- •
High versatility (i.e., may be used in nearly any area); therefore creams are the base most often prescribed
- •
Possible drying effect with continued use; therefore best for acute exudative inflammation
- •
Most useful for intertriginous areas (e.g., groin, rectal area, and axilla)
Ointments.
The ointment base contains a limited number of organic compounds consisting primarily of greases such as petroleum jelly, with little or no water. Many ointments are preservative-free. Ointments have the following characteristics:
- •
Translucent (look like petroleum jelly)
- •
Greasy feeling that persists on skin surface
- •
More lubrication, thus desirable for drier lesions
- •
Greater penetration of medicine than creams and therefore enhanced potency (see inside front matter; triamcinolone cream in group V and triamcinolone ointment in group IV)
- •
Too occlusive for acute (exudative) eczematous inflammation or for use in intertriginous areas, such as the groin
Gels.
Gels are greaseless mixtures of propylene glycol and water; some also contain alcohol. Gels have the following characteristics:
- •
A clear base, sometimes with a jelly-like consistency
- •
Useful for acute exudative inflammation, such as poison ivy, and in scalp areas where other vehicles mat the hair
Solutions and Lotions.
Solutions may contain water and alcohol, as well as other chemicals. Solutions have the following characteristics:
- •
Clear or milky appearance
- •
Most useful for scalp because they penetrate easily through hair, leaving no residue
- •
May result in stinging and drying when applied to intertriginous areas, such as the groin
Foams.
A foam preparation of desonide (Verdeso), betamethasone valerate (Luxiq), and clobetasol propionate (Olux-E) is available. Generic foams are now available. Olux contains a superpotent steroid. Treatment beyond 2 consecutive weeks is not recommended, and the total dosage should not exceed 50 g per week because of the potential for the drug to suppress the hypothalamic–pituitary–adrenal (HPA) axis. Use in children younger than 12 years is not recommended. Foams spread between the strands of hair until they reach the scalp, where the foam melts and delivers the active drug. Foams are useful for treatment of scalp dermatoses and in other areas for acute eczematous inflammation such as poison ivy and plaque psoriasis. Foams may cause stinging shortly after they are applied. Emollient foams such as Verdeso and Olux-E do not sting.
Steroid–Antibiotic Mixtures
Lotrisone Cream and Lotion.
Lotrisone cream contains a combination of the antifungal agent clotrimazole and the corticosteroid betamethasone dipropionate. It is indicated for the topical treatment of tinea pedis, tinea cruris, and tinea corporis. This product is used by many physicians as their topical antiinflammatory agent of first choice. Most inflammatory skin disease is not infected or contaminated by fungus. Lotrisone is a marginal drug for cutaneous fungal infections. Brand-name Lotrisone cream is no longer available; it has been replaced by a brand-name lotion.
Other Antibiotics and Corticosteroid Mixtures.
Mycolog II (nystatin/triamcinolone acetonide) is indicated for the treatment of cutaneous candidiasis. Nystatin does not treat fungi that cause tinea pedis. The majority of steroid-responsive skin diseases can be managed successfully without topical antibiotics.
Amount of Cream to Dispense
The amount of cream dispensed is very important. Patients do not appreciate being prescribed a $90, 60-g tube of cream to treat a small area of hand dermatitis. Unrestricted and unsupervised use of potent steroid creams can lead to side effects. Patients rely on the physician’s judgment to determine the correct amount of topical medicine. If too small a quantity is prescribed, patients may conclude that the treatment did not work. It is advisable to allow for a sufficient amount of cream, and then to set limits on duration and frequency of application. Many steroids (e.g., triamcinolone, hydrocortisone) are available in generic form. They are purchased in bulk by the pharmacist and can be dispensed in large quantities at considerable savings.
The amount of cream required to cover a certain area can be calculated by remembering that 1 g of cream covers 100 square centimeters of skin. The entire skin surface of the average-sized adult is covered by 20 to 30 g of cream.
The fingertip unit and the rule of hand provide the means to assess how much cream to dispense and apply.
Fingertip Unit.
A fingertip unit (FTU) is the amount of ointment expressed from a tube with a 5-mm diameter nozzle, applied from the distal skin crease to the tip of the index finger. One FTU weighs approximately 0.5 g.
The Rule of Hand.
The hand area can be used to estimate the total area of involvement of a skin disease and to assess the amount of ointment required. The area of one side of the hand is defined as 1 hand area. One hand area of involved skin requires 0.5 FTU or 0.25 g of ointment, or 4 hand areas equal 2 FTUs, which equals 1 g. The area of one side of the hand represents approximately 1% of the body surface area, so it requires 1 FTU (2 hand units) to cover 2% of the body surface. Approximately 282 g is required for twice-daily applications to the total body surface (except the scalp) for 1 week.
Application
Frequency
Tachyphylaxis.
Tachyphylaxis refers to the decrease in responsiveness to a drug as a result of enzyme induction. The term is used in dermatology in reference to acute tolerance to the vasoconstrictive action of topically applied corticosteroids. Experiments have revealed that vasoconstriction decreases progressively when a potent topical steroid is applied to the skin three times a day for 4 days. The vasoconstrictive response returned 4 days after termination of therapy. These experiments support years of complaints by patients about initially dramatic responses to new topical steroids that diminish with constant use. It would therefore seem reasonable to instruct patients to apply creams on an interrupted schedule.
Intermittent Dosing
Group I Topical Steroids.
Optimum dosing schedules for the use of potent topical steroids have not been determined. Studies show that steroid-resistant diseases, such as plaque psoriasis and hand eczema, respond most effectively when clobetasol is applied twice a day for 2 to 3 weeks. Treatment is resumed after 1 week of rest. The schedule of 2 weeks of treatment followed by 1 week of rest is repeated until the lesions have cleared.
Intermittent treatment of healed lesions can lead to prolonged remission. Psoriatic patients with lingering erythema remained clear with applications three times a day on 1 day a week. Twice-weekly applications of clobetasol kept 75% of psoriatic patients and 70% of hand eczema patients in remission.
Short weekly bursts of topical corticosteroids may play a role in keeping an adult’s atopic dermatitis under control. Weekly applications of fluticasone ointment (Cutivate), applied once daily for 2 consecutive days each week, maintained the improvements achieved after the initial treatment phase and delayed relapse.
Groups II Through VII Topical Steroids.
The optimum frequency of application and duration of treatment for topical steroids have not been determined. Adequate results and acceptable patient compliance occur when the following steps are taken:
- 1.
Apply groups II through VII topical steroids twice each day.
- 2.
Limit the duration of application to 2 to 6 weeks.
- 3.
If adequate control is not achieved, stop treatment for 4 to 7 days and begin another course of treatment.
Methods
Simple Application.
Creams and ointments should be applied in thin layers and slowly massaged into the site one to four times a day. It is unnecessary to wash the site before each application. Continue treatment until the lesion is clear. Many patients decrease the frequency of applications or stop entirely when lesions appear to improve quickly. Other patients are so impressed with the efficacy of these agents that they continue treatment after the disease has resolved in order to prevent recurrence; adverse reactions may follow this practice.
Different skin surfaces vary in the ability to absorb topical medicine. The thin eyelid skin heals quickly with group VI or VII steroids, whereas the thicker skin on the palms and soles offers a greater barrier to the penetration of topical medicine and requires more potent therapy. Intertriginous (skin touches skin) areas (e.g., axilla, groin, rectal area, and underneath the breasts) respond more quickly to creams that are weaker in strength. The apposition of two skin surfaces performs the same function as an occlusive dressing, which greatly enhances penetration. The skin of infants and young children is more receptive to topical medicine and responds quickly to weaker creams. A baby’s diaper has the same occlusive effect as covering with a plastic dressing. Penetration of steroid creams is greatly enhanced; therefore only group V, VI, or VII preparations should be used under a diaper. Inflamed skin absorbs topical medicines much more efficiently. This explains why red, inflamed areas generally have such a rapid initial response when treated with weaker topical steroids.
Occlusion.
Occlusion with a plastic dressing (e.g., Saran wrap) is an effective method for enhancing absorption of topical steroids. The plastic dressing holds perspiration against the skin surface, which hydrates the top layer of the epidermis – the stratum corneum. Topical medication penetrates a moist stratum corneum from 10 to 100 times more effectively than it penetrates dry skin. Eruptions that are resistant to simple application may heal quickly with the introduction of a plastic dressing. Nearly any area can be occluded; the entire body may be occluded with a vinyl exercise suit, available at most sporting goods stores and, big box stores (Walmart) and online.
Discretion should be used with occlusion. Occlusion of moist areas may encourage the rapid development of infection. Occlusive dressings are used more often with creams than with ointments, but ointments may be covered if the lesions are particularly dry. Weaker, less expensive products (e.g., triamcinolone cream 0.1%) provide excellent results. Large quantities of this medicine may be purchased at a substantial savings.
Method of Occlusion.
The area should be cleaned with mild soap and water. Antibacterial soaps are unnecessary. The medicine is gently rubbed into the lesions, and the entire area is covered with plastic (e.g., Saran wrap, Handi-Wrap, plastic bags, or gloves; Figs. 2.3 to 2.5 ). The plastic dressing should be secured with tape so that it is close to the skin and the ends are sealed; an airtight dressing is unnecessary. The plastic may be held in place with an Ace bandage or a sock. The best results are obtained if the dressing remains in place for at least 2 hours. Many patients find that bedtime is the most convenient time to wear a plastic dressing and therefore wear it for 8 hours. More medicine is applied shortly after the dressing is removed and while the skin is still moist.



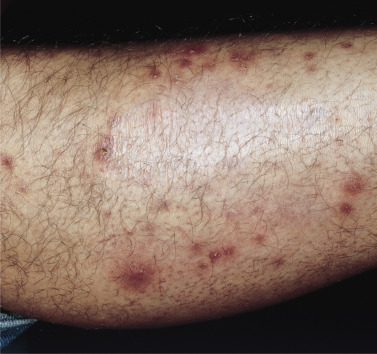
Dressings should not remain on the area continuously because infection or follicular occlusion may result. If an occluded area suddenly becomes worse or pustules develop, infection, usually with Staphylococci, should be suspected ( Fig. 2.6 ). Oral anti-staphylococcal antibiotics should be given (e.g., cephalexin [Keflex] 500 mg two to four times a day).
A reasonable occlusion schedule is twice daily for a 2-hour period or for 8 hours at bedtime, with simple application once or twice during the day.
Occluded areas often become dry, and the use of lubricating cream or lotion should be encouraged. Cream or lotion may be applied shortly after medicine is applied, when the plastic dressing is removed, or at other convenient times.
Systemic Absorption
The possibility of producing systemic side effects from absorption of topical steroids is of concern to all physicians who prescribe these agents ( Table 2.4 ). Topical corticosteroids can cause iatrogenic Cushing disease and adrenal suppression. Populations at greater risk are infants and young children, patients with an impaired cutaneous barrier, and patients in whom highly potent corticosteroids are applied over large areas or under occlusion. The risk of systemic absorption can be reduced by using pulse application of more potent corticosteroids (weekends only or 2 weeks on/1 week off), by using medication “holidays,” by using the minimally effective strength and dose of medication, and by using steroid-sparing agents.
| Ocular | Glaucoma, loss of vision, posterior subcapsular cataracts |
| Metabolic | Hyperglycemia, latent diabetes mellitus, avascular necrosis of femoral head, reduced bone mineral density, decreased growth rate in infants and children, hypothalamic–pituitary–adrenal axis suppression, glucose intolerance |
| Endocrine | Iatrogenic Cushing syndrome, centripetal obesity, striae, moon face, buffalo hump |
| Electrolyte balance | Edema, hypocalcemia, hypertension |
Avoid Weaker, “Safe” Preparations.
In an attempt to avoid complications, physicians often choose a weaker steroid preparation than that indicated; these weaker preparations all too frequently fall short of expectations and fail to give the desired antiinflammatory effect. The disease does not improve, but rather becomes worse because of the time wasted using the ineffective cream. Pruritus continues, infection may develop, and the patient becomes frustrated. Treatment of intense inflammation with hydrocortisone cream 0.5% is a waste of time and money. Generally, a topical steroid of adequate strength (see Table 2.2 ) should be used two to four times daily for a specific length of time, such as 7 to 21 days, in order to obtain rapid control. Even during this short interval, adrenal suppression may result when steroids in groups I through III are used to treat wide areas of inflamed skin. This suppression of the HPA axis is generally reversible in 24 hours and is very unlikely to produce side effects characteristic of long-term systemic use.
Children.
Many physicians are concerned about systemic absorption and will not use any topical steroids stronger than 1% hydrocortisone on infants. The group V topical steroid fluticasone propionate cream 0.05% (Cutivate) appears to be safe for the treatment of severe eczema for up to 4 weeks in children 3 months of age and older. Children between 3 months and 6 years with moderate to severe atopic dermatitis (≥35% body surface area; mean body surface area treated, 64%) were treated with fluticasone propionate cream 0.05% twice daily for 3 to 4 weeks. Mean cortisol levels were similar at baseline and at the end of treatment. The relative safety of moderately strong topical steroids and their relative freedom from serious systemic toxicity despite widespread use in the very young have been clearly demonstrated. Patients should be treated for a specific length of time with a medication of appropriate strength. Steroid creams should not be used continually for many weeks, and patients who do not respond in a predictable fashion should be reevaluated.
Group I topical steroids should be avoided in prepubertal children. Use only group VI or VII steroids in the diaper area and for only 3 to 10 days. Monitor growth parameters in children prescribed chronic topical glucocorticoid therapy.
Adults.
Suppression may occur during short intervals of treatment with group I or II topical steroids, but recovery is rapid when treatment is discontinued. Physicians may prescribe strong agents when appropriate, but the patient must be cautioned that the agent should be used only for the length of time dictated.
Adverse Reactions
Because information concerning the potential dangers of potent topical steroids has been so widely disseminated, some physicians have stopped prescribing them. Topical steroids have been used for decades with an excellent safety record. They do, however, have the potential to produce a number of adverse reactions. Once these are understood, the most appropriate strength steroid can be prescribed confidently. Reported adverse reactions to topical steroids are listed in Box 2.2 . A brief description of some of the more important adverse reactions is presented in the following pages.
- •
Rosacea, perioral dermatitis, acne
- •
Skin atrophy with telangiectasia, stellate pseudoscars (arms), purpura, striae (from anatomic occlusion, e.g., groin)
- •
Tinea incognito, impetigo incognito, scabies incognito
- •
Ocular hypertension, glaucoma, cataracts
- •
Allergic contact dermatitis
- •
Systemic absorption
- •
Burning, itching, irritation, dryness caused by vehicle (e.g., propylene glycol)
- •
Miliaria and folliculitis following occlusion with plastic dressing
- •
Skin blanching from acute vasoconstriction
- •
Rebound phenomenon (e.g., psoriasis becomes worse after treatment is stopped)
- •
Nonhealing leg ulcers; steroids applied to any leg ulcer retard healing process
- •
Hypopigmentation
- •
Hypertrichosis of face
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








