I. GENERAL PRINCIPLES
A. Function and goals of reconstruction
1. Function
a. *Thumb contributes 40% of the hand function.
b. Essential for prehensile hand function
c. Requires contact between the index and the thumb pulp to achieve tripod pinch, fine motor dexterity, and cylinder grasp
2. Goals
a. Adequate length for opposition
b. Mobility and stability for opposition, flexion, and pinch
i. Carpometacarpophalangeal (CMC) mobility is essential for normal function. If this cannot be achieved, CMC arthrodesis in full abduction-opposition.
ii. Interphalangeal (IP) and metacarpophalangeal (MP) joint contribute less to overall function.
c. Sensation
i. Freedom from pain
ii. Protection
iii. Ability to effectively function (e.g., pinch)
d. Adequate and durable soft-tissue coverage
e. Aesthetic appearance
B. Patient assessment
1. Occupation
2. Hand dominance
3. Age: Young patients have greater neural plasticity compared with adults.
4. Health and comorbid conditions
5. Associated injuries
C. Injury assessment
1. Nature and timing of the injury
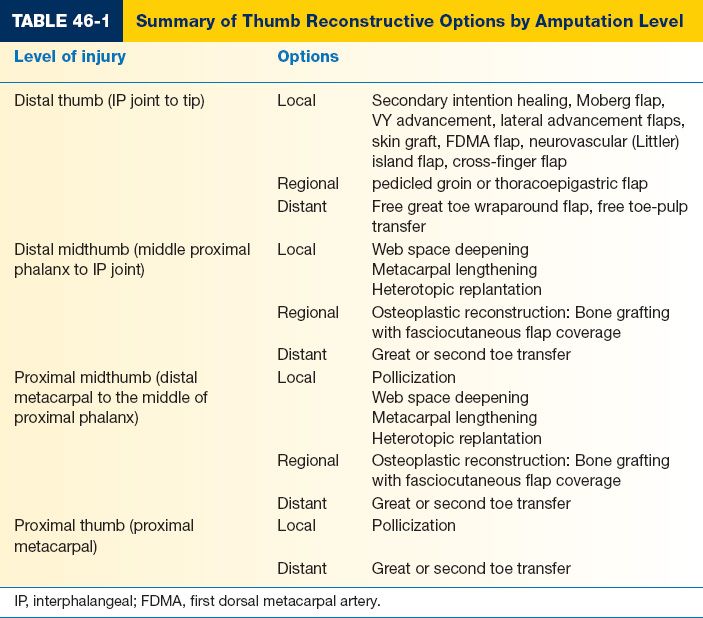
2. Level of injury (Table 46-1)
3. Presence of web space contracture
4. Status of the CMC joint
5. Lister classification
a. Soft-tissue loss with adequate length
b. Subtotal amputation with uncertain remaining length
c. Total amputation with intact CMC joint
d. Total amputation with loss of CMC joint
6. Radiographs: Three views (lateral, anteroposterior, and oblique) incorporating the CMC joint
II. RECONSTRUCTIVE OPTIONS
A. Soft-tissue loss with adequate length
1. General principles
a. Goals
i. Achieve durable, sensate, and painless coverage.
ii. Preserve length, but not as the expense of stable coverage.
b. Reconstructive options are dictated by the size of the defect.
______________
*Denotes common in-service examination topics
2. Small defects: <1 cm2
a. Healing by secondary intention
i. Preserves sensation with minimal resultant defect
ii. May require painful and prolonged wound care
b. Local flaps
i. VY advancement
ii. Lateral advancement
c. Skin grafts
i. More rapid healing, but insensate
3. Larger defects: >1 cm2, >50% of volar pad, exposed periosteum, bone, and tendon
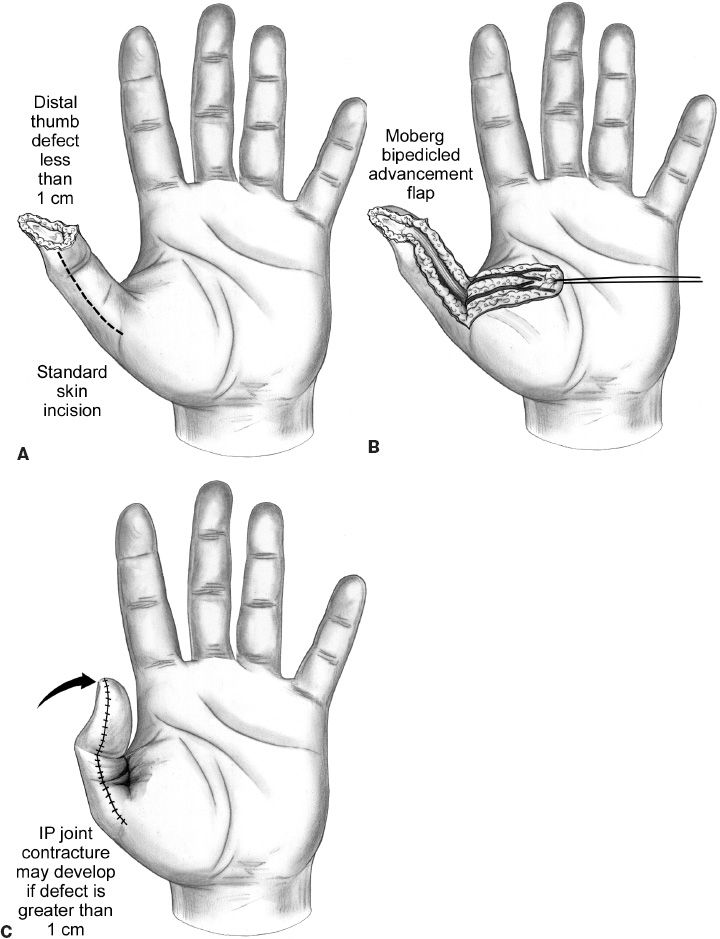
a. Palmar advancement (“Moberg” flap) (Fig. 46-1)
i. Sensate flap that is ideal for defects 1 to 2 cm2 of the volar pad
ii. Advances a palmar flap containing both neurovascular bundles
iii. *May require up to 45 degrees of IP joint flexion to achieve coverage, which may lead to long-term flexion contracture.
iv. Defects that require more than 1.5 cm of advancement or to minimize IP flexion can be covered using a proximal releasing incision—still limited by neurovascular bundles
b. Heterodigital flaps: Indicated for defects >2.5 cm2 or for loss of the entire volar pad
i. Cross-finger flap
a) Ideal for defects involving the entire palmar surface of the thumb distal to the IP joint.
b) A pedicled flap of nonglabrous is designed from the dorsal proximal phalanx of the index finger, which is divided and inset after 2 to 3 weeks. A skin graft is used to cover the donor defect.
Figure 46-1. Standard elevation technique for the Moberg flap. The dissection plane is just above the flexor tendon sheath, elevating the neurovascular bundles with the flap. A: The skin incision is planned in the midlateral line on both sides of the thumb. B: The flap is elevated, raising the neurovascualar bundles in the flap. C: The thumb is flexed, permitting the tip of the flap to reach the end of the defect. IP, interphalangeal. (From Berger RA, Weiss AC, ed. Hand Surgery. Philadelphia, PA: Lippincott Williams & Wilkins; 2004.)
c) Can be innervated as long as dorsal radial sensory branch is transferred to ulnar side of the thumb at inset
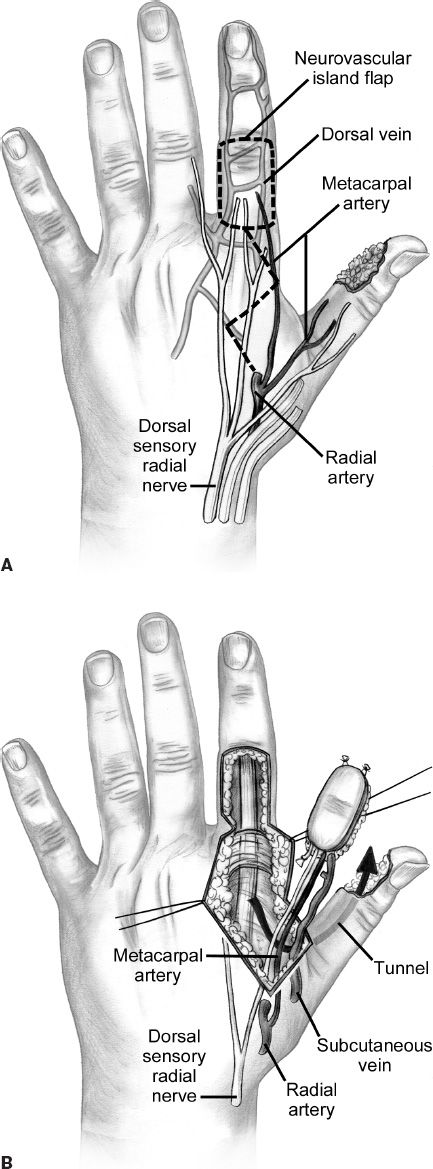
ii. First dorsal metacarpal artery (FDMA) flap (Fig. 46-2)
a) *An innervated, pedicled island flap transferring the FDMA, subcutaneous veins, dorsal branch of the radial sensory nerve, and skin from the index finger.
b) Pedicle runs under the first dorsal interosseous fascia and sometimes within the muscle.
c) First dorsal metatarsal artery is usually branch off of radial artery.
d) Donor site is covered with a full-thickness skin graft
e) Can cover both dorsal and palmar defects
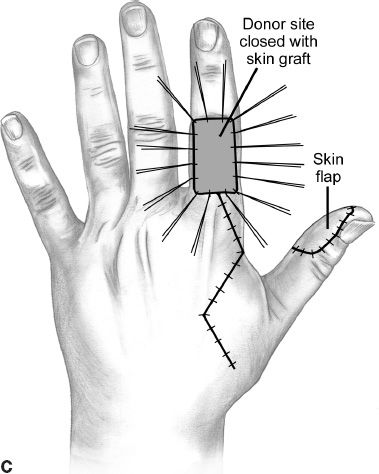
Figure 46-2. The first dorsal metacarpal artery flap is elevated off the dorsum of the index proximal phalanx and can provide coverage for the volar and dorsal thumb. The donor site is skin grafted. A: The skin is marked to incorporate the vascular supply of the first dorsal metacarpal artery flap. B: The flap is raised, elevating the first dorsal metacarpal artery and the dorsal veins. C: The flap is transposed to the thumb defect through a subcutaneous tunnel and the index finger defect is closed with a skin graft. (From Berger RA, Weiss AC, ed. Hand Surgery. Philadelphia, PA: Lippincott Williams & Wilkins; 2004.)
iii. Neurovascular island flap
a) Pedicled, island flap that transfers the ulnar neurovascular bundle from the middle finger (requires sacrifice of radial neurovascular bundle to ring finger).
b) The ring finger can be used if median nerve is not intact.
c) Greater morbidity due to loss of palmar sensation along the ulnar aspect of the donor digit, as well as scarring and stiffness of the donor digit.
c. Regional flaps
i. Thoracoepigastric flap
ii. Groin flap
d. Free tissue transfer: Wraparound great toe transfer, toe-pulp transfer
e. Revision amputation
i. Indicated only when stability and durable sensate coverage are not feasible
ii. Well tolerated for thumb loss distal to the IP joint, and near normal hand function can be maintained.
B. Subtotal amputation with inadequate length
1. General principles
a. Bone loss proximal to the IP joint results in diminished hand span, poor grasp, and decreased pinch dexterity
b. Injuries proximal to the midportion of the proximal phalanx may not achieve adequate length through phalangization procedures, and techniques to reconstruct an opposable thumb described in the next section may also be indicated.
2. “Phalangization”: To deepen first web space
a. Z-plasty techniques
i. Requires at least one-half of the proximal phalanx intact, minimal soft-tissue scarring, a mobile first metacarpal, and no muscle contracture.
ii. Options include two-flap (60 degree angle), four-flap, or five-flap Z-plasty techniques.
i. Ideal in cases with extensive scarring.
ii. Full-thickness skin grafting provides donor site coverage.
iii. May use external fixator or supplemental K wires to hold the first web space in abduction during healing.
c. Regional flap coverage
i. Distally based posterior interosseous flap (PIA).
a) PIA is usually branch off of common interosseous artery and ocasionally direct branch of ulnar artery.
b) In its proximal third, PIA lies deep to septum on the abductor pollicis longus with posterior interosseous nerve.
c) PIA pierces interosseous membrane 1/3 way down from elbow at junction of middle and proximal 1/3.
d) PIA pierces supinator and runs between EDQ and ECU.
e) Gives off large perforator in its middle third which should be included in flap.
f) Flap centered over line between humeral lateral epicondyle and distal radioulnar joint when arm is flexed 90 degrees. Place skin paddle at middle and distal 1/3 of this line.
ii. Distally based radial forearm flap
3. Osteoplastic reconstruction
a. Bone grafting (e.g., tricortical iliac crest) with fasciocutaneous flap coverage (e.g., FDMA, radial forearm flap, and groin flap)
b. Requires stable CMC joint with good mobility
c. Difficult to achieve sensory reinnervation and bony resorption common
C. Total amputation with preservation of the basal joint
1. Toe-to-hand transfer
a. Ideal if MP joint is intact
b. The great toe or second toe can be transferred to the thumb position and there is controversy among authors regarding preference.
i. Great toe is bulkier than the thumb, disfigures foot; good strength
ii. Second toe is smaller than the thumb, but minimal donor site
c. Anatomy can be variable: In general, the first dorsal metatarsal artery (FDMA) supplies the great and second toe; venous drainage provided by superficial dorsal veins to the saphenous vein; nerve supply from the plantar digital nerves from the medial plantar nerve.
i. Type 1a: FDMA is superficial to the first dorsal interosseous muscle
ii. Type 1b: FDMA is within the superficial portion of the first dorsal interosseous muscle.
iii. Type II: FDMA is deep to the first dorsal interosseous muscle and superficial to the deep intermetatarsal ligament.
iv. Type III: FDMA is diminutive and does not contribute to the plantar communicating branch. Instead, the first plantar metatarsal artery is larger and is used as the donor vessel.
2. Osteoplastic reconstruction: See above
3. Distraction lengthening
a. Osteotomy is created at the base of the metacarpal and lengthening at 1.0 to 1.5 mm per day
b. Can achieve up to 4 cm in length
c. May require additional Z-plasty soft-tissue release
4. Pollicization
a. Can transfer the index, middle, or ring finger to the thumb position as an island flap based on the digital neurovascular bundle
b. The metacarpal is shortened, and the digit is pronated 120 to 130 degrees and abducted palmarly to create adequate opposition
c. The index finger is most commonly substituted
i. Extensor indicis → extensor pollicis longus
ii. Extensor digitorum communis → abductor pollicis longus
iii. First palmar interosseous → adductor pollicis
iv. First dorsal interosseous → abductor pollicis brevis
5. Heterodigital replantation
a. “Spare parts” approach to transfer an injured ray or digit to the thumb position for immediate reconstruction
b. Can also be banked for delayed reconstruction
D. Total loss with destruction of the basal joint
1. Pollicization
2. Free digit transfer (e.g., ring finger) with arthrodesis of the basal joint in opposition
PEARLS
1. The majority of thumb reconstructive procedures are performed in a delayed or elective fashion. Therefore, it is essential for patients to be actively involved in the decision for surgery in order to address their expectations for recovery as realistically as possible.
2. Toe transfer procedures are technically demanding, but often suitable reconstructive options for a variety of injuries.
3. Prosthetics can offer restoration of function for those patients who do not desire or who are not candidates for thumb reconstruction.
QUESTIONS YOU WILL BE ASKED
1. How much does the thumb contribute to overall hand function?
Thumb contributes 40% of hand function.
2. Why are children with Blauth type V congenital thumb hypoplasia offered pollicization instead of great toe transfer?
They lack a CMC joint to articulate the digit on.
3. Where is the FDMA locate?
Within the fascia of the first dorsal interosseous muscle.
4. What artery is sacrificed when using an island flap from the ulnar middle finger?
Radial digital artery to the ring finger.
Recommended Readings
Buncke GM, Buncke HJ, Lee CK. Great toe-to-thumb microvascular transplantation after traumatic amputation. Hand Clin. 2007;23(1):105–115. PMID: 17478257.
Heitmann C, Levin LS. Alternatives to thumb replantation. Plast Reconstr Surg. 2002;110(6):1492–1503; quiz 1504–1505. PMID: 12409769.
Henry SL, Wei FC. Thumb reconstruction with toe transfer. J Hand Microsurg. 2010;2(2):72–78. PMID: 22282672.
Wei FC, Jain V, Chen SH. Toe-to-hand transplantation. Hand Clin. 2003;19(1):165–175. PMID: 12683453.
< div class='tao-gold-member'>