FINGERTIP AND NAILBED INJURIES
I. OVERVIEW
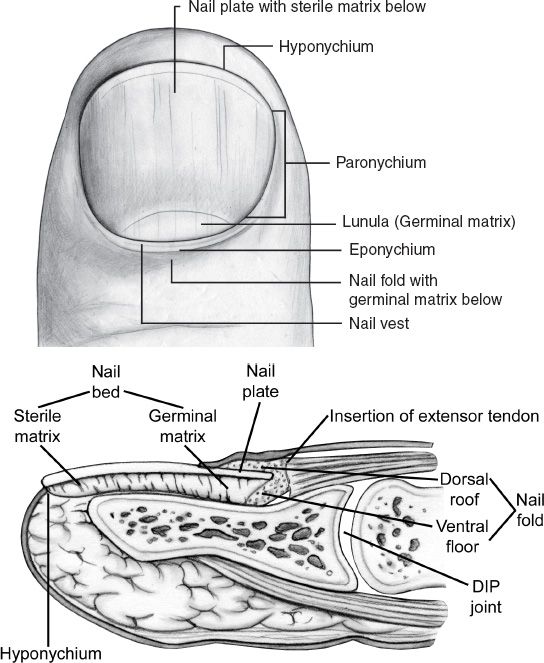
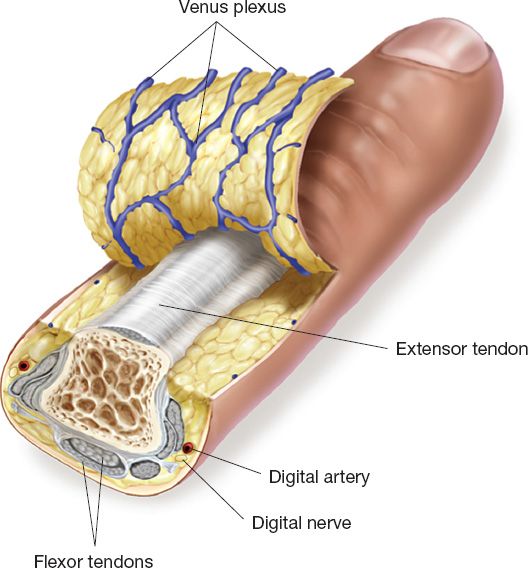
A. The part of the digit distal to distal interphalangeal (DIP) joint is considered the fingertip (Fig. 41-1).
B. The glabrous skin on the fingertip is specialized for pinch and grasp functions.
C. The nail gives protection of distal phalanx and counterforce to tip pulp.
D. Fingertips are essential for normal hand appearance.
E. Fingertips are commonly injured
1. Fingertip and nail injuries account for 45% of all emergency department (ED) hand injuries.
2. The middle fingertip is most commonly injured, followed by the ring fingertip
3. Thumb tip injury is least common.
F. Fingertip injuries can have a great impact
1. May appear minor, but can have serious implications because of the effect on so many activities.
2. Typically result in lost work (sometimes the end of a career).
G. Immediate repair is preferable for the best outcome. Repair can often be performed in the emergency room.
II. PREPARATION AND EXAMINATION
A. Surgical loupes are helpful
B. A digital nerve block is usually sufficient
C. Ensure adequate lighting in ED procedure room or equivalent
D. Irrigate the fingertip with sterile saline
E. Debride any clearly nonviable tissue
F. Finger tourniquet control
1. Penrose drain or sterile glove with large hemostat insure tourniquet removal
2. Do NOT roll a cut glove finger onto the digit, as this band may be forgotten, leading to ischemic loss of digit.
G. Have a low threshold for moving to the OR when necessary, and use sedation when needed, especially with children.
III. FINGERNAIL INJURIES
A. Nailbed hematomas
1. *If <50% of surface of the nail in size, incise and drain by lancing the nail with cautery or an 18G needle.
2. If >50%, remove the nail to repair the nailbed.
B. Nailbed lacerations
1. Obtain X-rays to rule out open fracture
a. Treat with antibiotics for nailbed lacerations with distal phalanx fractures (open fracture).
b. Immobilize stable fractures, consider operative fixation for unstable fractures to protect the nailbed repair.
______________
*Denotes common in-service examination topics
Figure 41-1. Fingertip and nailbed anatomy. (From Berger RA, Weiss AC, ed. Hand Surgery. Philadelphia, PA: Lippincott Williams & Wilkins; 2004).
2. Use a Freer elevator or tenotomy scissors to separate the nail from the eponychium and underlying matrix.
3. If nail plate is intact, place into Betadine solution for later replacement into nail fold.
4. Repair the nailbed (i.e., sterile matrix) with 6-0 or 7-0 absorbable suture material. Use precise, interrupted stitches, under loupe magnification.
5. Can maintain the eponychial fold by replacing nail (or foil from suture pack).
6. 2-Octylcyanoacrylate (Dermabond) has been shown to significantly decrease time required to repair nailbed injuries.
C. Avulsed nailbed
1. If attached to nail, replace as an onlay graft
2. *If the nailbed is missing and results in nail deformity, use a split-thickness nailbed graft from another (toe)nail to fill the defect (usually electively).
3. *Without grafting, nail will be non-adherent and risks bony infection.
D. Amputations through the lunula/germinal matrix: If unable to repair/replant, remove remaining germinal matrix before closure. Otherwise, the remaining matrix can form an irritating painful nail remnant.
E. Seymour fractures
1. In pediatric population, fracture through distal phalanx physis can entrap nail-fold, preventing reduction.
3. Often presents with benign looking proximal nail avulsion.
4. Operative I&D, reduction and nailbed repair usually required.
IV. DISTAL FINGER INJURIES
A. Assess injury
1. Dorsal versus volar
2. Angle of injury
3. Involvement of nail/nailbed (see below)
4. Exposure of bone
B. If no exposed bone
1. Secondary intention healing
a. Indication: ≤1 cm2
b. Gives the most sensate fingertip in most cases
c. Treat with dressing changes and antibiotic ointment to keep moist and clean.
d. Cold intolerance is common, but no worse than with other treatment options.
2. Primary closure is an option only if tissue loss is minimal; otherwise, tight closures can limit function, cause pain, and create a hooked nail deformity in which the nail bends volarly due to tension of the closure and the loss of distal bone support
3. Skin grafts
a. Recovery of sensation is not as good as with secondary intention healing.
b. If used, the best alternative is a full thickness skin graft. Best donor site options include.
i. Original skin (if salvageable). This skin should be aggressively trimmed of all fat and even some dermis.
ii. Skin from ulnar/hypothenar aspect of hand
iii. Volar wrist skin
iv. Antecubital skin
c. Split thickness skin grafts should only be used on non-critical areas (i.e., ulnar side of index, middle, and ring fingers).
C. If bone is exposed
1. Completion amputation: Bone shortening and primary closure
a. Allows return to work quickly
b. Best option for a patient unlikely or unwilling to do dressing changes
c. *Complications include hook nail deformity if nail bed is pulled tightly into tip closure or with contraction of scar.
2. Bone shortening and healing by secondary intention
a. Patients are often skeptical about outcome initially.
b. Good option if a patient is able to tolerate dressing changes.
3. Fingertip flaps (see below)
a. Many described surgical options; however, these procedures will not necessarily result in better outcomes or quicker recovery.
b. Individual patient presentation, and the surgeon’s preference and expertise, play large roles in determining treatment method to use.
V. FLAPS FOR FINGERTIP REPAIR
A. Healing by secondary intention often gives as good or better outcomes than flap repairs.
B. The angle of injury or amputation, as well as individual surgeon experience, determines when and where to use a given technique
C. Advancement flaps
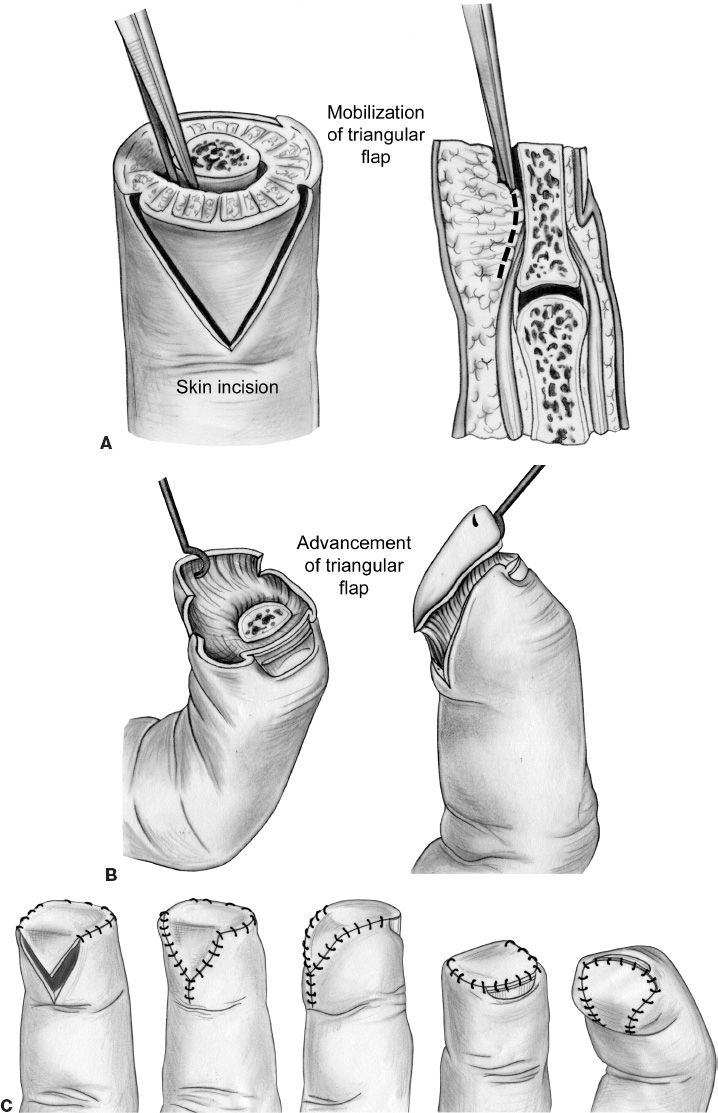
1. *Volar V–Y advancement flap (Atasoy–Kleinert flap) (Fig. 41-2)
a. Indication: Dorsal oblique amputations
b. Triangular flap, with base no wider than nailbed
c. Skin incisions through the dermis; deep aspect dissected off of phalanx
d. Advancement of up to 10 mm
e. Good survival; disadvantages include possible hypersensitivity or hook nail
Figure 41-2. The Atasoy volar V–Y advancement flap. A: The fingertip is debrided, and bone is shortened if necessary. B: A full-thickness triangular palmar flap is developed and advanced to the sterile matrix. C: The skin is then closed as illustrated. (From Berger RA, Weiss AC, ed. Hand Surgery. Philadelphia, PA: Lippincott Williams & Wilkins; 2004).
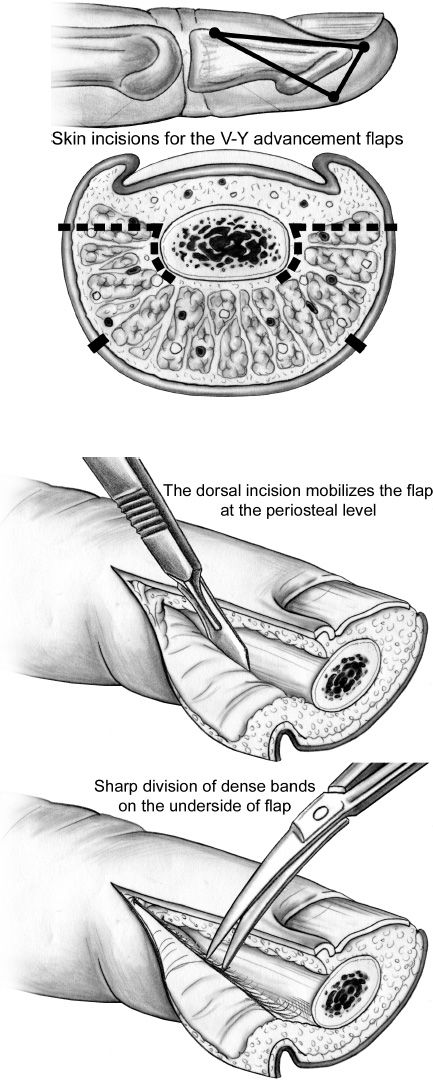
2. *Lateral V–Y advancement flap (Kutler flap) (Fig. 41-3)
a. Indication: Transverse amputations
b. Bilateral triangles: Advanced and sutured to distal nailbed
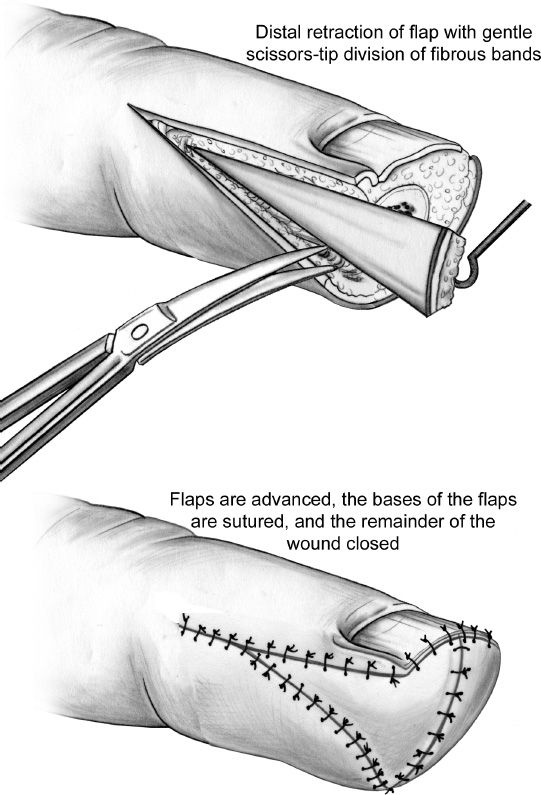
Figure 41-3. The Kutler lateral V–Y advancement flaps. The fingertip is debrided and bone is shortened if necessary. Two lateral full-thickness flaps are developed and advanced as shown. (From Berger RA, Weiss AC, ed. Hand Surgery. Philadelphia, PA: Lippincott Williams & Wilkins; 2004).
c. Can advance up to 5 mm if skin alone; 14 mm if a neurovascular flap is elevated down to the level of the periosteum.
d. Disadvantages
i. Vascular supply is sometimes unreliable
ii. Scar is at the tip; may be painful or insensate
3. Volar neurovascular advancement flap (Moberg flap): (See “Thumb Reconstruction” Chapter 46—Figure 1)
a. *Indication: Thumb tip ampuation >1 cm2, when padding and sensation are critical, and some flexion contracture can be tolerated.
b. Best sensation preservation
c. Longitudinal incisions made on both sides, dorsal to the neurovascular structures. Nerves and arteries are contained in the flap.
d. Advanced to cover tip defect
e. Requires some joint flexion during healing, therefore high risk of flexion contracture.
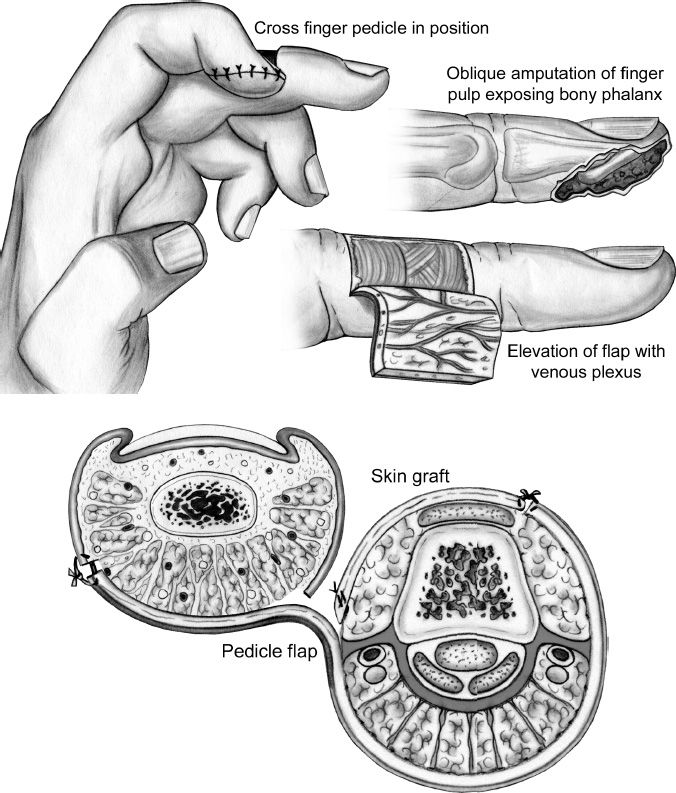
1. Cross finger flap (Fig. 41-4)
a. Indication: Volar defect distal to proximal interphalangeal (PIP).
b. Dorsal skin from one digit is transferred to the injured area of an adjacent digit; can use for volar or dorsal amputations.
c. Pedicled flap with delayed division, usually in 2 to 3 weeks.
d. Donor site requires a skin graft.
Figure 41-4. The cross-finger flap. This flap uses the dorsal skin of an adjacent finger to resurface volar defects. Specifically, the injured finger is debrided. A full-thickness flap of skin and subcutaneous tissue is developed off of the adjacent finger over the middle phalanx. The pedicle is adjacent to the injured finger. The paratenon of the extensor tendon is left intact. The injured finger is flexed slightly, and the flap is sewn to the fingertip; thus, both fingers are temporarily sewn together. Akin graft is sewn over the soft tissue defect created in the adjacent donor finger. A bolster gently holds the skin graft down, allowing for proper adherence. The fingers are separated at 2 to 3 weeks. (From Berger RA, Weiss AC, ed. Hand Surgery. Philadelphia, PA: Lippincott Williams & Wilkins; 2004).
a. *Indication: large fingertip pulp loss >2 cm.
b. The digit injured is flexed and tucked into thenar area, and the palmar skin is used to cover the tip by raising dorsal and volar flaps, division at 2 to 3 weeks.
c. Advantage: No defect on adjacent fingers to injury.
d. Disadvantage: PIP flexion contracture of recipient finger. Therefore mostly used in children, which can resolve the contracture more easily than adults.
3. Neurovascular island transfer flap (Littler flap)
a. Indication: Insensate fingers following trauma to recreate sensibility in the tip.
b. Usually reserved for thumb, index finger, or ulnar little finger.
c. Must balance recipient sensation restoration with donor site loss.
d. Flap pedicle is composed of digital vessels and nerve.
e. Typically raised from the ulnar aspect of the ring or middle finger; raised at level of flexor sheath.
f. Donor site is closed with either graft or primarily. This flap is rarely used because of the high donor site morbidity incurred.
4. Reverse cross finger flap
a. *Indication: Dorsal skin defect from mid-distal phalanx to mid-proximal phalanx.
b. Dorsal subcutaneous tissue skin from donor digit is transferred to the dorsal injury area of an adjacent digit.
c. Pedicled flap with delayed division, usually in 2 to 3 weeks.
d. *Recipient site requires a full-thickness skin graft over subcutaneous tissue; donor site skin is returned to donor site.
AMPUTATION
I. INITIAL ASSESSMENT
A. Level of the injury
B. Mechanism (crush vs. sharp, degloving)
C. Dominant hand?
D. What is the patient’s age? (Children heal more quickly and adapt more easily to changes in form and function.)
E. Smoker? How much?
F. Determine perception of hand image vs. function
G. Manage patient expectation from the start
H. What other injuries exist?
I. Is replantation possible? Is it a worthwhile option (see below)?
II. REVISION AMPUTATION GOALS
A. Preserve function
B. Create a durable amputation site/stump
C. Preserve sensation; prevent neuromas
D. Early return to work and activity
III. PROXIMAL FINGER AMPUTATIONS
A. Amputations through joints (DIP or PIP)
1. The bone end must be debrided. Use a rongeur to smoothly contour the distal end by removing the condylar prominences and irregular bone spikes.
2. Digital nerves must be transected on tension and allowed to retract to prevent neuromas in zone of injury.
3. The extensor and flexor tendons should be debrided, but care should be taken not to suture the ends of them together, as this will limit excursion of both
a. *If the FDP tendon is shortened and tethered, then the quadrigia effect can occur.
i. The FDP tendons share a common muscle belly.
ii. If one tendon is shortened, then the others cannot be fully contracted, leading to the inability to make a fist
i. If the FDP is severed from its insertion and migrates proximally, it pulls on the lumbrical.
ii. Attempts to flex the digit cause PIP extension (from FDP pull on lumbricals tendon, pulling on extensor mechanism).
iii. *Treatment: Sectioning of the lumbrical tendon.
B. Middle and proximal phalanx amputations
1. A “fish mouth” closure of the skin is used, with the incision oriented transversely across the end of the stump.
2. Tendons, when preserved, are secured to their insertion on the phalanx.
3. If an amputation occurs too proximally along the middle phalanx to allow resecuring of the tendon to the bone, or if the tendon is missing, then use of the next joint will be limited. Length preservation remains preferable, even if the joint is nonfunctional. In this case, the joint should be fused.
4. Amputations near the MCP joint often result in problems with small object manipulation, especially in ring and middle finger amputations.
a. Consideration should be given to eventually converting to a ray amputation to maximize function.
b. Alternatively, prosthetic finger replacement is possible.
IV. METACARPAL AND CARPAL AMPUTATIONS
A. Ray amputations
1. Injuries at or near the level of the MCP usually benefit from removal of most of the bone and closure of the space between remaining digits.
a. Amputation of the index finger at the MCP level leaves a stump that can interfere with thumb use and creates a bulky web space.
b. The overall appearance of the hand is better if the stump is removed and any gap closed, although the palm is made narrower in the process.
2. Ray amputations are generally carried out electively at a later time, after the wound has healed.
3. Central ray (middle or ring finger) amputations leave defects, which benefit from closure of the space remaining between the metacarpals.
B. Carpal amputations
1. Initially, the treatment is tissue preservation.
2. Functional recovery is poor. Some patients may opt for more proximal amputation, followed by fitting with a hand prosthesis.
3. Alternatively, the tissue at the hand base can be preserved and used to anchor a non-functional cosmetic appliance.
V. AMPUTATIONS AT AND PROXIMAL TO THE WRIST
A. Wrist disarticulation
1. Once felt to be inferior to a long below-elbow amputation; now performed increasingly, in part because of improvement in prostheses.
2. Preserving the radioulnar joint allows for a full range of pronation and supination.
3. A “fish mouth” skin closure, with a longer skin flap on the palmar side, is used.
B. Below-elbow amputation: The goal is length preservation. More length preservation of the radius and ulna means greater pronation/supination; ideally, 65% to 80% of length should be preserved for maximal function.
C. Elbow and above-elbow amputations
1. Humeral condyle preservation, when possible, allows for translation of rotation to the eventual prosthesis. Therefore, an elbow disarticulation is a very adequate level of amputation.
2. In above-elbow amputations, length preservation is key. Amputations proximally, at or above the axillary fold, have no real advantage versus shoulder disarticulations.
REPLANTATION
I. EVALUATION FOR REPLANTATION
A. “Life before limb”: Patients may have other serious injuries, which must be addressed prior to any attempt at replantation.
B. Assess injury, as outlined above in the “Amputation” section
C. Additional history is needed before considering replantation
1. Overall patient health and comorbidities; smoking and work history
2. Previous injuries to this extremity
3. Willingness of patient to comply with rehabilitation and to tolerate lengthy time off of work (average time until return to work is 7 months), as well as future operations
D. Obtain X-rays of both the hand and the amputated part. Give the patient a tetanus update and/or antibiotics if indicated, check the hematocrit, and perform fluid resuscitation
E. Assess the amputated part and stump site
1. Sharp amputations do better than avulsion or crush amputations.
2. Length of ischemia time of part is critical
a. *Digits can tolerate up to 12 hours of warm or 24 hours (or more) of cold ischemia time.
b. More proximal amputations, which include muscle, tolerate less ischemia: 6 hours of warm ischemia or 12 hours of cold ischemia is considered the limit of viability for wrist or more proximal replantations
II. INDICATIONS FOR REPLANTATION
A. Indications to attempt replantation
1. *Thumb amputations
a. Contributes 40% of function to hand
b. *Consider heterotopic pollicization in multiply amputated fingers when thumb not salvageable.
c. Electively, a toe-to-thumb transfer can be offered as well.
d. Avulsions at the interphalangeal (IP) joint deserve replantation and IP joint fusion as infection rate for replanting EPL and FPL too great.
2. Multiple finger amputations
3. *Any amputation in a child
4. Amputation at the palm, wrist, or forearm level
5. Single digit injury distal to FDS insertion (does well functionally)
B. Absolute contraindications to replantation
1. Life-threatening injuries
2. Prolonged ischemia time of part
3. Part in multiple pieces, that is, transected at more than one level
C. Relative contraindications
1. Severe crush or avulsion amputations
2. Injuries at multiple levels
3. Severe pre-existing illness
a. Diabetes mellitus
b. Heart disease/atherosclerosis
c. Recent stroke/MI
d. Psychiatric disorders
4. Gross contamination of site
5. Prior surgery/trauma to amputated part
6. Smoking history
D. A number of controversies persist
1. Amputation proximal to the elbow: Technically possible, but functional outcomes are quite poor. The success is greater in children.
2. Amputation of single finger proximal to the FDS insertion: Some surgeons feel that poor functional outcome negatively impacts the use of the remaining digits and leads to a less functional situation than amputation.
A. Care of amputated parts: The part should be gently cleaned, wrapped in saline-moistened gauze, and placed in a sealed plastic bag.
B. The bag is stored at 4°C for transport
1. Saline-ice bath will maintain the proper temperature.
2. Do NOT place the finger directly on ice; freezing worse than warm ischemia.
C. Consent
1. Obtaining surgical consent for replant attempts is not trivial
a. The patient/family will likely have unrealistic expectations prior to counseling.
b. The extensive recovery time, the need for rehabilitation and the likely amount of optimal function should be explained in detail prior to replantation attempts.
c. The possibility of long hospitalizations, multiple operations, heparinization, and blood transfusions must be recognized.
d. The significant chance of failure must also be addressed.
2. The surgeon must inform the patient that further reconstruction may be needed, including
a. Vein graft
b. Nerve graft
c. Skin graft
d. Muscle flap for coverage
e. Revision amputation
IV. OPERATIVE TECHNIQUES
A. Amputated part (Fig. 41-5)
1. Begin work preparing the amputated part on the “back table” prior to patient arrival
Figure 41-5. Anatomy of the amputated finger. Knowing the anatomy of the amputated digit will make replantation faster.
2. Carefully expose the vessels and nerves, and tag their ends with fine Prolene suture
a. For fingers, use mid-axial longitudinal incisions
b. *A “corkscrew” appearance to the arteries suggests traumatic stretch from an avulsion. These will need excision of these damaged segments prior to replantation. It is an ominous sign, suggesting that vein grafting is necessary and the chance of success is worse.
c. Bruising of the neurovascular bundle also suggests avulsion or traction injury.
3. Preservation of “spare parts” may optimize outcome.
a. Heterotopic replants transfer tissue from one site to another, for example, thumb restoration with another amputated digit when the thumb is lost or unsalvageable.
b. Use of components from one amputated part for another part’s replant is economical, for example, digital nerves from another amputated (but unreplantable) finger.
4. When the amputation is more proximal, the part will contain muscle, which will swell after reperfusion. Therefore, any fascial compartments in the part must be released.
B. Operative overview
1. The recommended replant sequence is as follows
a. Prepare the stump; debride the wound
b. Identify arteries, veins, nerves, and tendons; place tagging sutures
c. Stabilize the bone(s)
d. Repair extensor tendons/muscles, then flexor tendons/muscles
e. Coapt nerves
f. Anastomose arteries
g. Anastomose veins
h. Cover wound with soft tissue/skin
2. In replanting multiple digits, a “part-by-part ” approach is usually preferred to “digit-by-digit” when all replantable parts are in equal condition
a. The sequence for these repairs is altered depending on circumstances and surgeon preference.
b. In patients with short ischemia times, some authors feel nerve repair can and should precede vascular repair.
c. In amputations involving a part with significant muscle, the risk of prolonged ischemia and subsequent reperfusion injury is high. Therefore, arteries should be repaired first, then nerves, and finally veins. This sequence provides in-flow to the amputated part and the “flushing out” of toxic metabolites while the nerves are being fixed, before the veins are anastomosed.
C. Stump preparation: Avulsion injuries involving tendons sometimes require fasciotomies/carpal tunnel releases, as swelling proximal to the level of the amputation will occur.
D. Bone fixation
1. Bone should be debrided. Shortening is beneficial in that it decreases tension on anastomoses and skin repairs.
2. Fixation can be achieved via various methods
a. Kirschner wires: Simple; very useful for fingers. Placed retrograde in amputated part first.
b. Interosseous wires: Used to augment K-wire repairs
c. Plate fixation: Not typically necessary for phalanges; useful for amputation at or proximal to the metacarpals
d. External fixation: May be useful for forearm replants
E. Tendon/muscle repair
1. Clean the tendon edges, but do not shorten excessively
2. Extensor tendons are repaired first, with two or three horizontal mattress sutures using 4-0 braided polyester
3. Next, repair flexor tendons with a core suture technique, such as a modified Kessler or Tajima repair (see Chapter 40 “Tendon Injuries and Tendonitis”).
F. Vessel anastomoses
1. Arterial repair
a. The artery must be trimmed back to healthy intima.
b. Vein grafts of the appropriate size may be found in the volar forearm, in the dorsal foot, or in “spare” amputated parts.
c. Papaverine and/or lidocaine are used to minimize vasospasm.
d. Repair of two arteries to a digit yields a higher successful replantation rate versus repair of a single artery, but one good anastomosis is adequate.
2. Venous repair
a. Two vein repairs per artery are preferred
b. Tension on venous repair must be minimal to prevent congestion
G. Nerve coaptation
1. Trim the nerves back to undamaged areas
2. Realign fascicles when possible to maximize the return of sensibility
H. Coverage
1. Skin is closed loosely over repaired vessels. A tight closure will restrict venous outflow.
2. Split thickness skin grafts are used as needed.
3. Nail removal to assess for bleeding and allow leech attachment if congestion occurs.
4. For more proximal replants, local or free muscle flaps are used to cover the operative site and protect the anastomoses.
5. A well-padded splint, with absolutely no circumferential pressure, should be made to protect the replant. Blood oozing often causes padding to become saturated, clotted and restrictive and must be monitored carefully.
V. POSTOPERATIVE CARE
A. Acute care
1. Aggressive hydration to keep vessels patent (usually a total fluid intake of one and a half maintenance for the first day or two, following urine output closely)
2. Avoid ANY vasoconstrictors for 1 month or more post-op, including caffeine and nicotine.
3. Analgesia is important to minimize catecholamine release. The patient should be resting comfortably.
4. Keep replanted extremity warm (warm room, blankets, Bair Hugger).
5. Medical therapies used to diminish complication rates.
a. Systemic heparinization should be used if in cases of wide vessel damage such as in crush amputations. Initiate therapy intraoperatively for the best result.
b. Dextran 40 infusion is used by many replant surgeons for its plasma expansion and anti-platelet effects. 500 cc is administered per day in adults (or 25 cc/h). A test dose of 5 cc is usually administered in the OR. While statistical proof of efficacy is lacking, side effects (anaphylaxis, acute renal failure, pulmonary edema) are rare.
c. Aspirin 81 or 325 mg QD is given for 3 weeks to retard platelet aggregation
d. Other agents are advocated by some authors, including chlorpromazine (Thorazine), dipyridamole (Persantine), and calcium channel blockers.
6. Objective monitoring of the replant can be done in a number of ways
a. Temperature probes (most reliable), keep >30°C
b. Pulse oximetry >94%
7. Frequent evaluation by the surgeon and staff for color and capillary refill (subjective monitoring) is essential and represents the best monitoring method
B. Failing replant
1. In the acute setting, the problem is usually vascular, either inflow or outflow
a. Arterial insufficiency: Cool, pale replant; no capillary refill; pin prick produces little or no bleeding
b. Venous insufficiency: Congested replant, increased tissue turgor, pin prick yields copious bleeding with dark blood
2. Initial treatment options include nonoperative measures
a. Elevate hand/arm
b. Loosen dressing; if needed, relax/release sutures
c. Add medical therapies (heparin, Thorazine, etc.)
d. Better pain control, that is, axillary block
e. Medicinal leeches
i. Can reduce venous congestion
ii. Secrete hirudin, a potent anticoagulant that remains localized
iii. Treatment lasts for up to 6 days
iv. *Patients should be placed on a third-generation cephalosporin or fluroquinolone to protect from Aeromonas hydrophila (gram negative rod) infection (ceftriaxone, ciprofloxacin)
f. Use of thrombolytics in replants is controversial.
3. Reexploration is the definitive treatment for vascular problems
a. Functional outcomes are poorer in patients requiring reoperation
b. Outcomes are best when re-operation is performed within 6 hours of loss of perfusion
VI. OUTCOMES
A. With good patient selection, replant failure rate is low, on the order of 20%. However, that number may be deceiving, as viable replants are not always valuable replants.
B. Mechanism of injury was the most important factor influencing survival rate of digit.
C. Late complications diminish the value of a replantation
1. ~50% loss of motion
a. Due to tendon adhesions and joint contracture
b. Most common secondary procedure is tenolysis (35% of all replants)
2. Decreased sensation is a function of injury mechanism, repair technique and level of injury.
3. Loss of motor function is a problem in more proximal amputations, where the slow axonal regeneration limits muscle re-innervation.
4. Chronic pain, including CRPS (chronic regional pain syndrome)
5. Cold intolerance: May improve somewhat for 2 years, but some residual intolerance very common
D. Functional outcome depends upon multiple factors
1. Sharp amputations always have better recovery of sensation and function than crush or avulsion amputations.
2. Children have better outcomes for a given level, but they are more problematic during rehabilitation due to noncompliance in very young children.
3. Thumb replants do best. Even if mobility is poor, the replant has value as a sensate post.
4. Zone I finger replants: Regain an average of 82 degrees of motion at the PIP joint (PIPJ)
5. Zone II finger replants: Regain an average of 35 degrees of motion at the PIPJ
6. Average two-point discrimination in a finger replant is 11 mm
PEARLS
1. Venous congestion of replantation can be treated by removing nailbed and placing heparin soaked pledgets or use of Leeches.
2. If using leeches, make sure to give prophylaxis against Aeromonas.
3. Leeches secrete Hirudin which is a thrombin inhibitor that is excreted by the kidneys.
4. Amputated piece should be placed in moist paper towel in bag and then on ice.
5. Make sure to consent patient for revision amputation, vein and nerve graft prior to replantation.
QUESTIONS YOU WILL BE ASKED
1. What is the difference between a cross finger flap (CFF) and a reverse CFF?
A CFF is for a volar defect using volar skin, whereas reverse CFF is for a dorsal defect using dorsal soft tissue.
2. What are indications, relative contraindication, and absolute contraindication to replantation?
Indications include thumb amputations, proximal amputations, multiple digits, and amputations in children. Relative contraindications include need to return to work quickly, medical comorbidities, age, and tobacco use. Absolute contraindications are life-threatening injuries or medical illness.
3. When considering replantation, what are the warm and cold ischemic times for fingers versus more proximal amputations?
Amputations with significant muscle mass (i.e., forearm) only have a 6-hour warm and a 12-hour cold ischemia tolerance. Digits have been replanted with as much as a 42-hour cold ischemia time in case reports.
4. How do vascular inflow obstruction and venous congestion present differently? What are the treatments for each?
Inflow obstruction presents with a cold, pale digit. It is treated with revision arterial anastomosis. Venous congestion presents with a swollen, purple digit that bleeds dark blood when poked. It can be treated with medicinal leeches or occasionally with a return to the OR.
Recommended Readings
Chang J and Jones N. Twelve Simple Maneuvers to Optimize Digital Replantation and Revascularization. Techniques in Hand and Upper Extremity Surgery. 2004;8(3):161–166.
Fassler PR. Fingertip injuries: evaluation and treatment. J Am Acad Orthop Surg. 1996;4(1):84–92. PMID: 10795040.
Yoshimura M. Indications and Limits of Digital Replantation. JMAJ. 2003;46(10): 460–467.
< div class='tao-gold-member'>