I. INCIDENCE
A. Benign tumors
1. Most tumors of the hand are benign (>90%)
a. Usually can be diagnosed clinically and requires no treatment
b. If lesion suddenly changes in size, appearance, or aggressiveness, appropriate workup (i.e., biopsy) must be done
2. Ganglion cysts are the most common benign tumor, comprising 50% to 70% of all hand tumors
3. Next most common are giant cell tumors of tendon sheath, epidermal inclusion cysts, lipomas, and foreign bodies
B. Malignant tumors
1. Squamous cell carcinoma is the most frequent primary malignancy of the hand
2. Other malignancies are far less common
a. Malignant metastases to the bones of the hand are exceedingly rare
b. A significant proportion of soft-tissue sarcomas and melanomas occur in the upper extremity
II. BENIGN SOFT-TISSUE TUMORS
A. Ganglion cysts
1. General
a. 50% to 70% of all hand tumors
b. 3:1 female predilection
c. Degenerative cysts commonest in older patients. Other ganglions commonest in second to fourth decade of life.
d. Most common benign tumor of the hand
i. Mucin-filled cyst attached to the tendon, tendon sheath, or joint capsule
ii. Most often occur in second to fourth decade of life, though they can occur in children and the aged
iii. Most often occur at the dorsal wrist, followed by volar wrist, flexor tendon sheath (volar retinacular), and distal interphalangeal (DIP) joint (mucous cyst)
a) These four sites make up more than 90% of the ganglions of the hand
b) Can also see ganglions in association with carpometacarpal bossing, at the proximal interphalangeal joint
iv. Transilluminate
2. Dorsal wrist ganglion
a. Epidemiology—60% to 70% of all hand and wrist ganglions
b. Anatomy: *Usually over the scapholunate (SL) junction between the third and fourth extensor compartments. Approximately 75% connect by the stalk with the SL joint ligament.
c. Presentation: Compressible, transilluminating, mobile, limited wrist dorsiflexion, aching discomfort
d. Diagnosis/workup: Clinical exam, ± diagnostic ultrasound (US) if unsure, magnetic resonance imaging (MRI) if diagnosis remains elusive
______________
*Denotes common in-service examination topics
i. Observation: If not symptomatic or impairing
ii. Supportive splinting/nonsteroidal anti-inflammatory drugs (NSAIDs)
iii. Puncture and aspiration: High potential for recurrence
iv. Surgical excision: Indicated for pain, impairment, and failure of conservative treatment. Usually done in operating room under loupe magnification, with a transverse incision; dissect down to stalk and coagulate base.
f. Outcomes: Recurrence is very low if small cuff of normal tissue is taken with the cyst and stalk
g. Complications
i. Injury to radial sensory branches
ii. Wrist stiffness
3. Volar wrist ganglion
a. Epidemiology: 10% to 20% of the hand and wrist ganglions
b. Anatomy: Between the first extensor compartment and the flexor carpi radialis tendon sheath. About 60% arise from the radioscaphoid joint and 30% from the scaphotrapezial joint.
c. Presentation: Characteristics similar to dorsal ganglions. Discomfort when mass is “bumped.” Nonpulsatile. Possible median or ulnar nerve palsies with mass effect.
d. Diagnosis/workup: Clinical exam. Requires imaging and additional workup if history of penetrating injury to volar forearm (check for bruits, Doppler US to rule out pseudoaneurysm), or symptoms of nerve palsy (US or MRI: extent of mass).
e. Treatment
i. Observation: If asymptomatic
ii. Supportive splinting/NSAIDs
iii. Surgical excision: Similar indications as dorsal ganglion
f. Outcomes: Similar to dorsal ganglions
g. Complications
i. Nerve injuries: Palmar cutaneous median branch and lateral antebrachial cutaneous nerve
ii. Wrist stiffness
4. Volar retinacular ganglion cyst
a. Epidemiology: 5% to 10% of hand and wrist ganglions
b. Anatomy: Arise from digital flexor sheath at A1 or A2 pulley, near proximal digital flexor crease or metacarpophalangeal (MCP) joint. No movement with flexor excursion. Propensity for middle finger.
c. Presentation: Firm immobile “pea-like” firm mass. Diminished sensation if it impinges on digital neurovascular bundle. Discomfort with forceful grip. May present with stenosing flexor tenosynovitis (trigger finger).
d. Diagnosis/workup: Clinical exam
e. Treatment
i. Observation: If asymptomatic
ii. Aspiration: Can be curative. Risk of injury to digital neurovascular bundle.
iii. Injection: Can be curative; 1% lidocaine and methylprednisone into the cyst to rupture it
iv. Surgical excision: If patient preference or conservative measures fail
f. Outcomes: Recurrence is rare
g. Complications: Digital neurovascular bundle injury
5. Degenerative mucous cysts
a. Epidemiology: Predilection for middle aged and elderly
b. Anatomy: Over dorsal DIP joint. Propensity for index and long fingers. *Nail deformity common (pressure on the germinal matrix).
c. Presentation: Firm, minimally mobile, transilluminating, thinned skin over lesion. Pain from osteoarthritis of DIP joint. Drainage of cystic fluid if thinned skin ruptures. Soft-tissue infection and septic arthritis possible with ruptured cyst.
d. Diagnosis/workup: Clinical exam. Radiographs for degenerative changes of osteoarthritis.
i. Observation: If asymptomatic and no perceived risk of rupture
ii. Aspiration: Potential for recurrence, need for multiple treatments, risk of infection, and septic arthritis
iii. Surgical excision: Highest success rate with low complications risk. If the skin is very thin, excised, with osteophyte when present, and closed with rotation-advancement flap of dorsal skin.
f. Outcomes
i. Recurrence uncommon
ii. Nail deformity may resolve after excision
g. Complications
i. DIP joint extensor lag
ii. DIP joint stiffness
iii. Residual pain
iv. Infection including septic arthritis
v. Nail plate deformity
vi. DIP joint radial or ulna deviation
h. Adjunctive procedures: DIP joint arthrodesis if debilitating pain from osteoarthritis
B. Giant cell tumors
1. Also known as localized nodular synovitis, fibrous xanthoma, and pigmented villonodular tenosynovitis
2. Epidemiology
a. Second most common soft-tissue tumor in the hand
b. Fourth to sixth decade of life
c. Slight predilection for women
3. Anatomy
a. Multilobular, well circumscribed
b. Propensity for DIP joint region
c. May displace or envelope neurovascular bundle
d. Can be locally aggressive and involve bone
4. Presentation
a. Firm painless mass in the hand or wrist
b. Propensity for the thumb, index, and long fingers
c. Slow growing and present for several months to years
d. Do not transilluminate
e. Neuropathic symptoms with digital neurovascular bundle involvement
5. Diagnosis/workup: Clinical exam
6. Treatment: Marginal excision
7. Outcomes: Recurrence ranges from 5% to 50%
8. Complications
a. Recurrence
b. Neurovascular bundle injury
C. Epidermal inclusion cysts
1. Epidemiology
a. Often from trauma: Epithelial cells introduced into subcutaneous tissue or bone
b. Third commonest tumor of the hand
c. Common after traumatic digital amputation
d. Unapparent for months to years following inciting event
e. Predilection for men
2. Anatomy
a. Propensity for the finger tip
b. Usually just beneath the skin
c. Finger tip cysts may erode into the bone causing lytic lesion in distal phalanx
3. Presentation
a. Firm, well circumscribed, and slightly mobile
b. Slow growing and present for months to years
c. Do not transilluminate
4. Diagnosis/workup: Clinical exam
5. Treatment: Excision
6. Outcomes: Recurrence is rare
7. Complications: Rare
III. MALIGNANT SOFT-TISSUE TUMORS
A. General
1. Rapid enlargement, aching (especially at night), >5 cm: Malignant until proven otherwise
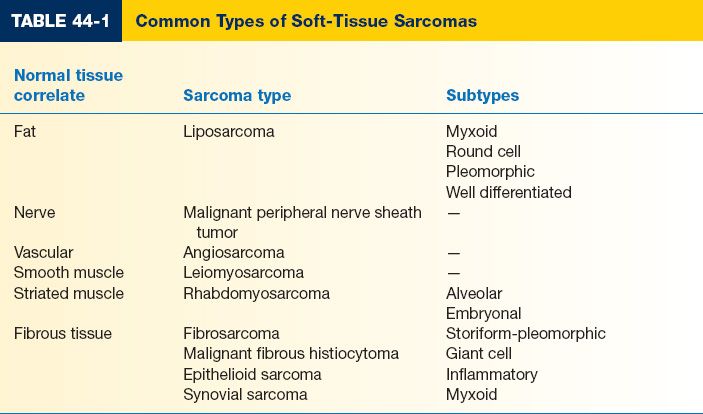
2. The most common soft-tissue sarcomas of the hand/upper extremity are malignant fibrous histiocytoma, synovial sarcoma, epitheliod sarcoma, and liposarcoma
3. Diagnosis via incisional or excisional biopsy; not fine-needle aspiration
4. Most commonly metastasize to the lungs except for epithelioid sarcoma, which usually goes to the lymph nodes
5. Treatment usually involves wide local excision (with 2- to 3-cm margin) and XRT with high grade lesions; chemo is controversial; amputation if 2- to 3-cm margin not possible
B. Epithelioid and synovial cell sarcoma
1. Epidemiology
a. Only 3% of sarcomas present in the hand, the two most common sarcomas in hand being epithelioid and synovial cell (Table 44-1)
b. First to third decade with male preponderance
2. Anatomy
a. Epithelioid: Volar digits and palm
b. Synovial: Adjacent to carpus. Rare in digits. Arise in tendon sheaths and bursa.
3. Presentation
a. Epithelioid: Firm or ulcerating nodule. Usually mistaken for infection.
b. Synovial: Slow-growing painless mass. May be present for years.
4. Diagnosis/workup
a. MRI to evaluate anatomy
b. Incisional biopsy if possible, arranged longitudinally
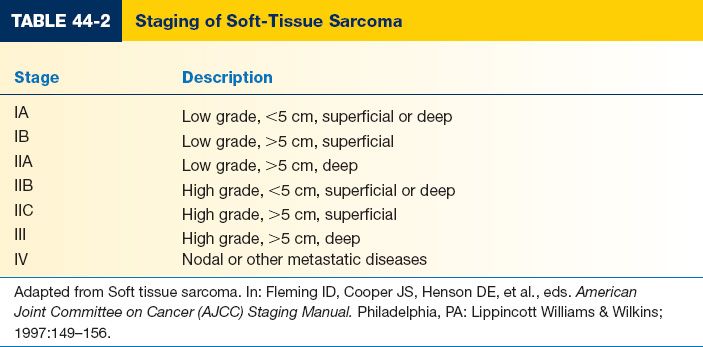
c. Staging and multidisciplinary discussion is critical (Table 44-2)
5. Treatment options
a. Neoadjuvant radiation: Depending on stage. When adjacent to vital structures.
b. *Epithelioid: Limb-sparing wide or radical excision with sentinel node biopsy and adjuvant radiation. Some indications for adjuvant chemotherapy (depends on the size, grade, nodal, and metastatic status).
c. Synovial: Limb-sparing wide or radical excision with adjuvant radiation and chemotherapy
d. Amputation if wide excision is not possible
6. Outcomes
a. Worse prognosis with hand sarcomas
b. Five-year survival significantly poorer than nonhand sarcomas
7. Complications
a. Recurrence
b. Impaired wound healing, usually due to XRT
8. Follow-up/surveillance
a. Local: MRI.
b. Systemic: Chest and abdominal computed tomography (CT). Every 4 months (3 years), then every 6 months (2 years), then annually
C. Kaposi’s sarcoma
1. Malignant vascular tumor
2. Occurs in the hand, but is more common in lower extremities
3. Whenever patient presents with bluish-red skin nodules, must consider diagnosis of AIDS (acquired immunodeficiency syndrome)
4. Highly radiosensitive tumor, though residual disease usually remains even after aggressive XRT
IV. BENIGN BONE AND CARTILAGE TUMORS
A. Enchondroma
1. Epidemiology
a. *Solitary enchondroma: Most common bone tumor of the hand. About 54% of all enchondromas. Approximately 90% of all hand bone tumors.
b. Multiple enchondromas: Ollier disease (enchondromatosis) and Maffucci syndrome (enchondromatosis and multiple hemangiomas)
c. Second to third decade of life. Patients with enchondromatosis present earlier.
d. Malignant transformation (chondrosarcoma): Rare except in enchondromatosis
2. Anatomy
a. Proximal phalanges > metacarpals > middle phalanges
b. Intramedullary
a. Asymptomatic with local edema
b. *Sudden onset of pain, swelling, and edema = Pathologic fracture
c. Rapid growth: Concern for malignant degeneration
4. Diagnosis/workup: Plain radiographs
5. Treatment
a. Observation: Acceptable for small asymptomatic tumors with no concerns for malignancy (discuss the potential for fracture)
b. Surgical treatment
c. *If the patient presents with a pathologic fracture, first heal the fracture (with immobilization or pins as needed) and then resect the lesion.
6. Surgical treatment
a. Curettage of lesion
b. Extend margins with burr if possible. May cauterize cavity with phenol.
c. Cancellous bone grafting of lesion
7. Outcomes
a. Recurrence after curettage ranges from 2% to 15%
b. If recurrent: Rule out malignancy
8. Complications
a. Infection
b. Fracture
c. Recurrence
9. Follow-up/surveillance
a. After curettage and grafting: Radiographs and clinical exam at 6 months, 1 year, and 2 years
b. For observed patients: Annual radiographic surveillance (at least 2 years)
B. Giant cell tumor (GCT) of the bone
1. Epidemiology
a. Uncommon in the hand
b. >20 years of age. Predilection for women.
c. Benign but locally aggressive; can metastasize (propensity for the chest). Metastasis can be fatal.
d. Hand and wrist tumors: Higher rates of local recurrence and metastasis
2. Anatomy: Wrist (distal radius): Third most affected site. In the hand, usually in carpus.
3. Presentation: Pain and swelling. May present with pathologic fracture.
4. Diagnosis/workup
a. Plain radiographs: Lytic with cortical expansion and indistinct borders. MRI for treatment planning.
b. Chest X-ray or CT and bone scan: Metastasis/multifocal disease
c. Staging for GCT of bone (radiographs)—stage I: no distortion or perforation of cortex; stage II: distortion or expansion of the cortex without soft-tissue involvement; stage III: perforation of the cortex with extension into soft tissues.
d. Incisional biopsy
5. Treatment
a. Wrist. Stage I and II: Curettage with adjuvant treatments (phenol, high-speed endosteal burring, and liquid nitrogen). Cavity packed with bone graft, methyl methacrylate.
b. Wrist. Stage III: Wide en bloc excision with reconstruction. Proximal row carpectomy if intra-articular contamination present. Intercalary wrist arthrodesis with bone graft.
c. Metacarpals/phalanges: Stage I and II treatments similar to the wrist. Stage III: Amputation versus wide en bloc excision with reconstruction.
a. Higher recurrence in hand/wrist tumors (up to 50% with curettage and adjuvant treatments)
b. 25% risk of metastasis from distal radius and 10% risk of metastasis with hand tumors
7. Complications
a. Stiffness
b. Infection
c. Joint collapse
d. Impaired range of motion
e. Neurapraxia
f. Recurrence
8. Follow-up: For local and systemic disease. Chest X-ray at regular intervals (optimal interval unknown). CT chest for patients presenting with recurrence.
C. Aneurysmal bone cyst
1. Epidemiology
a. Uncommon in the hand, 5% of cases
b. 75% in patients <20 years. No gender predilection.
c. Locally aggressive and destructive. No metastatic potential.
2. Anatomy: Usually in metacarpals and proximal phalanges
3. Presentation
a. Slowly enlarging firm mass with or without pain
b. Significant edema and warmth may be present
c. May present with pathologic fracture
4. Diagnosis/workup: Plain radiographs. MRI or CT scan may narrow differential diagnoses.
5. Treatment
a. Treatment is curettage and bone grafting, may need several tx
b. Adjuvant treatments: Liquid nitrogen, high-speed burring, and cementation also used
c. En bloc excision for aggressive tumors with no good bone stock
d. Amputation for destructive distal phalanx tumors
6. Outcomes: Up to 60% recurrence with curettage and no adjuvant treatment. Adjuvant treatments improve outcomes (come with complications).
7. Complications
a. Fracture (high-speed burring and liquid nitrogen)
b. Premature physeal closure (liquid nitrogen)
c. Joint collapse (liquid nitrogen)
d. Infection (liquid nitrogen)
e. Recurrence
D. Osteoid osteoma/osteoblastoma
1. Epidemiology
a. 10% of all benign bone tumors; 5% to 15% of all osteoid osteomas are in the hand/wrist
b. Second to third decade of life
c. 2:1 male predilection
2. Anatomy
a. Predilection for carpus (scaphoid and capitate) and proximal phalanges
b. Propensity to be juxta-articular
3. Presentation
a. Significant focal dull ache, worse at night. Relief with NSAIDs.
b. Soft-tissue edema and limited motion at nearest joints
a. *Radiographs, small round lucency (the nidus), situated within the cortex, surrounded by sclerotic, reactive bone
b. Thin-cut CT and bone scan have higher sensitivity than plain radiographs
5. Treatment
a. Symptomatic treatment with NSAIDs
b. Surgical treatment: Curettage and grafting
6. Outcomes: Recurrence ranges from 0% to 25%
7. Complications
a. Fracture
b. Recurrence
V. MALIGNANT BONE AND CARTILAGE TUMORS
A. Chondrosarcoma
1. Epidemiology
a. *Most common primary malignant bone tumor of the hand
b. Most likely malignant degeneration of preexisting lesion (enchondroma, osteochondroma, and fibrous dysplasia)
c. Fourth to sixth decade of life
2. Anatomy: Occurrence in proximal phalanx > metacarpals. Rare in carpus.
3. Presentation
a. Slowly enlarging firm mass, often painful
b. Symptoms could be present >10 years
4. Diagnosis/workup
a. Radiographs (cortical expansion and destruction, endosteal erosion, mineralization, and pathologic fracture) and histopathology (incisional biopsy): Correlate to improve sensitivity
b. Staging chest CT
5. Treatment: Wide en bloc resection: Limb-sparing or amputation/ray resection and reconstruction
6. Outcomes
a. Approximately 10% risk of metastasis, usually to the lung
b. Good local control with amputation and ray resection
7. Complications
a. Infection
b. Recurrence
8. Follow-up/surveillance: Monitor for local recurrence with MRI and pulmonary metastasis with CT scan
B. Osteosarcoma
1. Epidemiology
a. <1% of all osteosarcomas are in the hand
b. Fourth to seventh decade of life. No gender predilection.
c. Usually arise de novo from the bone. May be secondary to Paget’s disease and ionizing radiation.
d. Metastasis from hand tumors less common than tumors elsewhere
2. Anatomy
a. Metacarpals and phalanges. Carpal tumors rare.
b. Propensity for metaphysis
3. Presentation
a. Palpable soft tissue mass with localized tenderness
b. Pain and swelling
c. May present with pathologic fracture
d. Average duration before presentation is 3 months
4. Diagnosis/workup
a. Plain films of the entire bone involved, bone scan, plain films, and CT scan of the chest for staging
b. Classic radiographic appearance: Radial ossification (“sun burst” pattern), periosteal elevation with Codman triangles
c. MRI of involved hand for surgical planning
d. Incisional biopsy
5. Treatment
a. Neoadjuvant chemotherapy versus adjuvant chemotherapy
b. Limb sparing wide en bloc excision and reconstruction or amputation
c. Radiation after induction chemotherapy for patients who decline surgery
6. Outcomes
a. Overall 5-year survival is 70%. About 10% to 20% in patients that present with metastasis.
b. Up to 80% to 85% 5-year survival if >90% tumor necrosis with preoperative induction chemotherapy
c. Success of radiation dependent on induction chemotherapy response
7. Complications
a. Wound healing difficulties
b. Recurrence
C. Ewing’s sarcoma
1. Epidemiology
a. 10% of all primary malignant bone tumors. Rare in the hand.
b. 80% in patients <20 years. Male preponderance.
2. Anatomy: Metacarpals and proximal phalanges
3. Presentation
a. Swelling, pain, and erythema; may present with fever; can resemble infection
b. May show leukocytosis and elevated sedimentation rate (nonspecific)
4. Diagnosis/workup
a. May be mistaken for an infection
b. MRI for diagnosis, local staging, surgical planning
c. Incisional biopsy
d. Chest X-ray and CT, bone scan, bone marrow aspirate for oncologic workup
5. Treatment options
a. Neoadjuvant chemotherapy to decrease tumor size
b. Wide en bloc resection and reconstruction
c. Radiation: If poor response to chemotherapy, surgical margins are inadequate, surgical treatment is not feasible
6. Outcomes: Up to 70% 5-year survival with adjuvant chemotherapy
7. Complications: Recurrence
VI. GENERAL MANAGEMENT PRINCIPLES OF PATIENTS WITH UPPER EXTREMITY TUMORS
A. Patient workup
1. Radiographs of the extremity
2. MRI or CT of the primary lesion
3. Chest X-ray, liver function tests, complete blood count
4. Bone scan to assess for metastatic disease
5. Examine epitrochlear (around the medical epicondyle), axillary lymph nodes, and deltopectoral area along the cephalic vein
B. Biopsy considerations
1. Incisional (usually when >3 cm) versus excisional biopsy
2. Do not exsanguinate the extremity, but may use a tourniquet (no Bier blocks)
3. Longitudinal incisions: Can subsequently be incorporated into a limb salvage procedure or completely excised during an amputation (do not use transverse, zig-zag, or Brunner-type incisions)
4. Limit skin flaps to minimize potential soft-tissue contamination
5. Notify surgical pathologist in advance; discuss differential diagnosis and handling of specimen; use frozen sections to determine if specimen is adequate (not to determine diagnosis)
6. Culture every specimen for bacteria, tuberculosis, and fungus
C. Types of surgical margins
1. Intracapsular or intralesional (piecemeal): Leave gross tumor behind
2. Marginal (shell out the tumor): Leave microscopic satellite lesions
3. Wide (intra-compartmental): Lesion removed with normal adjacent tissue
4. Radical (extra-compartmental): Removes entire compartment of involved and noninvolved tissues
D. Surgical management of a malignant tumor
1. Function is secondary to eradication of tumor
2. Need a complete workup prior to final resection
3. Know the sensitivity of the tumor to XRT and chemotherapy
4. Site-specific management
a. Distal phalanx
i. Usually amputate through the DIP joint or distal middle phalanx
ii. Usually ray amputation not necessary
b. Middle/proximal phalanx: Ray amputation often provides better function and aesthetics than MCP disarticulation
c. Thumb metacarpal
i. If confined to bone, excise and bone graft
ii. If soft tissues involved, perform a ray resection
iii. To resect second metacarpal to obtain a clear margin, consider index pollicization
d. Metacarpals 2 to 5: May require resection of surrounding rays
e. Wrist/distal forearm
i. Should not be treated with local excision
ii. Leaving nerve or tendon for function could result in a high rate of recurrence
PEARLS
1. Seemingly benign lesions can simply undergo excision for treatment and diagnosis
2. Seemingly malignant lesions require further imaging—usually MRI—and tissue diagnosis with an incisional or core biopsy
3. Always design biopsies or excisions longitudinally in the extremities. It allows positive margins to be more easily excised while sacrificing less normal tissue.
4. Glomus tumors: Usually subungual. Presentation: Intermittent extreme pain, cold sensitivity (Love sign), tender to palpation. Diagnosis: MRI. Treatment: Excision.
5. Neurilemmoma: Usually in volar forearm. Presentation: Painless nonadherent mass, Tinel’s sign present over mass, no neurologic deficit. Diagnosis: MRI. Treatment: Nerve-sparing excision.
6. Greater than 90% of all hand tumors are benign
QUESTIONS YOU WILL BE ASKED
1. What is the most common benign tumor?
Ganglion cyst.
2. What is the most frequent primary malignancy of the hand?
Squamous cell carcinoma.
3. What is classic triad associated with glomus tumor?
Severe pain, cold sensitivity, and tenderness.
4. What is the most common primary bone tumor of the hand?
Enchondroma.
5. What tumor presents with nocturnal pain that is typically relieved by aspirin or NSAIDs?
Osteoid osteoma.
Recommended Readings
Athanasian EA. Aneurysmal bone cyst and giant cell tumor of bone of the hand and distal radius. Hand Clin. 2004;20(3):269–281, vi. PMID: 15275686.
Nahra ME, Bucchieri JS. Ganglion cysts and other tumor related conditions of the hand and wrist. Hand Clin. 2004;20(3):249–260. PMID: 15275684.
O’Connor MI, Bancroft LW. Benign and malignant cartilage tumors of the hand. Hand Clin. 2004;20(3):317–23, vi. PMID: 15275690.
Plate AM, Lee SJ, Steiner G, Posner MA. Tumorlike lesions and benign tumors of the hand and wrist. J Am Acad Orthop Surg. 2003;11(2):129–141. PMID: 12670139.
Plate AM, Steiner G, Posner MA. Malignant tumors of the hand and wrist. J Am Acad Orthop Surg. 2006;14(12):680–692. PMID: 17077340.
< div class='tao-gold-member'>