ELECTRICAL INJURY
I. BACKGROUND
A. Electrical injuries represent less than 5% of burn injuries admitted to major burn centers.
B. The typical patient is a young male. The injury is often work-related.
C. Total body surface area (TBSA) is not necessarily associated with prognosis and does not quantify damage to deep tissues
II. MECHANISM OF INJURY
A. Thermal: Can generate temperatures over 100 degrees
B. Electroporation: Electrical force drives water into lipid membrane and causes cell rupture
C. Assessment of entry and exit wounds not always useful
D. Difficult to determine type and severity of damage between entrance and exit
E. Tissue resistance in decreasing order = bone, fat, tendon, skin, muscle, vessel, nerve. (Bone heats to a high temperature and burns surrounding structures.)
III. INJURY SEVERITY
A. Determined by voltage, current type, and resistance
B. High voltage burns are considered to be those involving >1000 volts
C. Alternating current causes tetanic muscle contraction and the “no-let-go” phenomenon. This occurs due to simultaneous contraction of (stronger) forearm flexors and (weaker) forearm extensors.
D. Ohm’s law: Current = Voltage/Resistance
IV. ETIOLOGY
A. All must be considered prior to determination of a management plan.
B. Current flow through tissue can cause burns at entrance/exit wounds and burns to deep tissue.
1. Current will preferentially travel along low-resistance pathways.
2. Nerves and blood vessels have low resistance. Bone has high resistance.
3. Current will pass through soft tissue, contact high-resistance bone, and travel along bone until it exits to the ground
C. Vascular injury to nutrient arteries
1. Damage to intima and media
2. Thrombosis
D. Cardiac effects
1. Arrhythmia—EKG monitor for at least 24 hours
2. Coronary artery spasm
3. Myocardial injury and infarction
E. Gastrointestinal (GI) effects
1. Injury to solid organs
2. Acute bowel perforation
3. Delayed bowel perforation
4. Gallstones after myoglobinuria
______________
*Denotes common in-service examination topics
F. Electrical arcs have incredibly high temperatures and can cause flash burns.
G. Electricity can ignite clothing or structures with secondary flame burns.
V. INITIAL MONITORING
A. Airway maintenance: C-collar until c-spine cleared
B. Breathing and ventilation—100% oxygen
C. Circulation and cardiac status
1. Cardiac monitor
2. Two large-bore IV catheters
3. Assess peripheral perfusion
4. ECG
5. 24-hour monitor if
a. Ectopy or dysrhythmia present
b. Loss of consciousness
c. Cardiac arrest
d. Abnormal rate or rhythm
D. Disability, neurological deficit, and gross deformity
1. Assess level of consciousness
2. Note any neurological deficit
3. Note any gross deformity
E. Exposure and environmental control
1. Stop the burning process and remove clothes
2. Avoid hypothermia
F. Renal function analysis and urine myoglobin
VI. FLUID RESUSCITATION
A. TBSA provides an inadequate estimation of burn severity
B. Unlike thermal injury, electrical injury often occurs deep to the skin and is not visible. Thus, standard fluid resuscitation models (Parkland formula) may underestimate fluid resuscitation needs.
C. The Parkland formula can be used to provide a minimum volume estimate. If no urine pigmentation is present, the minimum acceptable urine output is 0.5 mL/kg/h.
D. Pigmented urine can be caused from myoglobin (secondary to rhabdomyolysis) and/or free hemoglobin (from damaged RBCs)
1. For myoglobinuria, the urine dipstick will be positive for blood. However, microscopy will not demonstrate RBCs.
2. *The goal urine output for rhabdomyolysis and myoglobinuria is 2 mL/kg/h or about 75 to 100 cc/h.
a. Insufficient volume resuscitation can predispose to myoglobin-induced acute tubular necrosis.
b. In addition to adequate fluid resuscitation, myoglobin excretion can be promoted using mannitol (12.5 g/h osmotic diuresis) and/or urine alkalinization with 50 mEq/L of bicarbonate.
c. Follow urine myoglobin levels every 6 hours until a downward trend is seen.
VII. COMPARTMENT SYNDROME CAN OCCUR AFTER HIGH-VOLTAGE INJURY TO AN EXTREMITY
A. Current travels along bone, which has high resistance.
B. The bone serves as a conductor and “cooks” adjacent tissue from deep to superficial.
C. *In the upper extremity, flexor digitorum profundus and flexor pollicis longus will be most severely affected (closest to bone)
D. Over-aggressive fluid resuscitation can worsen tissue edema, resulting in increased tissue pressures, and exacerbating raised compartment pressures typically occurs within 48 hours of injury
E. Compartment syndrome
1. Clinical concern for raised compartment pressures mandates an evaluation of compartment pressures or a trip to the operating room
2. The 6 “P” signs/symptoms include pain out of proportion, paresthesia, pallor, paralysis, pulselessness, and poikilothermia
3. Raised compartment pressures can be used as an adjunct to clinical diagnosis, or when the patient is unable to participate in clinical examination
a. *Absolute pressure ≥30 mmHg
b. Pressure within 20 mmHg of the diastolic blood pressure is also diagnostic of compartment syndrome.
4. Compartment pressures can be measured using a Stryker intra-compartmental pressure monitor or an arterial line pressure transducer.
F. Upper extremity compartment syndrome is managed with surgical release of the volar and extensor compartments, the mobile wad, carpal tunnel, Guyon’s canal, and nine compartments of the hand
G. Lower extremity compartment syndrome managed with fasciotomies of the anterior, lateral, superficial posterior, and deep posterior compartments
CHEMICAL BURNS
I. GENERAL APPROACH TO CHEMICAL BURN TREATMENT
A. Protect yourself with personal protective equipment: always consider that the chemicals are still present and must be neutralized or temporized
B. Clothing that is saturated with chemical should be removed. Any powders that are present on the skin should be brushed off.
C. With few exceptions (see below), all chemical burns should be copiously irrigated with water. This dilutes but does not neutralize the chemical and cools the burning area.
D. Neutralization of a chemical burn is generally contraindicated because neutralization may generate heat and cause further burn injury
E. Water irrigation is contraindicated or ineffective in several scenarios
1. Contraindicated with elemental sodium, potassium, and lithium as this will precipitate an explosion.
2. Dry lime should be brushed off, not irrigated
3. Phenol is water insoluble and should be wiped from the skin with polyethylene glycol-soaked sponges.
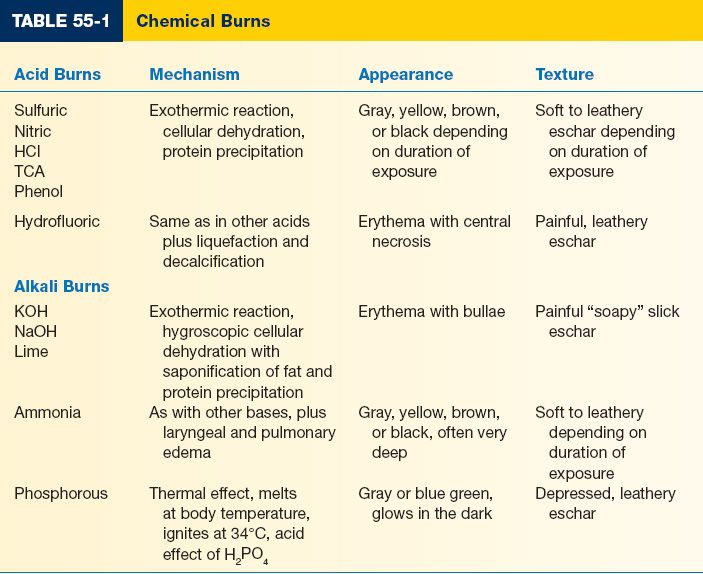
II. TYPES OF CHEMICAL BURNS (TABLE 55-1)
A. Alkali-mechanism of injury is via liquefaction necrosis and protein denaturation
1. Oven, toilet and drain cleaners, fertilizer, wet cement
2. Alkali injury will extend deeper into tissues until the source is removed or diluted
B. Acids damage tissue via coagulation necrosis and protein precipitation
1. Acid injury is typically self-limited and confined to the region of exposure.
2. Acids are commonly found in household cleaners and rust removers.
C. Organic compounds cause damage via multiple mechanisms
1. Phenol and petroleum
2. Cutaneous damage due to fat solvent action (cell membrane solvent action)
3. Systematic absorption with toxic effects on the liver and kidneys
D. When in doubt about the type of burn, check the label on the can or bottle. Your local poison control office may be a helpful resource.
III. SPECIFIC TYPES OF CHEMICAL BURNS
A. Hydrofloric acid (HF) is a potent and corrosive acid commonly used as a rust remover, in glass etching, and to clean semiconductors
1. HF is a weak acid but the fluoride ion is toxic.
2. HF can cause severe pain and local necrosis.
3. Acid exposure is treated with copious water irrigation.
4. *Fluoride ion can be neutralized with topical calcium gel (1 amp calcium gluconate in 100 g lubricating jelly)
5. If symptoms persist, can consider intra-arterial calcium infusion (10 mL calcium gluconate diluted in 80 mL of saline, infused over 4 hours) and/or subeschar injection of dilute (10%) calcium gluconate solution.
6. *Fluoride ion can bind free serum calcium. Make sure to check the serum calcium and replace with IV calcium as needed.
B. Phenol is commonly used in disinfectants and chemical solvents
1. Phenol is an acidic alcohol with poor water solubility.
2. Phenol causes protein disruption and denaturation that result in coagulation necrosis.
3. Phenol is associated with cardiac arrhythmia and liver toxicity: Cardiac and liver function should be monitored
4. Phenol is cleared by the kidneys
5. Phenol causes demyelination and has a local anesthetic effect. Thus, pain is not a reliable indicator of injury.
6. *Treatment of phenol exposure includes copious water irrigation and cleansing with 30% polyethylene glycol or ethyl alcohol
7. EKG is required.
C. Tar is used in the paving and roofing industry as a durable, waterproof coating
1. Tar can be heated to 260°C (∼500°F) prior to application. In addition to thermal injury, tar solidifies as it cools and will become enmeshed with hair and skin.
2. Tar should be cooled with copious water irrigation to stop the burning process.
3. Tar removers promote micelle formation to break the tar–skin bond.
a. A sterile surfactant mixture (De-Solv-it or Shur-Clens) allows tar to be wiped away in real time.
b. Wet dressings using polysorbate (Tween 80) or Neomycin cream for 6 hours prior to tar removal can also be effective.
D. White phosphorus is used in the manufacture of military explosives, fireworks, and methamphetamine
1. White phosphorous explosions will deposit chemical particles on the skin.
2. These particles will smoke when exposed to air
3. Obvious particles should be brushed off. The skin should be irrigated with a 1% to 3% copper sulfate solution.
4. Copper sulfate stains the particles black for identification
5. Copper sulfate will also prevent ignition when particles are submerged in water
6. After copper sulfate irrigation, the exposed area should be placed in a water bath and the white phosphorous should be removed.
E. Anhydrous ammonia is an alkali used in fertilizer
1. Skin exposure is treated with irrigation and local wound care
2. Anhydrous ammonia exposure is associated with rapid airway edema, pulmonary edema, and pneumonia: Consider early intubation for airway protection
F. Methamphetamine
1. Tachycardia (greater than expected with a similar size burn)
2. Hyperthermia
3. Agitated
4. Paranoid
IV. INJURY TO EYES
A. Prolonged irrigation with Morgan lenses
B. Eyelids may need to be forced open due to edema or spasm
C. Utilize topical ophthalmic analgesic
D. Consult an ophthalmologist
E. Electrical injuries can cause late cataracts therefore good to get a baseline.
F. Can cause increase in intra-ocular pressures.
G. Can get corneal abrasions if corneas not protected and/or lubricated.
PEARLS
1. Electrical injury can cause harm via multiple mechanisms, including cutaneous burns from arc or clothing fire, deep tissue burns from current flow along bones, concomitant traumatic injury, and cardiac arrhythmia
2. Rhabdomyolysis is treated with aggressive fluid resuscitation to maintain urine outputs ∼100 cc/h
3. Compartment syndrome is treated with decompressive fasciotomy
4. Acids, alkalis, and organic compounds can all cause chemical burns
5. Alkalis cause liquefaction necrosis and will continue to burn until diluted
QUESTIONS YOU WILL BE ASKED
1. How is compartment syndrome diagnosed and treated?
a. Compartment syndrome is a clinical diagnosis, typically made using the 6 “P’s” (see above). Measurement of intra-compartmental pressures is a useful adjunct when clinical diagnosis is unclear or the patient is unresponsive. Compartment syndrome requires compartment release of the affected areas, typically the forearm and/or hand.
b. *Diagnosis: Absolute pressure ≥30 mmHg or pressure within 20 mmHg of the diastolic blood pressure is also diagnostic of compartment syndrome.
2. How can kidney damage associated with rhabdomyolysis be minimized?
The goal urine output for patients with rhabdomyolysis is 2 mL/kg/h. Excretion of myoglobin can also be encouraged using mannitol (osmotic diuresis) and/or urine alkalinization with 50 mEq/L of bicarbonate. Serum myoglobin levels can be followed.
3. Which is worse: acid burns or alkali burns?
Alkali. Alkali burns will continue to extend deeper into tissues until the source is removed or diluted. Acid injury is typically limited to the exposed area.
4. How are hydrofluoric acid burns managed?
Acid burns should be copiously irrigated with water for dilution. If pain persists, the fluoride ion can be neutralized with topical calcium gel. Additional interventions include intra-arterial calcium infusion or sub-eschar injection of dilute calcium gluconate solution.
Recommended Readings
Arnoldo B, Klein M, Gibran NS. Practice guidelines for the management of electrical injuries. J Burn Care Res. 2006;27(4):439–447. PMID: 16819345.
Palao R, Monge I, Ruiz M, Barret JP. Chemical burns: pathophysiology and treatment. Burns. 2010;36(3):295–304. PMID: 19864073.
< div class='tao-gold-member'>