Thumb Reconstruction
Wee-Leon Lam
Fu-Chan Wei
INTRODUCTION
A functional thumb is critical to overall hand prehension. Efforts to reconstruct the thumb have spanned the history of hand surgery, and thumb reconstruction was one of the first microsurgical free tissue transfers to be attempted in humans.1 A functional thumb must meet the minimum requirements for pulp-to-pulp or tripod pinch to enable fine object manipulation and also hand-digital cylinder grasp for larger objects. Successful thumb reconstruction must therefore result in a construct that has (1) sufficient length to oppose the remaining fingers; (2) mobility of all joints involved in opposition and flexion; (3) adequate sensation for pulp pinch; and finally (4) an acceptable aesthetic appearance.2 Thumb amputation represents one of the few indications where every effort is made for replantation. When replantations fail for whatever reasons, numerous techniques have been described to replace the amputated thumb ranging from simple osteoplastic techniques to complex microsurgical procedures. With increased experience, toe-to-thumb transplantation has become the superior method of reconstruction to achieve all the functional and aesthetic requirements of a thumb in a single-stage procedure. This chapter details the different techniques and their indications and limitations for the wide variety of thumb injuries encountered in clinical practice.
ASSESSMENT AND EVALUATION OF INJURY
A comprehensive history and detailed examination form the basis of decision-making. Salient points in the history include the hand dominance, nature and timing of injury, occupation, hobbies, and patient’s expectations of the final outcome. Lengthy microsurgical procedures may produce a superior functional and aesthetic outcome but are not suitable in every patient. On the other hand, patients must understand the limitations of conventional (non-microsurgical) methods.
A complete hand examination should reveal the important findings of soft tissue deficits, bone or joint injuries, nail bed or tendon lacerations (including zones), neurological damage, and condition of the remaining fingers. Standard investigations should include lateral and anteroposterior radiographs with additional special views for certain injuries, for example, carpometacarpophalangeal (CMC) joint or carpal injuries. Computerized tomography or magnetic resonance imaging is useful to detect certain wrist or ligamentous injuries.
TABLE 84.1 GUIDELINES FOR THUMB RECONSTRUCTION BASED ON THE RECONSTRUCTIVE EMPHASES, OBJECTIVES, AND OPTIONS | |||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Special considerations for thumb reconstruction from the history, examination, and investigations therefore include:
Conditions for opposition:
Thumb opposition depends on an intact basal joint and functional thenar muscles. If these are damaged or deficient, an intact range of movement at the interphalangeal joint may compensate to a certain degree but hand function is impaired. In a thumb with a badly damaged CMC joint, the creation of an immobile post facilitates some degree of functional restoration but the thumb lacks finesse of function. Additional procedures may include addressing any concomitant narrowing or contracture of the first web space to achieve optimum opposition.
Condition of the remaining fingers:
An opposable thumb is dependent on its finger counterparts. In the severely mutilated hand, careful positioning of any new thumb or fingers remains critical to ensure adequate pulp-to-pulp or pulp-to-side contact and sufficient grip strength (see below, types IIC and IID metacarpal hand reconstruction).
Patient’s motivation and expectations:
For optimum functional recovery, the patients’ cooperation with rehabilitation must follow closely with the reconstructive efforts. It is imperative to obtain this commitment from the patients before subjecting them to any form of surgery, especially if embarking on a lengthy reconstructive procedure. For microsurgical methods, concerns regarding donor foot morbidity must be addressed because this may influence the types of toe flap used for reconstruction.
RECONSTRUCTIVE STRATEGIES
Thumb deficits can be classified into two broad strategies: defects or amputations. Partial thumb losses result in a variety of missing components and the main goal is to resurface or replace components. Amputations result in complete thumb loss and the goal is to completely restore the length of missing thumb (see Table 84.1). Considerable overlaps exist; for
resurfacing and replacement of missing components, as well as for amputations (see Table 84.1). For example, the free glabrous skin flap is an excellent option for resurfacing volar pulp defects.
resurfacing and replacement of missing components, as well as for amputations (see Table 84.1). For example, the free glabrous skin flap is an excellent option for resurfacing volar pulp defects.
Reconstruction of Thumb Defects
Thumb injuries result in a number of damaged components, including bone, joints, neurovascular bundles, tendons, and soft tissue. Skeletal injuries without missing bony components are managed by accurate anatomic reduction and early mobilization to prevent joint stiffness. In severely damaged joints, arthrodesis remains a valid option for the thumb interphalangeal and even the metacarpophalangeal joint, provided the CMC joint remains mobile. In general, mobility of two out of three joints (including the carpometacarpal joint) should be preserved to achieve effective opposition. Any bony losses should be replaced with bone grafts to maintain length and stability of the thumb. Nerve defects are replaced with nerve grafts whenever possible to restore sensation to the thumb tip. Excellent sources of nerve grafts are the distal posterior interosseous nerve or the medial cutaneous nerve of forearm. For more extensive composite losses including the loss of multiple components, microsurgical reconstructions with composite flaps can be excellent choices to achieve primary, total reconstruction in a single-stage procedure.
More commonly, thumb defects present with skin or soft tissue losses that require resurfacing. A useful classification for coverage of thumb defects is to separately consider the requirements of dorsal and volar defects. Volar pulp defects require pain-free and glabrous (non-slippery) skin with good sensibility, whereas dorsal defects do not require sensate skin to the same degree but have greater cosmetic considerations due to the aesthetic nature of the nail on the thumb tip. Small, superficial volar defects less than 1 cm2 in surface area possess an astonishing ability for healing by secondary intention. The use of wet dressings and antimicrobial cream will promote enough epithelialization within 2 to 3 weeks to cover the raw surfaces. However, deeper defects, or those associated with exposure of the bone, joint, and tendons, especially on the volar aspect, require coverage with local or even microsurgical reconstruction with glabrous skin flaps to achieve optimum results. Local flaps in thumb reconstruction can be homodigital or heterodigital and should ideally meet all the requirements for sensibility and good contour match with minimal donor-site morbidity.
Homodigital Local Flaps.
For partial volar pulp defects not crossing the interphalangeal joint, V-Y advancement flaps of the Tranquilli-Leali or Atasoy design are ideal local options to restore pulp and preserve length.3 For defects up to and involving the entire pulp, the Moberg advancement flap can be used effectively, ideally by the incorporation of a V-Y advancement flap proximally to avoid interphalangeal joint flexion as described by O’Brien.4 Based on both neurovascular bundles, this island flap is uniquely suited for thumb reconstruction due to the robust independent dorsal blood supply to the thumb tip. For resurfacing finger tip injuries, this flap design should be used with extreme caution because the lack of independent dorsal blood supply can lead to higher risk of distal flap loss.5 The main consideration in dorsal defects is the nail complex, which should be reconstructed whenever possible. More proximal defects not involving the nail can be reconstructed using standard homodigital advancement flaps of the hatchet design, by taking advantage of the skin laxity on the dorsum of the hand. For both volar and dorsal defects, flaps raised from the region of the first web space, either of the dorsal ulnar or radial designs, are useful alternatives although these flaps are not innervated.6 The anatomical basis of these flaps is derived from the constant communication between the dorsal arteries and proper digital arteries that allow the flaps to be raised with a reliable reverse flow through these distal arcades.
Heterodigital Local Flaps.
Heterodigital flaps are useful options when the rest of the thumb is injured or where local tissues are inadequate for homodigital options. Choices include the Littler neurovascular flap, first dorsal metacarpal artery flap, innervated lateral middle phalangeal finger flap,7 or the heterodigital arterialized flap from the middle finger.8 Crossed-finger flaps are available as a backup option but should always be used as a last resort as they restrict thumb and donor finger movements and interfere with rehabilitation.
Distant or Regional Flaps.
For larger or circumferential defects, regional or distant flaps such as the posterior interosseous flap or reversed radial forearm flap are useful for resurfacing. However, the resultant donor-site morbidity has become less acceptable in today’s practice. The pedicled groin flap remains a reasonable option for the coverage of defects in the dorsum of the hand extending to the thumb, as it avoids further upper limb donor morbidity, offers plenty of redundant skin, and leaves an almost negligible donor scar (Figure 84.1). Despite the disadvantage of having the injured hand in a dependent position, it is also a useful option for the interim coverage of larger thumb defects prior to a toe-to- thumb transplantation without the need to sacrifice any local tissues or recipient vessels.
Microsurgical Free Tissue Transfer.
The advent of microsurgery and toe-to-hand transplantation ushered in the possibility of composite tissue replacement as an elegant, one-stage reconstruction without causing further donor morbidity to the rest of the hand. Different flaps have been described, including vascularized osteocutaneous flaps from the groin or vascularized tendon-cutaneous flaps based on the dorsalis pedis region.9 Although these flaps greatly increase the versatility of reconstruction for compound hand and thumb defects, the donor morbidity should be carefully considered and explained to the patient. For resurfacing of volar thumb pulp defects, the free toe pulp or hemi-pulp remains an excellent option in providing a sensate, stable pulp with glabrous skin.
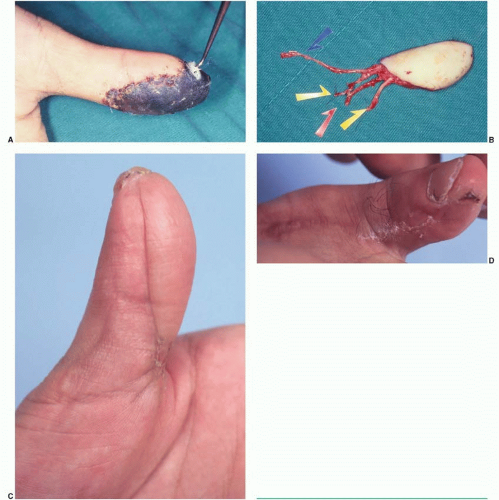
Free Toe Pulp-Flap Design and Elevation. The fibula side of the great toe is selected more often as a donor site than the second toe for the following advantages: it has better two-point discrimination (approximately 7 to 18 mm); more tissue is available; and the possibility for direct closure (avoiding a skin graft) is greater.10 Preoperatively, the skin incisions are outlined according to a template of the defect and extended proximally over the course of the proper digital artery to the first web space. This is where the dissection begins to identify whether the dominant arterial pedicle is the first dorsal or
plantar metatarsal arteries (Figure 84.2).11 Once the pedicles (arterial and venous) are identified, efforts are made to meticulously strip off the adventitia to facilitate their tunneling to the recipient vessels during flap inset. The proper digital nerve on the fibula side or terminal branches of the deep peroneal nerve can be included in the flap for subsequent reinnervation with either the proper digital or dorsal digital nerves of the thumb.
plantar metatarsal arteries (Figure 84.2).11 Once the pedicles (arterial and venous) are identified, efforts are made to meticulously strip off the adventitia to facilitate their tunneling to the recipient vessels during flap inset. The proper digital nerve on the fibula side or terminal branches of the deep peroneal nerve can be included in the flap for subsequent reinnervation with either the proper digital or dorsal digital nerves of the thumb.
RECONSTRUCTION OF THUMB AMPUTATIONS
Amputation of the thumb represents one of the few instances when there is an almost absolute indication for replantation. In the hand with multiple amputations, including the thumb, sacrificing a finger for the thumb as a heterotopic replantation may be a suitable option.12 When replantation fails, various methods (non-microsurgical or microsurgical) are considered to restore the four objectives of length, sensibility, mobility, and aesthetic appearance necessary for a successful thumb reconstruction.
Microsurgical Versus Non-Microsurgical: Which Is Better?
Conventional (non-microsurgical) methods fulfill some but not all of the above four objectives (see Table 84.2). With the advent of microsurgery, toe-to-hand transplantation is an ideal option that facilitates a custom-made, “like-for-like” and single-stage replacement of the amputated thumb at different levels. The foot is a warehouse of flaps in providing tissues of various configurations to “best fit” the missing components. Despite these advantages, one must consider
the available expertise and resources for microsurgery, as well as the fitness of patient to tolerate a long microsurgical procedure. Table 84.2 shows the different conventional methods and their comparisons with microsurgical methods with regard to outcomes and also donor morbidity.
the available expertise and resources for microsurgery, as well as the fitness of patient to tolerate a long microsurgical procedure. Table 84.2 shows the different conventional methods and their comparisons with microsurgical methods with regard to outcomes and also donor morbidity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree