This article provides an update on the contemporary use of the thermally confined micropulsed 1444-nm Nd:YAG interstitial fiber laser in the aging face and neck. Beginning with the concept that the use of Nd:YAG fiber lasers in aesthetic surgery is no longer limited to laser lipolysis, the article also covers the differentiating characteristics of the available Nd:YAG fiber laser wavelengths and laser tissue interaction and safety considerations when incorporating the use of these lasers into aging face surgery.
Key points
- •
The micropulsed 1444-nm Nd:YAG interstitial fiber laser enables precision contouring of the mid- and lower face and the neck, both as stand-alone procedures (laser-assisted facial contouring [LAFC] and laser-assisted neck contouring [LANC]) and as an adjunct during aging face surgery (laser-assisted facelift [LAFL]).
- •
Use of the 1444-nm Nd:YAG interstitial fiber laser requires knowledge regarding how to maintain safe clinical thermal confinement during treatment.
- •
Integrating this technology with facelift surgery facilitates elevation of (extended, if desired) cervicofacial rhytidectomy flaps, enables percutaneous release of major fascial retaining ligaments in the mid- and lower face, may obviate open submentoplasty and platysmaplasty in some patients, and facilitates greater posterior and superior repositioning of flaps for improved outcomes.
Introduction
Although the use of Nd:YAG fiber lasers in aesthetic surgery has been traditionally referred to as laser lipolysis , it is now evident that subcutaneous fat may not or need not be the primary laser target. As such, the use of Nd:YAG fiber lasers has evolved to include ablation and emulsification of subcutaneous fatty tissue, fibrolysis, and shrinkage of fine skin ligaments (ligamentae retinacula cutis) and more dense structural osseocutaneous anchoring ligaments (eg, zygomatic- and mandibular-cutaneous ligaments) as well as postulated direct tissue effects that may contribute to tightening of the skin and of the platysma muscle. Because the use of Nd:YAG fiber lasers goes beyond direct treatment of subcutaneous fat, some laser surgeons now advocate the term, interstitial laser , in lieu of laser lipolysis when referencing the use of these devices.
Subcutaneous Nd:YAG fiber laser tissue interaction is influenced by a variety of factors, including laser wavelength, power, pulse duration and total energy applied, target tissue composition, and relative amounts of exogenous water added to the treatment area. Collectively these factors influence opposing characteristics of fiber laser tissue interaction, termed thermal confinement and thermal diffusivity (discussed later), whereas related clinical implications affect subcutaneous Nd:YAG fiber laser treatment protocols and safety and immediately observed and late tissue effects.
Evaluation of absorption spectra for Nd:YAG fiber lasers reveals absorption in fat and water is greatest in the mid–1400-nm range, intermediate at 1320 nm, and least at 1064 nm. The relative absorption is on the order of 1 magnitude higher for fat but many orders of magnitude higher for water in the mid–1400-nm range versus 1320 nm and 1064 nm. A minor anhydrous collagen absorption peak present in the mid–1400-nm range may also influence laser energy absorption and laser tissue interaction. Comparison of direct tissue effects reveals that fatty tissue ablation crater depth and fatty tissue ablation efficiency are greatest at 1444 nm, intermediate at 1320 nm, and least at 1064 nm. Differences in tissue absorption and laser tissue interaction among Nd:YAG fiber lasers are summarized in Table 1 .
| Mid–1400 nm | 1320 nm | 1064 nm | |
|---|---|---|---|
| Water absorption | Highest a | Intermediate | Lowest |
| Fat absorption | Highest a | Intermediate | Lower |
| Collagen (anhydrous) absorption | Low a | — | — |
| Fatty tissue ablation efficiency | Highest | Intermediate | Least |
a Absorption peaks for water, fat, and collagen occur in the mid–1400-nm range.
Thermal confinement and thermal diffusivity are opposing characteristics of fiber laser tissue interaction that are of critical importance for exerting desired laser tissue effects while avoiding undesired complications. Thermal confinement refers to spatial limitation of tissue heating relatively near the tip of the laser fiber or more broadly within the desired tissue treatment area whereas thermal diffusivity refers to heat distribution away from the source or tip of the laser fiber via conduction. Although the 2 phenomena are simultaneously present, the relative proportions are influenced by laser wavelength, power, and pulse duration as well as target tissue composition, tissue water content, and total laser energy applied to the treatment area—their differential effects on thermal confinement and diffusivity are summarized in Table 2 .
Thermal imaging studies among the Nd:YAG fiber laser wavelengths demonstrate that thermal confinement is greatest at mid–1400 nm, intermediate at 1064 nm, and least at 1320 nm. Clinically, improved thermal confinement translates to a longer lag period or larger therapeutic window that precedes significant heat accumulation in the larger laser treatment area. The ability of the tissue and exogenous water in the treatment area to maintain thermal confinement is exceeded at the far side of the therapeutic window where thermal diffusivity then prevails with more rapid tissue heating from that point forward. Various tissues have specific tolerances to prolonged heating—irreversible coagulation of the skin may occur with heating to 59°C for as little as 1 second. Excessive thermal diffusion leading to irreversible tissue injury indicates a clinical failure of thermal confinement.
Native target tissue composition affects Nd:YAG fiber laser tissue interaction. Although relative adipocyte may not able to be estimated versus fibrous tissue content prior to laser treatment, this can be inferred based on the tissue response. If the tissues soften during treatment, significant fat emulsification and liquefaction have generally occurred. Significant firming and tightening of the tissues suggest a greater fibrous tissue content with contraction of collagen containing structures; significant fat emulsification and liquefaction may still have occurred despite the firmness but greater mechanical effort may be required for its removal during lipoaspiration.
Introduction
Although the use of Nd:YAG fiber lasers in aesthetic surgery has been traditionally referred to as laser lipolysis , it is now evident that subcutaneous fat may not or need not be the primary laser target. As such, the use of Nd:YAG fiber lasers has evolved to include ablation and emulsification of subcutaneous fatty tissue, fibrolysis, and shrinkage of fine skin ligaments (ligamentae retinacula cutis) and more dense structural osseocutaneous anchoring ligaments (eg, zygomatic- and mandibular-cutaneous ligaments) as well as postulated direct tissue effects that may contribute to tightening of the skin and of the platysma muscle. Because the use of Nd:YAG fiber lasers goes beyond direct treatment of subcutaneous fat, some laser surgeons now advocate the term, interstitial laser , in lieu of laser lipolysis when referencing the use of these devices.
Subcutaneous Nd:YAG fiber laser tissue interaction is influenced by a variety of factors, including laser wavelength, power, pulse duration and total energy applied, target tissue composition, and relative amounts of exogenous water added to the treatment area. Collectively these factors influence opposing characteristics of fiber laser tissue interaction, termed thermal confinement and thermal diffusivity (discussed later), whereas related clinical implications affect subcutaneous Nd:YAG fiber laser treatment protocols and safety and immediately observed and late tissue effects.
Evaluation of absorption spectra for Nd:YAG fiber lasers reveals absorption in fat and water is greatest in the mid–1400-nm range, intermediate at 1320 nm, and least at 1064 nm. The relative absorption is on the order of 1 magnitude higher for fat but many orders of magnitude higher for water in the mid–1400-nm range versus 1320 nm and 1064 nm. A minor anhydrous collagen absorption peak present in the mid–1400-nm range may also influence laser energy absorption and laser tissue interaction. Comparison of direct tissue effects reveals that fatty tissue ablation crater depth and fatty tissue ablation efficiency are greatest at 1444 nm, intermediate at 1320 nm, and least at 1064 nm. Differences in tissue absorption and laser tissue interaction among Nd:YAG fiber lasers are summarized in Table 1 .
| Mid–1400 nm | 1320 nm | 1064 nm | |
|---|---|---|---|
| Water absorption | Highest a | Intermediate | Lowest |
| Fat absorption | Highest a | Intermediate | Lower |
| Collagen (anhydrous) absorption | Low a | — | — |
| Fatty tissue ablation efficiency | Highest | Intermediate | Least |
a Absorption peaks for water, fat, and collagen occur in the mid–1400-nm range.
Thermal confinement and thermal diffusivity are opposing characteristics of fiber laser tissue interaction that are of critical importance for exerting desired laser tissue effects while avoiding undesired complications. Thermal confinement refers to spatial limitation of tissue heating relatively near the tip of the laser fiber or more broadly within the desired tissue treatment area whereas thermal diffusivity refers to heat distribution away from the source or tip of the laser fiber via conduction. Although the 2 phenomena are simultaneously present, the relative proportions are influenced by laser wavelength, power, and pulse duration as well as target tissue composition, tissue water content, and total laser energy applied to the treatment area—their differential effects on thermal confinement and diffusivity are summarized in Table 2 .
Thermal imaging studies among the Nd:YAG fiber laser wavelengths demonstrate that thermal confinement is greatest at mid–1400 nm, intermediate at 1064 nm, and least at 1320 nm. Clinically, improved thermal confinement translates to a longer lag period or larger therapeutic window that precedes significant heat accumulation in the larger laser treatment area. The ability of the tissue and exogenous water in the treatment area to maintain thermal confinement is exceeded at the far side of the therapeutic window where thermal diffusivity then prevails with more rapid tissue heating from that point forward. Various tissues have specific tolerances to prolonged heating—irreversible coagulation of the skin may occur with heating to 59°C for as little as 1 second. Excessive thermal diffusion leading to irreversible tissue injury indicates a clinical failure of thermal confinement.
Native target tissue composition affects Nd:YAG fiber laser tissue interaction. Although relative adipocyte may not able to be estimated versus fibrous tissue content prior to laser treatment, this can be inferred based on the tissue response. If the tissues soften during treatment, significant fat emulsification and liquefaction have generally occurred. Significant firming and tightening of the tissues suggest a greater fibrous tissue content with contraction of collagen containing structures; significant fat emulsification and liquefaction may still have occurred despite the firmness but greater mechanical effort may be required for its removal during lipoaspiration.
Interstitial Nd:YAG fiber laser–assisted facial contouring
Interstitial Nd:YAG fiber LAFC may be used as a stand-alone percutaneous sculpting procedure for the midface, lower face/jawline, and the female round Asian face. LAFC of the mid- and/or lower face as a stand-alone treatment is generally more successful in female patients. Volumetric sculpting of the mid- and/or lower face (ie, soft tissue reduction) with LAFC complements well-established procedures for soft tissue augmentation and enables synergy through a proportionally greater effect with soft tissue augmentation. Appropriate patient selection should include those with mild to moderate fullness and readily palpable subcutaneous fat but without excessive skin laxity. Patients with skin laxity but no significant subcutaneous fat are not appropriate candidates for the LAFC procedure. Patient age is not a major determining factor with regard to successful outcomes—very good LAFC results have been obtained with patients into their early 70s.
Mild to moderate post-treatment inflammatory edema (PIE) is expected. Early on, PIE seems to have blunted or limited the lower facial tissue contouring response; however, lower facial contour improves over time as PIE gradually resolves and the skin contracts. Early on (eg, weeks 2 through 6), weekly lymphatic massage sessions for the LAFC treatment areas may help reduce PIE and improve lower facial contour. Significant PIE may be treated with staged escalating-dose intralesional triamcinolone (eg, 10 mg/mL initially, gradually moving to 40 mg/mL) beginning at post-treatment month 1 or 2 and continuing monthly as needed until final desired contour is achieved or until no further tissue response. Although this approach is successful in a majority of patients with PIE, the origin of persistent lower facial fullness with palpable subcutaneous fullness in partial responders is not known.
Some of the adipocyte lipid content liberated during laser lipolysis may be subject to reuptake by adipocytes that remain at the periphery of the treatment area. A significant increase in body mass index after LAFC could also partially account for a blunted tissue response. It seems more likely, however, that the natural healing response to adipose tissue ischemia and adipocyte necrosis may stimulate a tissue regeneration response, with adipose tissue remodeling involving adjacent adipose-derived stem progenitor cells and formation of neoadipocytes—this phenomenon has been carefully elucidated in animal models for adipose tissue ischemia and nonvascularized fat grafting. Persistent fullness 6 to 12 months after LAFC may be addressed through a touch-up percutaneous LAFC procedure.
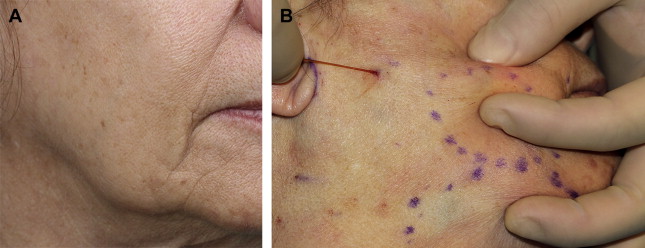
LAFC treatment begins with identification and marking of the desired treatment areas. In keeping with anatomic studies of the jowl fat compartment, the desired area of tissue ablation for contouring of the lower face and jawline may include subcutaneous tissue fullness at, below, and well above the caudal border of the mandible ( Fig. 1 A). In many patients, the position of the jowl changes substantially with supine or slight Trendelenburg positioning; therefore, patient marking for LAFC should be done with patients in an upright, seated position to most accurately ensure inclusion of the desired tissue in the outlined treatment areas. The LAFC percutaneous entry point should be at least 1.5-cm posterior to the posterior extent of the intended LAFC treatment zone to ensure that an adequate tissue seal is maintained between the entry point and the treatment zone. If the entry point is placed too close to the LAFC treatment zone, the lipoaspiration step may be more difficult and inefficient because air may easily be drawn into the aspiration syringe.