I. SCOPE OF THE PROBLEM FOR THERMAL INJURY
A. Burns are a major source of morbidity: Approximately 2 million burns occur per year.
B. Burns result in over 60,000 hospitalizations and nearly 6,000 deaths per year.
C. Total healthcare expenditures approach 4 billion dollars per year.
II. PATHOPHYSIOLOGY OF BURN INJURY
A. Coagulaiton of protein due to intense heat
B. Release of local mediators
C. Change in blood flow due to vasoconstriction and thrombosis
D. Tissue edema
III. SYSTEMIC EFFECTS
A. Loss of skin’s barrier function leads to fluid loss and massive fluid shifts.
B. Injured tissues release vasoactive mediators with secondary interstitial edema, hypoproteinemia, fluid shifts, and organ dysfunction.
C. Bacterial translocation
D. Immune function: Hypermetabolic state
1. *Initial response: Decreased cardiac output, decreased metabolic rate
2. 24 to 48 hour after injury: Increased cardiac output (2 times normal), increased metabolic rate (2 times normal).
3. Hypothalamic function altered: Increased glucagon/cortisol/Catecholamines
4. GI barrier function breaks down, leads to bacterial translocation
5. Nutritional needs dramatically increase (2 to 3 times normal)
6. Overall catabolic state
7. *Strategies to alter the hypermetabolic state have included antipyretics, β-adrenergic bolckade, NSAIDs, growth hormone, and IGF-1 are areas of active investigation.
IV. BURN INJURY SEVERITY
A. Total body surface area (TBSA) burned and presence of inhalation injury are the most important.
B. Depth of burn can be affected by temperature, duration of contact, and thickness of skin.
C. Patient comorbidities and age are other important factors
D. Patients may have coexisting traumatic injury (motor vehicle accidents, explosions, etc.)
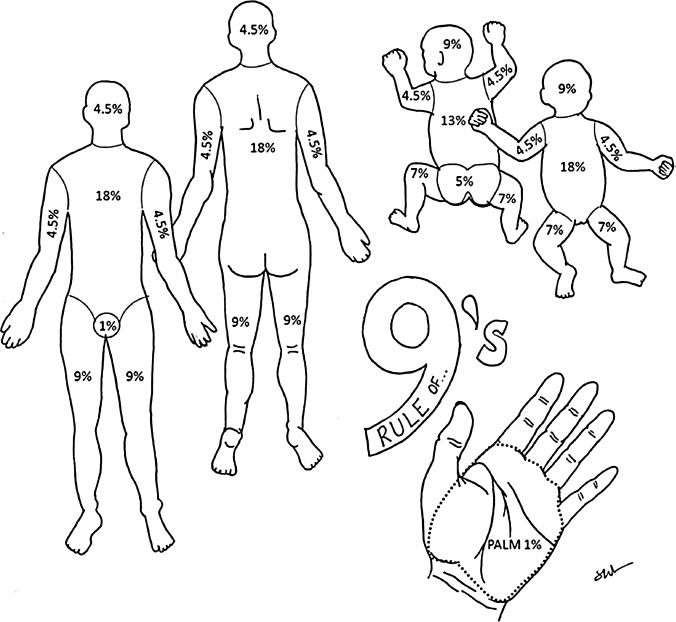
V. TBSA CAN BE ESTIMATED BY THE “RULE OF NINES” (FIG. 54-1)
A. The Rule of Nines is altered for children and infants whose heads are larger and extremities smaller than adult patients.
B. The size of a patient’s palm is a reasonable estimate of 1% of TBSA.
VI. DEPTH OF BURN
A. Superficial burns
1. Involve the epidermis
______________
*Denotes common in-service examination topics
Figure 54-1. Percent total body surface area burn as estimated by location in adults and children (“Rule of Nines”).
2. Symptoms similar to a bad sunburn and include hyperemia, blanching skin, and tenderness to palpation.
3. Blisters are not present
B. Partial-thickness burns
1. Involve the dermis and are categorized into superficial partial-thickness and deep partial-thickness burns.
2. Superficial partial thickness
a. Papillary dermis involved without involvement of skin appendages
b. Raw surfaces are deeper red and tender to palpation
c. Blisters (either intact or ruptured) will be present
d. Blanches with pressure
e. If the dermal appendages are intact, then healing without skin grafting is possible.
3. Deep partial thickness
a. Reticular dermis involved with skin appendages
b. No capillary refill
c. White
d. Decreased sensation
C. Full-thickness burns result in destruction of the epidermal and dermal layers
1. Burns extend into the subcutaneous tissues, muscle, or bone.
2. Skin is white and nonblanching or, in deeper burns, dry and leathery in appearance. No sensation is present. If a burn is painful, it is not full thickness (sensory nerves are preserved).
3. Will not heal on own and will require surgery for coverage or closure.
A. Inhalation injury occurs in ∼10% of burn patients. However, inhalation injury is present in ∼70% of patients who die of their burn injury.
B. History often includes fire in an enclosed space such as a basement.
C. Physical examination characteristics include singed nasal hairs, facial burns, carbonaceous sputum, and/or hoarseness
1. Agitation or shortness of breath may be caused by hypoxia.
2. Fluorescein eye examination is mandatory for patients with facial burns.
D. *Definitive diagnosis is made by direct airway examination using nasopharyngeal scope or fiberoptic bronchoscopy.
1. Early intubation for airway protection is mandatory.
2. Intubation becomes much harder when the airway swells.
E. Inhalation injury can be divided into three categories
1. Injury above the glottis is typically from inhalation of superheated air.
2. Injury below the glottis is due to smoke particles damaging large airway epithelium.
3. Carbon monoxide (CO) poisoning
a. Occurs because CO has 200 times affinity for hemoglobin compared to O2.
b. CO will shift oxygen disassociation curve to the left and create tissue hypoxia.
c. Physical examination classically demonstrates cherry red color of mucous membranes, altered level of consciousness and agitation.
d. Carbon dioxide removal is unaffected, so cyanosis and tachypnea are less likely.
e. Pulse oximetry may be normal (cannot distinguish between CO and O2).
f. Treatment is 100% oxygen because CO half life is 4 hours on room air versus 1 hour on 100% FiO2.
F. Upper airway swelling
1. Most common manifestation of inhalation injury.
2. Results from dissipation of heat energy into tissues of the pharynx, larynx, and vocal cords.
3. Process begins several hours after injury lasts 2 to 4 days until edema resolves.
4. Diagnosis: Direct visualization of the upper airway
5. Intubate if swelling, erythema, or soot is present on examination.
6. Indications for extubation:
a. Passed spontaneous breathing trial for at least 15-30 minutes.
b. Adequate resolution of laryngeal edema as assessed by direct laryngoscopy or fiberoptic larygncoscopy.
c. Can also assess cuff leak with cuff deflated but this is not very sensitive or specific.
G. Acute respiratory failure
1. Chemical pneumonitis caused by toxic products of combustion.
2. Exacerbated by generalized tissue edema and a systemic and local inflammatory response.
3. Treatment: Intubation, PEEP, low FiO2, frequent suctioning, and supportive measures.
4. May occur several days into hospitalization due to hospital acquired pneumonia.
VIII. CRITERIA FOR TRANSFER TO BURN CENTER
A. Partial- or full-thickness burns >10% TBSA
B. Burns involve the face, hands, feet, genitalia, perineum, or major joints
C. Electrical or chemical burns
D. Inhalation injuries
E. Children in hospitals not equipped to treat pediatric patients
F. Patients with significant comorbid medical conditions
G. Trauma patients where the burn injury poses the greatest risk of morbidity or mortality.
H. Patients with burns who require social, emotional, and rehabilitative services
A. *The Parkland Formula is widely used to estimate fluid requirements in the first 24 hours
1. *First 24-hour requirement = 4 cc × %TBSA × weight in kilograms
a. For fluid resuscitation, only partial- and full-thickness burns count toward TBSA; do not include superficial/first degree burns.
b. Lactated Ringer’s solution (LR) should be used as its composition is closest to extracellular fluid.
c. Do not resuscitate with colloids (though some studies show patients with low albumin might benefit).
2. *Administer half of the above volume during the first 8 hours (calculated from the time of injury, not the time of hospital admission), and the other half over the next 16 hours.
3. Pediatric patients
a. Add maintenance fluid with D5 LR
b. Infants and children have limited stores of glycogen which can quickly lead to hypoglycemia.
4. *The adequacy of resuscitation is best judged by hourly urine output (0.5 mL/kg/h in adults or 1 mL/kg/h in children)
5. Also important to follow trend of base deficit, lactate and pH. These should continue to go down with adequate resuscitation.
6. Swan Ganz Catheter or bedside ultrasound (IVC filling and cardiac contractility) can also be used to assess fluid status.
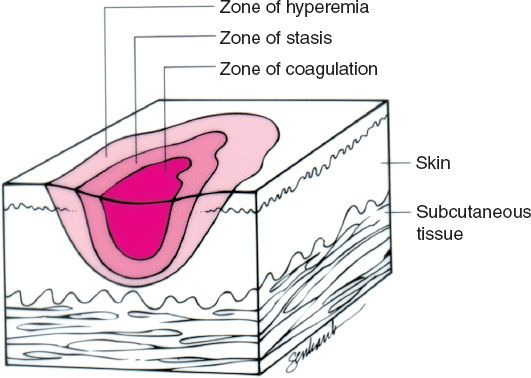
B. *Jackson burn model describes the distinct areas within every burn wound (Fig. 54-2)
1. Zone of coagulation
a. Tissue is severely damaged and will not recover
b. Treatment: excision and grafting
2. Zone of stasis
a. Tissue is inflamed with impaired vasculature
b. Tissue may recover with appropriate resuscitation
c. Surrounds zone of coagulation
d. Treatment: Aggressive resuscitation
3. Zone of hyperemia
a. Tissue has intense vasodilation with increased bloodflow and should recover
b. Treatment: Aggressive resuscitation
Figure 54-2. Jackson burn model.
C. Fluid resuscitation and should be assessed on an hourly basis
1. Fluids should be regularly adjusted to maintain adequate urine output as both under- and over-resuscitation have severe consequences. Keep in mind that urine output might lag early in the resuscitation and it is important to avoid giving too much fluid to just increase urine if other parameters continue to improve.
2. Jackson’s zone of stasis can potentially be salvageable with judicious fluid resuscitation. Under- or over-resuscitation may result in additional tissue loss.
3. Over-resuscitation can predispose to
a. Pulmonary edema with prolonged ventilator requirements.
b. Increased tissue edema with subsequent need for escharotomy.
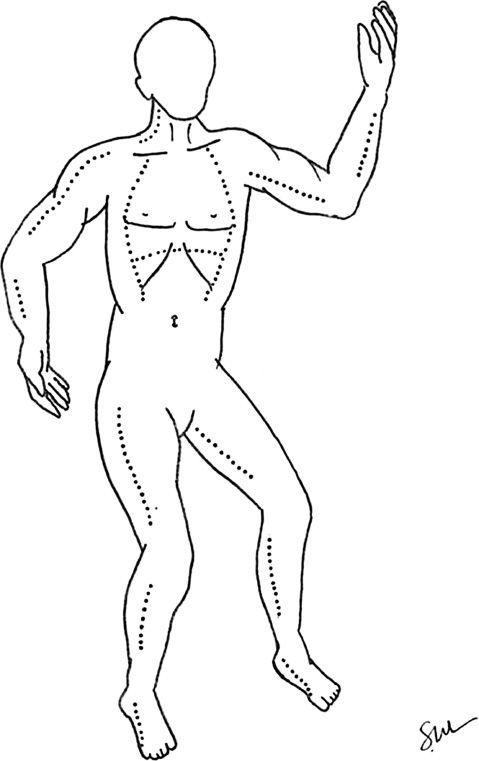
X. CIRCUMFERENTIAL BURNS AND ESCHAROTOMY (FIG. 54-3)
A. Circumferential burns
1. Can produce a tight, inelastic contraction with limited ability for expansion of tissues.
2. As tissue edema develops during resuscitation, supra-physiologic pressures can develop with subsequent tissue ischemia and necrosis.
Figure 54-3. Recommended escharotomy incisions are marked with dotted lines.
1. Physical signs are often obscured by the burn injury or tissue edema. However, physical examination remains your best clinical diagnostic tool.
2. Doppler examination is unreliable in estimating tissue perfusion.
C. Burned chest: Circumferential burns can cause difficulty in ventilation with high peak pulmonary pressures.
D. Burned abdomen
1. Circumferential burns can create an abdominal compartment syndrome.
2. Bladder pressure is a good estimate of intra-abdominal pressure and can be measured via the foley catheter.
E. Escharotomy is an incision of burned skin to relieve constriction.
1. When designing escharotomy incisions, remember that all burned skin will eventually be excised, so standard rules (e.g., not making an incision perpendicular to a joint) do not apply.
2. Electrocautery incision is the method of choice, and can be performed at the bedside, as the burned skin is anesthetic.
a. Need to connect unburned skin to unburned skin.
b. Burn eschar will “pop” when the constriction is released and a gap between edges of burned tissues will be created.
c. Healthy, viable tissue (usually fat) should be present at the wound base.
3. Arms and legs
a. Can be decompressed with axially oriented medial and lateral incisions.
b. Digital escharotomies are not typically needed.
4. Chest and upper abdomen
a. Can be decompressed with bilateral midaxillary releases.
b. These can be connected with one or multiple horizontal incision to form an “H”.
XI. BURN WOUND CARE
A. All blisters and nonviable tissue should be debrided at the bedside. Wounds should be dressed with a topical antimicrobial agent.
1. Silvadene (1% silver sulfadiazene) has broad coverage for gram-negative and -positive bacteria.
a. Wound penetration is moderate
b. Can damage the cornea so use near the eyes is contraindicated
c. *Can cause neutropenia so white blood cell count should be followed
d. Avoid in patients with sulfa allergy
2. Sulfamylon (10% mafenide acetate) has broad coverage for gram-positive bacteria and is bacteriostatic.
a. Wound and eschar penetration is excellent.
b. Sulfamylon is the topic agent of choice for exposed cartilage of the ear or nose.
c. *Sulfamylon is a carbonic anhydrase inhibitor and can cause hyperchloremic acidosis, particularly when used in large burns.
d. Avoid use in burns greater than 20% TBSA.
3. Silver nitrate (0.5% solution) has broad spectrum coverage with coverage of Staphylococcus and Pseudomonas
a. Silver nitrate solution does not penetrate eschar well.
b. Silver nitrate solution will discolor the adjacent skin and surrounding dressings and bedding.
c. *Silver nitrate can cause hyponatremia. Sodium level should be followed.
d. Cost effective.
4. Acticoat is a silver-impregnated dressing that is available in sheets. Moisture activates the silver ions, which act as a topical antimicrobial agent.
a. Sheets can be placed over clean burn wounds and moistened with normal saline several times per day. Dressings can be changed every 3 to 5 days.
b. Acticoat is available in glove form, which is ideal for clean, partial-thickness burns of the hand.
5. Bacitracin zinc ointment can provide coverage for gram-positive organisms
a. Bacitracin penetrates burn eschar
b. Commonly used for facial burns
c. Bacitracin is safe for use around the eye
XII. BURN WOUND DEBRIDEMENT AND GRAFTING
A. Initial debridement of blisters should be performed at the bedside prior to initial wound dressing.
B. Formal debridement and grafting in the operating room is performed after adequate resuscitation and when the patient is hemodynamically stable
1. Early debridement can prevent burn wound infection; the first debridement is often within 2 to 4 days of injury.
2. For large burns, sequential debridement and grafting is appropriate.
3. Ideally, all burn wounds would be grafted by 3 weeks to prevent hypertrophic scar formation, however, in very large burns, it is important to perform early escharotomies to remove the large bioburden of dead tissue.
C. Tangential excision allows sequential excision of thin layers of nonviable tissue until bleeding, healthy tissue is reached.
1. Thin layer sequential excision of all nonviable tissue, until a viable tissue level is reached
2. At debridement, the most important distinction is between superficial and deep partial-thickness burns.
a. *Superficial partial-thickness injuries will heal on their own without grafting.
b. *Deep partial-thickness burns require skin grafting.
3. Delayed grafting can be performed if inadequate donor skin is present. Cover wounds first with cadaveric allograft or a nonbiologic dressing to protect against fluid losses and burn wound infection (see below)
D. Equipment needed in the OR
1. Weck knives and/or the Versajet for debridement
2. Epinephrine-soaked telfa for hemostasis
3. Blood products for as-needed use
4. Dermatome
5. Mesher
6. Carrier for mesher
7. Mineral oil
8. Dressing for donor site (typically xeroform gauze or a large Tegaderm)
9. Bolster materials
10. Staplers for both the graft and bolster
E. Grafting techniques (see “Grafts” Chapter 3)
1. Split-thickness grafts
a. Usually 12 to 14/1000th of an inch.
b. Thinner grafts preserve donor site and have higher take rates but are more prone to secondary contracture.
2. Meshing is typically performed at a 1:1.5 ratio to increase surface area and decrease fluid collection beneath the graft.
a. Higher mesh ratios (e.g., 1:2, 1:3, or 1:4) can be used but prolong healing.
b. Even if mesh, the less you need to spread out the graft, the better the graft appearance will be in the future and the less likely it will break down.
3. Unmeshed sheet grafts are typically used on cosmetic or functional areas, such as the face, breast, and hands.
F. *Graft failure can occur for many reasons
1. Inadequate wound debridement prior to graft application is the primary cause.
2. Quantitative cultures showing more than 105 cells will result in graft loss.
3. Fluid collection beneath the graft, including hematoma (most common) or seroma.
4. Shear force to graft from inadequate immobilization and compression.
5. Poor nutrition or overall physiologic status.
A. Autograft is a patient’s own skin and is the preferred grafting material when available.
1. Advantages include a single-stage reconstruction and reliable take on a clean, vascularized wound bed.
2. Disadvantages include creation of a second partial-thickness donor site
B. Allograft is a skin graft taken from a cadaver
1. Advantages
a. Limitless quantities when autograft is sparse.
b. Can temporarily revascularize and dermal elements may incorporate.
c. Allows coverage of burn wounds to minimize fluid loss and burn wound infection.
2. Disadvantages
a. Cost
b. Potential for disease transmission
c. Will eventually reject
C. Xenograft is a tissue graft between species
1. Advantages
a. Limitless quantities when autograft is sparse.
b. Allows coverage of burn wounds to minimize fluid loss and burn wound infection.
c. Good for patients with painful superficial partial thickness burns that will likely not require grafting.
2. Disadvantages
a. Predictable slough at ∼7 days because the graft cannot obtain blood supply.
b. Potential for disease transmission exists
D. Integra is a bilaminate bovine collagen construct that provides a decellularized matrix to be populated by patient’s own cells.
1. Advantages
a. Ability to cover over nonvascularized surfaces such as bone without periosteum or tendon without paratenon.
b. Will provide a vascularized wound bed in 3 to 4 weeks for grafting.
c. Allows usage of thin (6 to 8/1000th of an inch) skin graft to conserve donor site.
2. Disadvantages
a. High incidence of infection
b. Need for a second operation for skin grafting
c. Need for thin autograft harvest at second surgery
E. Cultured epithelial autograft cells are a patient’s own skin cells that are expanded in cell culture prior to grafting.
1. Advantages: Expansion of available autograft in patients with large surface area burns (>80%).
2. Disadvantages
a. 3 to 4 week lag time before cells are ready for grafting.
b. Creation of a thin, unstable coverage with no dermal elements.
c. High cost
d. Squamous cell cancer has been reported in patients treated with these grafts.
XIV. BURNS OF THE FACE, EYES, AND EARS
A. The central face has deeper skin appendages and excellent blood supply, resulting in a greater healing capacity.
B. Assessed using the subunit principle: When greater than 50% of a subunit requires grafting, excision and grafting of the entire subunit optimizes aesthetic outcome
1. Use unmeshed sheet grafts, applied by aesthetic units.
2. Thicker grafts (16 to 20/1000th of an inch) are preferable on the face.
3. Facial grafting should be performed less than 2 weeks from the time of injury to decrease scarring.
C. Eyes: Lid edema usually protects the eyes in the early stages. Patients are at risk of corneal exposure and corneal abrasion as edema subsides.
1. Opthalmology consult and fluorescent staining often indicated to assess for corneal abrasions.
2. Eye lubrication and/or temporary tarsorrhaphy may be required.
3. Definitive surgical correction to address anterior, middle, and posterior lamella
4. Goals
a. Restore the lid to the proper functional position.
b. Covering the inferior margin of the corneoscleral limbus in neutral gaze.
D. Ears: Ear skin is very thin and exposed cartilage is common
1. *Twice-daily sulfamylon is the best wound dressing for exposed cartilage.
2. Avoid any external pressure to the ear.
3. Suppurative chondritis requires urgent debridement.
4. If no cartilage exposure is present, split-thickness skin grafting and a bolster are appropriate.
5. Small amounts of exposed cartilage may be debrided to allow primary wound closure.
6. Large amounts of exposed cartilage necessitate vascularized coverage prior to grafting. An ipsilateral temporal-parietal fascia flap is ideal.
XV. BURNS OF THE HANDS AND FEET
A. Have a low threshold for early escharotomies of severely burned extremities.
B. Superficial extremity burns are treated with elevation, topical antimicrobials, and passive ROM for each joint BID.
C. *Burned hands should be splinted in the intrinsic plus position with the thumb maximally abducted.
D. If prolonged hospitalization and severe burns with exposed tendon, should consider K-wire hand in intrinsic plus.
E. Deep partial- and full-thickness burns.
1. Early excision and sheet grafting are preferred, particularly on the dorsum of the hand and fingers.
2. After 5 days of immobilization, ROM exercises should be restarted.
F. Exposed tendon may require local tissue rearrangement versus flap coverage versus integra placement.
G. Palmar skin is thick and only 20% of palmar burns ultimately require resurfacing. A conservative approach is recommended to preserve thick fascial attachments.
H. Burns of the feet are managed similarly to hand burns.
XVI. GENITAL BURNS
A. Place burned foreskin into its normal position to prevent paraphimosis.
B. Topical antibiotic therapy may be instituted for several weeks as needed. Any remaining open wounds should then be sheet-grafted.
C. Early consultation with an experienced urologist is recommended. The foley catheter may be removed at their discretion.
XVII. OPTHAMOLOGIC INJURY
A. Important to consult opthamology if concern for elevated intraocular pressures
B. Important to keep eyes well lubricated and consider tarsorraphy.
XVIII. NUTRITIONAL SUPPLEMENTATION
A. A hypermetabolic response is common to all large burns
1. The metabolic rate is proportional to the size of the burn, up to 60% TBSA, and remains constant thereafter.
2. This response begins soon after injury, reaching a plateau by the end of the first week.
3. Most burns >30% TBSA require intensive nutritional support until wound healing is complete.
4. *Curreri formula for caloric requirements: 24 hour caloric requirement = (25 kcal × kg body weight) + (40 kcal × %TBSA).
5. Protein requirements: 2.5 to 3 g/kg/day are recommended. In children, requirements are 3 to 4 g/kg/day.
B. Intestinal feeding should be performed early
1. Initial feeds can be performed using a nasogastric tube.
2. If feeds are administered to the stomach, feeding should be held 6 hours prior to the OR.
3. A post-pyloric Dobhoff tube is appropriate for long-term feeding. Post-pyloric feeds can be continued in the perioperative period.
C. Weekly nutrition labs, prealbumin levels are drawn to monitor nutrition status.
D. Early involvement of a registered dietician is imperative.
PEARLS
1. The Parkland formula is only a guide to approximate fluid replacement. Real-time monitoring of urine output is the most important indicator of adequate resuscitation.
2. Be wary of inhalation injury and have a low threshold for early endotracheal intubation
3. All patients with inhalation injury or facial burns should be evaluated with a fluorescein examination. Have a low threshold for opthamology consultation.
4. Escharotomy for circumferential burns can be life- or limb-saving
5. Wounds that are not closed by 3 weeks (through healing on their own or skin grafting) are at high risk for hypertrophic scar formation
6. During resuscitation, monitor urine output, pH, base deficit and lactate frequently.
QUESTIONS YOU WILL BE ASKED
1. How does a skin graft survive?
a. *Initially the graft survives by imbibition or diffusion of nutrients from the surrounding serum (first 48 hours).
b. Inosculation (days 2 to 3) connections forming between vessels in the skin graft and from the recipient site.
c. Revascularization, with new blood vessel ingrowth into the graft (days 5 to 7).
2. How should we deal with exposed ear cartilage?
a. Sulfamylon is the preferred topical wound dressing because it has good cartilage penetration.
b. Small amounts of exposed cartilage can be resected with primary closure.
c. Large amounts may require temporal-parietal flap closure with skin grafting.
3. By what time point should burn wounds be closed to prevent hypertrophic scar formation?
a. Three weeks.
4. What factors cause a skin graft to fail?
a. Shear forces
b. Infection or inadequate debridement
c. Fluid collection beneath the graft (hematoma most common, seroma)
THINGS TO DRAW
1. Draw basic schematic of percent burn percentage per body part (Fig. 54-1).
2. Draw incision lines for escharotomy (Fig. 54-3).
Recommended Readings
Friedstat JS, Klein MB. Acute management of facial burns. Clin Plast Surg. 2009;36(4):653–660. PMID: 19793559.
Klein MB, Moore ML, Costa B, Engrav LH. Primer on the management of face burns at the University of Washington. J Burn Care Rehabil. 2005;26(1):2–6. PMID: 15640725.
Sterling J, Gibran NS, Klein MB. Acute management of hand burns. Hand Clin. 2009;25(4):453–459. PMID: 19801119.
< div class='tao-gold-member'>