and Ziv Gil2
(1)
Division of Otolaryngology Head and Neck Surgery and Maxillofacial Surgery, Tel Aviv Sourasky Medical Center, Tel Aviv, Israel
(2)
The Head and Neck Center Department of Otolaryngology Head and Neck Surgery, Rambam Healthcare Campus, Haifa, Israel
Keywords
Translabyrinthine approachInternal auditory canalCerebellopontine angleVestibular schwannoma8.1 Introduction
The translabyrinthine (TL) approach is the most direct course to the internal auditory canal (IAC) and cerebellopontine angle (CPA). It was described as a route for removing vestibular schwannomas as early as the beginning of the twentieth century, in the early days of surgical treatment of this pathology, but the procedure was established as one of the main approaches to the region in the 1960s by Dr. William F. House [1]. It also has been used in the treatment of many other lesions in the area, such as meningiomas, cancer, and facial nerve schwannomas.
The TL approach allows for the exposure of the complete length of the intratemporal part of the facial nerve proximal from the stylomastoid foramen. This exposure serves as an aid for both extirpation of disease and reconstruction of the nerve, when needed. The TL approach is associated with lower rates of cerebrospinal fluid (CSF) leaks than the suboccipital approach, and it is also thought to have a lower rate of postoperative headaches [2, 3]. The TL approach usually requires limited cerebellar retraction. These advantages have made the TL approach popular with many skull base surgeons.
8.2 Indications for the Procedure
The TL approach provides wide and direct access for removal of tumors involving the IAC and CPA with minimal cerebellar retraction. The most common lesions are vestibular and cochlear schwannomas. Other tumors also can be addressed, such as meningiomas, squamous cell and glandular carcinomas, endolymphatic sac tumors, and epidermoids. Tumors and traumatic or iatrogenic lesions of the facial nerve can be effectively treated via the TL approach, as its exposure of the nerve’s complete intracranial and intratemporal route permits positive facial nerve identification and manipulation from the brainstem to the stylomastoid foramen. Thus, tumors involving the facial nerve can be dissected from either direction with optimal control of the nerve. Reanimation of an injured facial nerve is facilitated by the complete exposure of the nerve. Extending the TL approach (particular anteriorly) and combining it with additional approaches allow its use for lesions extending to additional anatomical areas.
The TL approach should not be used in an infected ear. Small mastoids create a surgical challenge by hindering access to the depth of the cavity. Whether an alternative surgical approach is indicated in this situation depends on the size and location of the tumor and the preference of the surgeon.
8.2.1 Vestibular Schwannomas: Epidemiology, Presentation, and Diagnosis
The most commonly used indication for applying the TL approach is the removal of vestibular schwannomas (VS). VS are benign tumors originating from one of the vestibular branches of cranial nerve VIII. The clinical presentation of a cochlear nerve schwannoma is typically indistinguishable from the presentation of a VS, so they can be discussed in unity. Patients commonly complain of hearing loss, tinnitus (in up to 70 % of patients [4]), or both. Vestibular symptoms are more often related to imbalance and instability rather than vertigo, most probably as a result of the slow-growing nature of these tumors. Symptoms related to the trigeminal nerve may appear as the tumor grows. Motor facial nerve function is rarely compromised by VS, although hypoesthesia may be present in the external auditory canal region supplied by the facial nerve (Hitselberger sign) [5]. Tumor growth may damage the lower cranial nerves and cerebellum, ultimately leading to respiratory distress and death (rarely seen today). Heightened alertness to the possible diagnosis of VS and the widespread availability of hearing tests and imaging most likely contribute to the reported decrease in the average size of tumors at presentation [6]. Consequently, patients present with milder symptoms; symptoms attributed to brain compression and mortality risk are rare.
VS also can present sporadically or infrequently as part of neurofibromatosis type II. The TL approach can be used effectively for both tumor types. The gold standard for the diagnosis of IAC and CPA tumors is paramagnetic-enhanced MRI of the region. The incidence of VS varies significantly between reports, most likely because of the disparity in rates of gadolinium-enhanced MRI surveillance. The increased use of MRI contributes to the increase in the incidence of tumor detection. The incidence is 13:1,000,000 new cases per year in the United States [7] and 19:1,000,000 new cases per year in Denmark [8].
8.2.2 The Place of the TL Approach in VS Treatment
Current treatment options for sporadic VS are “watchful waiting” or “watch and scan,” low-dose stereotactic radiation, and surgical resection. There is an ongoing debate regarding the relative role of each option. The age of the patient, tumor size, and residual hearing are the principal factors influencing treatment choice. There is good evidence that a substantial portion of small tumors tend to remain stable in size, so watchful waiting with serial MRIs can verify the stability in tumor size and is often the best choice for patients (especially middle-aged or elderly) with small, nongrowing tumors. The use of aspirin was found to be associated with reduced rates of tumor growth [9]. The natural history of VS results in many patients losing serviceable hearing. Pressure on the auditory nerve, compromise of blood supply to the cochlea, and toxic effect on the inner ear are the main mechanisms thought to deteriorate hearing. However, both stereotactic radiation [10] and surgery also pose real risks to hearing. The goal of stereotactic radiation is to prevent tumor growth, and this goal is achieved in the vast majority of patients, with excellent rates of preservation of facial nerve function. Nevertheless, radiation is best offered as a treatment option only for patients with proven growth of tumors. Watchful waiting can be an appropriate choice for patients with minimal or no symptoms, poor health status, or advanced age [11].
Candidates for surgery are treated with one of three main surgical approaches: the middle fossa, the suboccipital, or the TL approach [12]. The first two options are suitable when the goal is hearing preservation—that is, in patients with serviceable hearing in the operated ear or when it remains the only functioning ear. Tumor size, tumor location, the pattern of preoperative auditory brainstem responses, and the results of behavioral audiograms are the main prognostic factors for the chance to preserve hearing with surgical extirpation of a VS. Resection of tumors larger than 2.5 cm and tumors involving the inner ear are associated with poor prognosis for hearing preservation, and the TL approach may be applied even when preoperative hearing is serviceable. There is no accepted definition of the level of hearing requiring hearing preservation techniques; in most cases, it varies between classes A and B according to the American Academy of Otolaryngology and Head and Neck Surgery [13]. Serviceable hearing defined by the class B and House Ear Institute’s 50/50 rule (threshold ≤50 dB and word recognition scores [WRS] >50 %) has gained popularity, although the class A definition (30 dB, 70 % WRS) is used by others [14].
8.3 Surgical Technique: Translabyrinthine Approach for Resection of Vestibular Schwannoma
8.3.1 Perioperative Preparation in the Operating Room
The patient is placed in the routine supine position for ear surgery, with the surgeon seated beside him or her. The head is mildly hyperextended and rotated to the contralateral side from the surgeon, on a suitable head rest. Shaving of the postauricular scalp and some of the temporal scalp is recommended. Broad-spectrum prophylactic antibiotics are administered intravenously an hour prior to the beginning of surgery and are usually continued at least 24 h postoperatively. Antibiotics may also be used in the irrigation solution.
Hyperventilation usually is sufficient for brain relaxation. If needed, mannitol can be used as well. Electromyography (EMG) electrodes for intraoperative facial nerve monitoring are inserted into the orbicularis oris and oculi muscles. Anesthesia is adjusted accordingly, avoiding paralytic agents past the first 30 min of the procedure. The skin is sterilized using regular skin preparations. There is no need to avoid ototoxic agents (such as alcohol-based solutions), as inner function is sacrificed and no connection is present between the middle and inner ears and the solutions. A site in the left lower abdomen for harvesting a subcutaneous abdominal fat graft is prepared and draped.
8.3.2 Soft-Tissue Incisions and Flaps
Prior to making the incision, the skin and subcutaneous tissues are injected with a local anesthetic, 1 % lidocaine with 1:100,000 epinephrine.
The retroauricular C-shape skin incision extends from the area of the mastoid tip to the temporal skin above the auricle, passing 3–4 cm posterior to the postauricular sulcus. The incision should allow unhindered access to the mastoid tip, the cortex, the area posterior to the sigmoid sinus, and the middle fossa dura. In addition, sufficient anterior rotation of the auricle is needed for proper exposure.
Soft-tissue, muscle, and periosteal flaps over the mastoid cortex and adjacent occipital bone are fashioned and elevated, and self-retaining retractors are used to expose the bone. These flaps should be elevated widely for unrestricted access to the CPA, allowing for a large amount of bone to be removed and allowing for the placement of a titanium mesh during the closing stages of the procedure. Retraction of the muscle and periosteal flaps is performed gently to avoid excess pressure, because stretching the flaps, applying pressure on them, or puncturing them can damage their integrity.
8.3.3 A Wide Mastoidectomy (Canal Wall-Up or Canal Wall-Down)
The TL approach can be effectively performed via either a canal wall-up (CWU) or a canal wall-down (CWD) mastoidectomy. The advantage for the latter is a potentially more robust seal preventing CSF leakage and the slightly wider angle of anterior access achieved by the removal of the external auditory canal (EAC). The advantage of the CWU mastoidectomy is avoiding the need for blind sac closure of the EAC and total removal of the canal skin and tympanic membrane, with the associated remote risk of an iatrogenic cholesteatoma. Our preference for most patients is the CWD procedure, but others routinely and successfully use the CWU approach, as depicted in the accompanying images.
The CWD procedure involves blind sac closure of the EAC. The EAC is entered posteriorly at the bone-cartilage junction and amputated. If needed, two incisions are performed, longitudinal to the cartilaginous canal at 6 and 12 o’clock. The skin of the cartilaginous framework of the canal is elevated. Anterior and posterior skin flaps are rotated laterally and sutured outside the meatus of the EAC with eversion of their edges. This blind sac closure must be hermetically sealed. Sutures can be added at the superior and inferior aspects of the everted skin as needed. The skin closure is reinforced medially by a soft-tissue flap rotated and sutured to support the amputated canal.
The cortex overlying the mastoid and the adjacent dura of the middle fossa and the sigmoid sinus is removed. Bone and air cells are exenterated posteriorly to the sigmoid sinus, as retraction of the sinus will be needed. The sigmoid sinus is widely exposed. An oval island of bone overlying the central section of the exposed sigmoid sinus, termed Bill’s island (after Dr. William House), may be left to protect the sinus wall from abrasion of the drill shaft while more medially placed structures are dissected (Fig. 8.1). Finally, the sinus is followed all the way to the bulb. Bone is left overlying the bulb, as the wall of the bulb is more delicate than the wall of the sinus itself. Superiorly, the dura of the middle fossa is followed medially until the antrum is opened and the incus and lateral semicircular canal are identified.
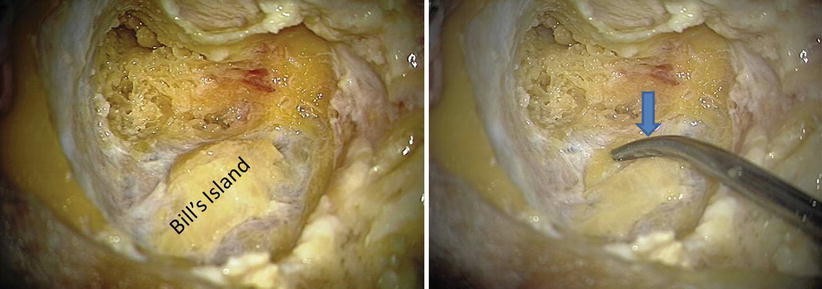
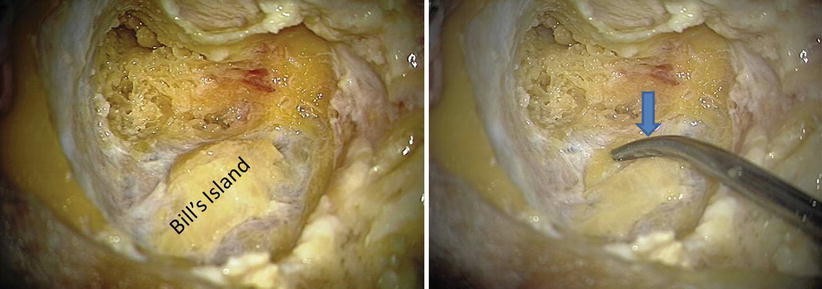
Fig. 8.1
Mastoidectomy and Bill’s bar. An extensive canal wall-up mastoidectomy with decompression of the dura of the middle and posterior fossa has been completed. An island of bone overlying the sigmoid sinus was left (Bill’s island). As it detached from the surrounding bone, it is easily compressible (arrow)
All bone adjacent to the fallopian canal of the mastoid segment of cranial nerve VII is removed. The facial nerve is defined throughout its mastoid segment, including the stylomastoid foramina (Fig. 8.2).
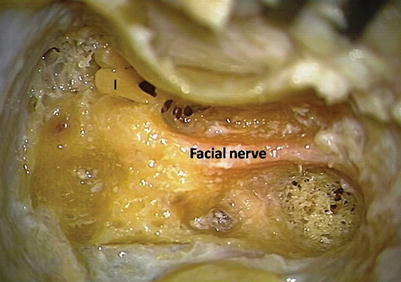
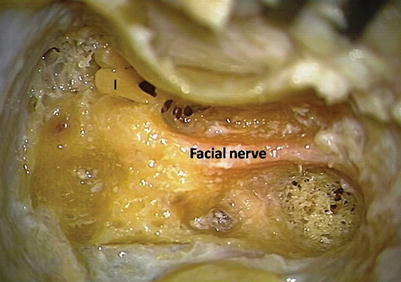
Fig. 8.2
The facial nerve. The complete tympanic and mastoid segments of the facial nerve are defined. An extended facial recess is opened
8.3.4 Removing All Bone over the Posterior and Middle Fossa Dura
The dura of the middle fossa and the posterior fossa must be devoid of all bone coverage. A large cutting burr is used to exenterate all air cells and bone until a thin layer of bone remains overlying the dura. Subsequently, a large diamond burr is used to remove all covering bone. Even a small amount of bone left will limit retraction of the dura and will restrict sight and access to the IAC and CPA. Special attention is paid to the sinodural angle. Removing the spine of bone at the angle requires smaller diamond burrs in order to avoid injury to the underlying superior petrosal sinus.
8.3.5 Systematic Labyrinthectomy
The labyrinth is exenterated systematically. First, the lateral canal is opened and followed from its midportion to its ends (Fig. 8.3). The ampullary side of the lateral canal lies in close proximity medial to the facial nerve, and drilling at this point with the side of the burr may easily damage the nerve. Next, the posterior canal is opened and followed to the common crus (Fig. 8.4). The superior canal is met and followed from its nonampullary side to the ampullary end (Figs. 8.5 and 8.6). Resection of the posterior canal takes into account the proximity to the jugular bulb located inferior to the ampulla of the posterior canal. Dissection proceeds inferiorly, using a diamond burr, until the jugular bulb is defined. The cochlear duct is used as a limit to the dissection because the lower cranial nerves neighbor it closely. The three ampullae lie in close proximity to the vestibule. Immediately medial to the vestibule is the fundus of the IAC.




Fig. 8.3
Lateral semicircular canal (LSCC). Systematic labyrinthectomy begins with the definition of the vestibular otic capsule and the opening of the lateral semicircular canal

Fig. 8.4
Posterior semicircular canal (PSCC). After opening the LSCC, the PSCC is opened (arrow)

Fig. 8.5
Superior semicircular canal (SSCC). The SCC is defined (arrows). The ampullary side of the LSCC lies in close proximity to the facial nerve (asterisk)










