The Osnabrueck Experience with Reconstruction of the Partial Mastectomy Defect
Klaus E. Brunnert
Oncologic Considerations
The traditional paradigm of breast cancer treatment to cure the disease with the help of radical local therapy has changed due to the fact that aggressive surgical methods have not succeeded in improving overall survival. Randomized clinical trials regarding certain clinical and histologic parameters show that breast-conserving therapy (BCT) has identical overall survival results. Patients have to be informed about this opportunity. The aim of surgical therapy is the complete removal of the cancer with clear margins, and it is up to the patient to decide whether to choose BCT or modified radical mastectomy (MRM). In the case of BCT, local radiotherapy of the breast has to follow to reduce the incidence of local recurrence.
The threshold for indication of adjuvant systemic therapy as endocrine, anti-HER2, or cytotoxic therapy depends on three factors: endocrine responsiveness, the overexpression or amplification of HER2, and the risk of recurrent disease. According to the St. Gallen Consensus Conference 2009, judgments must be made in the case of individual patients of whether to use or withhold each treatment modality. Only under certain favorable circumstances, such as ductal carcinoma in situ (DCIS) or invasive cancer with a very low risk of recurrence as tumor size <1 cm, without axillary nodal involvement and other features indicating increased metastatic potential, local therapy alone is sufficient in curing the disease. However, if such a low-risk cancer is endocrine responsive, endocrine therapy should be considered.
Due to the increased importance of systemic therapies in comparison to local surgical treatment modalities, especially in cases of further-advanced primary breast cancer with a higher-risk situation, survival will depend more on systemic adjuvant therapy than on local aggressive surgical treatment. As a consequence, the option of BCT and oncoplastic surgery plays a major role in the local treatment of breast cancer. In addition, primary chemotherapy has enlarged the conservative options if the tumor is already locally advanced and shows a good chemosensibility. The National Surgical Adjuvant Breast and Bowel Project B-18 study demonstrated a significant increase in BCT by 8% due to primary chemotherapy, especially in large tumors, >5 cm. By applying new dose-dense and sequential chemotherapy regimens, the rate of pathologic complete remissions (pCR) can be increased, a very promising finding given that pCR correlates with improved overall patient survival. The most important predictive marker for response is no evidence of endocrine responsiveness. In this group of patients, pCR up to 40% could be achieved. A resection in the new limits of the tumor is an option as long as free margins can be achieved. Thus primary chemotherapy is today the standard of care in patients with locally advanced, nonoperable, or inflammatory primary breast cancer and an alternative treatment option for patients with an indication for mastectomy who would prefer BCT.
A possible conflict between the goal to achieve the optimal result by oncoplastic and surgical procedures and the necessity for the highest degree of oncologic safety might arise due to the fact that in any case postoperative local radiotherapy will reduce local recurrence even if the benefit is a small one. The value of this benefit might be viewed in a different way by surgeons and radiotherapists and be taken into consideration in planning (e.g., a skin-sparing mastectomy with immediate reconstruction). If the risk of local recurrence is high in the case of invasive cancer, there is good evidence that local radiotherapy will improve overall survival by 4:1, that is, 1 life saved due to prevention of 4 local recurrences.
Breast-Conserving Therapy As the Standard of Surgical Care in Primary Breast Cancer
Breast-conserving therapy has become worldwide the new standard therapy for local treatment, and the cure of the systemic disease depends on additional systemic treatment. About 70% of primary breast cancers can be treated in a conservative way. In about 30% of the cases a mastectomy is necessary, either as a modified radical procedure, with or without reconstruction, or as a skin-sparing mastectomy (SSM) with immediate reconstruction. Performing SSM conservation of the nipple-areola complex (NAC) is possible under certain conditions: tumor site in the periphery of the breast, absence of extensive intraductal component, and negative frozen section behind NAC intraoperatively. Both procedures, SSM and nipple-sparing mastectomy (NSM), are as oncologically safe as MRM. Last but not least and the most important factor is the patient’s wish: It is up to the patient to decide whether to perform BCT or a mastectomy with or without a breast reconstruction.
The limitations concerning BCT are as follows:
An unfavorable tumor/breast size ratio.
Hyperplasia of the breast due to possible problems administering prophylactic radiotherapy. In this case lumpectomy and bilateral reduction mammaplasty are advisable.
The location of the tumor and its adherence to neighboring structures such as the overlying skin or the chest wall.
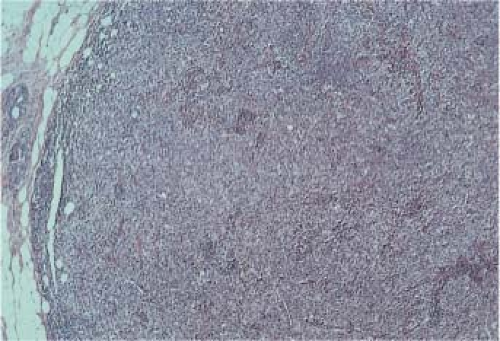
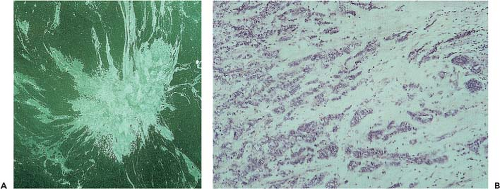
The growth pattern of the tumor, including a disseminated growth and multifocality, that is, lobular type of breast cancer (Figs. 14.1 and 14.2).
Extensive areas if DCIS is in the neighborhood of an invasive tumor.
Contraindications
Residual tumor despite repeated resection.
Inflammatory breast cancer.
Radiation therapy not possible.
Patient’s choice not to undergo procedure.
The main aims of BCT are as follows:
To reduce the surgical impact on the patient.
To preserve a natural, good-looking breast.
To provide efficient local treatment in regard to local control. Free margins and prophylactic radiation therapy will guarantee the best possible success.
Psychological Aspects
The loss of a breast due to cancer treatment has a devastating impact on the psychological welfare of most patients. Severe deformities after BCT or mastectomy can be seen as losing one’s feminine attributes and may result in profound alterations of the patient’s mental health and sex life. The loss of self-confidence may disrupt the ability to live a normal life and may permanently remind the patient of the deadly threat of the disease. In addition, functional impairments due to asymmetry, scaring, and resulting pain or hypersensitivity of the surgically treated area may occur.
With the choice between different treatment options after a primary breast cancer has been diagnosed, the need for individualizing and establishing a treatment plan suitable for each patient has arisen. This means that the surgical oncologist responsible for the treatment has to share his or her knowledge with the patient in order to reach informed consent. According to our experience, the best medical facility in which to achieve this is a comprehensive breast center, where the patient is able to contact different specialists and other patients with the same history of disease and treatment. Studies showed that patients and their husbands had lower levels of anxiety and depression when offered the opportunity to have a choice of treatment, even though it was sometimes difficult to make a decision.
Surgical Management to Improve Breast-Conserving Therapy
To achieve a rate of about 70% BCT and a good and natural aesthetic result, additional surgical procedures besides lumpectomy, derived from plastic surgery of benign breast disorders, have to be applied. In our experience and including primary chemotherapy, 70% of our primary breast cancer patients could be treated by BCT. Eighty percent of the BCT patients had a lumpectomy only, with or without an internal mastopexy; 11% needed additional flap surgery, mostly with a latissimus dorsi flap, and another 9% underwent a reshaping of the breast using a skin reduction pattern. That means that 20% of our BCT patients would have needed a mastectomy if additional surgical techniques had not been applied.
Role of Radiotherapy
Radiotherapy is an integral part of BCT. In order to achieve an optimal aesthetic result and to avoid reoperations due to
resulting breast deformities, it is vital to apply the necessary additional and prophylactic radiotherapy after the surgical procedures have been completed, not before. In the experience of our and other breast units, preoperative radiotherapy often proved to be detrimental to the final aesthetic result due to fibrotic changes and the impairment of the healing capacities of radiated tissue.
resulting breast deformities, it is vital to apply the necessary additional and prophylactic radiotherapy after the surgical procedures have been completed, not before. In the experience of our and other breast units, preoperative radiotherapy often proved to be detrimental to the final aesthetic result due to fibrotic changes and the impairment of the healing capacities of radiated tissue.
Methods of Closing the Partial Mastectomy Defect
How to close a lumpectomy or partial mastectomy defect depends on the amount of breast tissue resected and the amount of the remaining tissue. The margins between these two different types of volume are not precisely determined, and there is no way to define the border between BCT and the need for a total mastectomy by means of tumor size or a specific localization like a central tumor. An example of a central tumor is Paget’s disease of the nipple. In this case the resection of the nipple with a good portion of underlying gland and clear margins plus additional prophylactic radiation therapy may still represent an aesthetically pleasing example of BCT without the need for a total mastectomy.
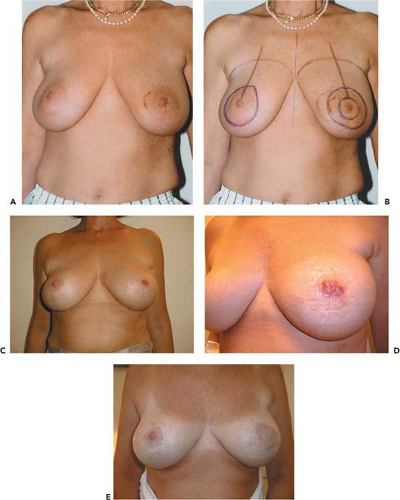
Case 1
A 50-year-old patient had a primary breast cancer of the left breast lower inner quadrant, pT2 G2 pTis G3 ERPR–HER2+++ pN0 pM0 2, years prior. A BCT using a bilateral reduction mammaplasty with radiotherapy was performed in our unit. The recommended adjuvant chemotherapy was refused by the patient. In the year 2000, the patient was diagnosed with Paget’s disease of the left NAC, 2.5 cm in size. The NAC was removed in combination with a wide resection of the underlying gland. Free margins were larger than 2 cm. The defect was closed with local tissue and covered with a skin transplant from the upper inner thigh. The patient is currently, in 2010, free of disease, with the latest follow-up photograph taken in 2004 (see Case 1 figure, A to E).
Due to reshaping methods of the gland and the possibility of additional flap surgery where it is needed, there is a wide range of different and individual options for achieving BCT even under unfavorable conditions. Therefore, there is a fluid transition between a simple lumpectomy and a mastectomy, and the different options for closure are determined by the available local or distant tissue. However, no definite surgical decision with irreversible major consequences should be made based on intraoperative frozen section only due to the fact that the definition of a free margin defined by frozen section may be inaccurate.
Excision of A Small Breast Mass (Lumpectomy)
At the time of surgery the diagnosis of an occult or palpable DCIS or invasive cancer should already been made via core or vacuum biopsy. For accurate preoperative treatment planning, breast imaging with the description of the most likely extension of neoplasia is important. To accomplish the goal of free surgical margins, intraoperative use of ultrasound, specimen radiology, and sometimes frozen section in selected areas of the excised specimen are helpful.
First step: If a sentinel node biopsy is indicated, preoperative marking with technetium is executed in most of the cases. A subcutaneous and peritumoral injection of 5 mL of blue dye might help in special cases. Guided by technetium and/or the dye, a separate incision in the axilla is made and the sentinel node is sent for frozen section, so the axillary clearance can be performed during the same procedure if necessary.
Second step: The vicinity of the tumor and the base of the breast are infiltrated with epinephrine 1:200,000. For lumpectomy, the skin incision follows the Langer lines directly above the tumor. This gives the surgeon direct access to the tumor area without tunneling. For tumors close to the NAC, a periareolar incision will be made. On the lower breast, a half radial incisions may be chosen under certain conditions. In general, the subdermal layer of fat must be preserved to prevent an unfavorable dimple. If this is not possible due to local conditions, this layer of fat has to be replaced.
Third step: The excision of the tumor is always performed with the least possible amount of trauma on the mass itself. The tumor area is separated from the surrounding tissue by blunt dissection if possible, using a pair of Lexer scissors, touching the specimen with the fingertips only, without the use of a clamp, leaving a sufficient margin of healthy tissue on the tumor. The use of an ultrasound device might help to preserve this margin of tissue. Electrocautery should be avoided at this stage and used for hemostasis only, to prevent thermal injury to the specimen. The excised specimen has to be marked with sutures for orientation or inked due to recognized local protocol to enable an accurate reexcision of tissue if necessary. An additional drawing integrating the tumor may be helpful for communicating with the pathologist.
The resulting defect can be closed just by suturing the subdermal layer and the skin itself if the breast is full and large and the walls of the resulting cavity collapse on their own. If this is not the case and to prevent a palpable or even visible defect, that is, in case of a firm breast tissue without fat, a few sutures can close or loosely adapt the walls of the cavity if necessary and prevent deformity. In general, hemostasis should be sufficient so no drains are necessary.
If the tumor area is situated close to the axilla, the same incision may be chosen for the excision of the sentinel node or the axillary clearance. In this case, a running suture should close the axilla after the clearance. The axillary clearance itself should include levels 1 and 2 but should not be performed as an en bloc resection. On the contrary, vessels and nerves should be preserved by removing the lymph nodes one by one together with some additional fat around them. Larger lymph vessels should be sealed by cautery if they have to be cut.
Excision of A Larger Breast Mass
This may follow the surgical technique described previously. To close the rather large defect, a so-called internal mastopexy is necessary. The breast tissue adjacent to the defect has to be mobilized, brought into the defect, and closed by interrupted sutures. This procedure probably has the same effect as a mastopexy, so asymmetry may occur.
Lumpectomy Using A Periareolar Access
In smaller, ptotic breasts with larger tumors lumpectomy using periareolar access may be useful. In this case the surgeon is able to expose the whole gland by circular dissection as when performing a periareolar reduction or mastopexy. In this way there is excellent access to the whole gland, and a wide excision can be made together with a whole segment of breast tissue, and the defect is easily closed again resulting in a simultaneous lifting. The axillary clearance can be performed using the same incision.
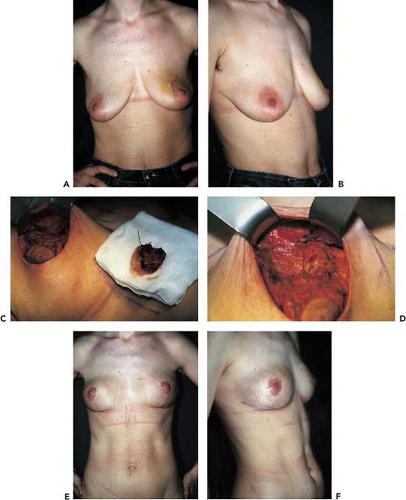
Case 2
A 39-year-old patient with an invasive ductal carcinoma on the left side was treated via an incomplete resection externally.
Reexcision was necessary immediately and was performed in our unit via a periareolar approach to have better access to the pretreated tumor area. Due to the individual extension of the tumor growth close to the skin, a radial skin ellipse was excised (tumor staging: pT2 pN1 pM0). On the right breast, a benign tumor was excised at the same time and a mastopexy performed due to a mild ptosis and to prevent asymmetry. The postoperative views were taken after 1 week (see Case 2 figure, A to F).
Reexcision was necessary immediately and was performed in our unit via a periareolar approach to have better access to the pretreated tumor area. Due to the individual extension of the tumor growth close to the skin, a radial skin ellipse was excised (tumor staging: pT2 pN1 pM0). On the right breast, a benign tumor was excised at the same time and a mastopexy performed due to a mild ptosis and to prevent asymmetry. The postoperative views were taken after 1 week (see Case 2 figure, A to F).
Excision of A Skin Ellipse
If the breast mass is close to the skin, a skin ellipse above the tumor has to be excised. Whether this will result in a deformity or asymmetry depends on the width of the ellipse needed, the laxity of the skin, and the localization (e.g., the excision of a horizontally orientated skin ellipse below the nipple will reduce the distance between NAC and the submammary fold).
However, a vertical incision in this area will probably reduce the width of the breast. Whether this is acceptable has to be considered on an individual basis. Before the surgeon takes the risk of causing a deformity, additional flap surgery or reshaping of the breast should be considered.
However, a vertical incision in this area will probably reduce the width of the breast. Whether this is acceptable has to be considered on an individual basis. Before the surgeon takes the risk of causing a deformity, additional flap surgery or reshaping of the breast should be considered.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree