One-Stage Immediate Breast Reconstruction with Adjustable Implants
Hilton Becker
Introduction
Although autologous tissue is ideal for breast reconstruction, the magnitude of the surgery, the length of recovery, potential complications, and the resultant scarring are of concern to many patients. In addition, if radiation is anticipated following immediate reconstruction, an expander should be placed initially in order to avoid radiation to the flap. Autologous reconstruction can still be performed following radiation by placing a de-epithelialized flap in the expander pocket.
The increased awareness of the risk factors and the availability of genetic testing have increased the incidence of bilateral mastectomies being performed on younger women. These patients are eager to have immediate reconstruction with minimal scarring and minimal downtime. Many of these patients are already dissatisfied with their breasts and may have, or are considering, breast implants. For these patients, a one-stage implant reconstruction with minimal or no visible scarring, with the opportunity to correct prior hypomastia or ptosis with minimal surgical time and downtime, is often preferable to autologous flaps.
The one-stage reconstruction technique involves the following.
Mastectomy performed using the skin-sparing technique
Muscle release and inframammary fold reconstruction
Use of adjustable implants
Technique
Preoperative planning is done in concert with the general surgeon who will be performing the mastectomy. Inframammary folds are marked, and the topics of extent of skin resection and feasibility of nipple-areolar or skin preservation are discussed.
Mastectomy Performed Using the Skin-Sparing Technique
It is advantageous for the plastic surgeon to assist the general surgeon, at least initially, with the mastectomy. The general surgeon’s awareness of the reconstructive procedure is key to obtaining an excellent result. The skin-sparing mastectomy is performed by the general surgeon, who is encouraged to use plastic surgery principles. Fiber-optic lighting is used to facilitate dissection. Care is taken to avoid trauma to the skin flaps. If necessary, a medial and lateral extension can be made to the circular incision for better exposure, or a separate incision can be made in the axilla for axillary dissection. Both incisions are easily concealed.
Keeping the option open to maintaining the nipple-areolar complex or the areolar skin, preserving the fascia, avoiding any damage to the muscle, maintaining the inframammary fold, and maintaining viable skin flaps are keys to facilitating an optimal reconstruction (Figs. 30.1 to 30.4).
Muscle Release and Inframammary Fold
After the general surgeon has completed the mastectomy, the drapes are changed and hemostasis checked. The integrity of the muscle and inframammary fold is then assessed. If the muscle and fold are totally intact, a similar technique to submuscular breast augmentation is possible. A subpectoral-serratus anterior muscular pocket is dissected, starting at the lateral border of the pectoralis major muscle. Dissection continues approximately 2 cm below the inframammary fold. The muscle fibers and rectus fascia are incised at this level. The inframammary fold is enhanced, while the pectoralis remains attached to the fascia above the releasing incision.
As the muscle is intact and attached, no fixation sutures or dermal grafts are necessary (Figs. 30.5 and 30.6).
If the decision is made to detach the pectoralis muscle, two options are available: (a) elevation of the pectoralis and serratus muscle and (b) elevation of the pectoralis major only. For elevation of the pectoralis and serratus muscle, the two muscles are sutured together. Fixation will be necessary to prevent retraction of the muscle. Fixation may be done with:
Mesh (Fig. 30.8)
Autologous dermis
For elevation of the pectoralis major only, fixation is accomplished with acellular dermis, both inferiorly and laterally (Fig. 30.9B). Dissection begins at the lateral border of the pectoralis major muscle. The muscle is elevated and detached inferiorly at its insertion. It is also partially detached medially. The serratus anterior muscle is elevated laterally and detached inferiorly at the level of the inferior margin of the pectoralis major. The two muscles are then sutured together with interrupted sutures, thus expanding the submuscular pocket (Fig. 30.10).
As an alternative to acellular dermis, an autologous dermal graft may be used. If the muscle is damaged or partially removed, an acellular dermal graft is invaluable in augmenting and strengthening the muscle (see Fig. 30.4). An intraoperative expander is placed beneath the muscle and partially expanded to assess the size and position. The inferior edge of the muscle or the dermal graft is then sutured to the fascia at the level of the inframammary fold. A deliberate space of 0.5 to 1 cm is left between the inferior edge of the dermal graft and the inframammary fold. This space allows the lower pole to expand differentially, resulting in a more anatomic pocket. Several sutures of 2/0 Vicryl are placed from the muscle edge to the fascia for added security. If the fascia has been removed or the muscle is damaged or atrophic, the muscle is fully released and then reinforced with acellular dermal grafts.
Acellular dermal grafts are rapidly vascularized when placed in contact with muscle. However, revascularization has been
noted to be slower when the graft is placed over the implant posteriorly and in contact with subdermal fat anteriorly, especially if the patient has had prior radiation. Therefore, in order to facilitate revascularization, the use of thinner grafts is preferred. Meshing dermal grafts using a 1:1 graft has also been found to be beneficial. Wherever possible, the skin closure should be over muscle rather than over dermal graft.
noted to be slower when the graft is placed over the implant posteriorly and in contact with subdermal fat anteriorly, especially if the patient has had prior radiation. Therefore, in order to facilitate revascularization, the use of thinner grafts is preferred. Meshing dermal grafts using a 1:1 graft has also been found to be beneficial. Wherever possible, the skin closure should be over muscle rather than over dermal graft.
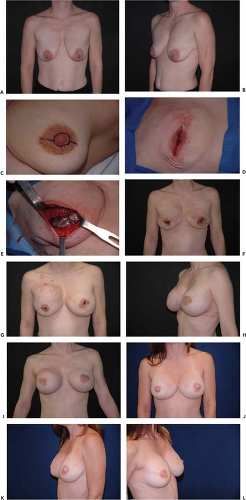
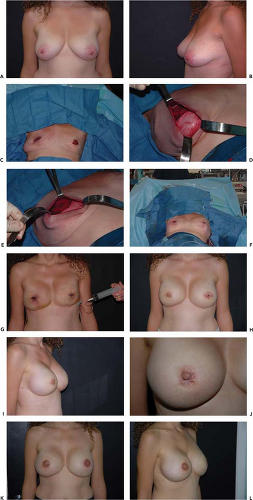 Figure 30.2. A: Preoperative anterior view of a patient for bilateral skin-sparing mastectomies. B: Preoperative lateral view. C: Postoperative view following bilateral skin-sparing mastectomy. D: Acellular dermal graft sutured to the inferior edge of the pectoralis major muscle. E: Adjustable implant placed beneath the muscle-dermal graft flap. F: Purse-string closure following immediate reconstruction. G: Saline added via external filling dome once circulation is assured. H: Final result following injection dome removal and nipple reconstruction. I: Final result, lateral view. J: Final result; close-up view, no visible scar. K, L: Final result following areolar tattoo.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|