The orbicularis retaining ligament is the structure responsible for defining the palpebromalar groove and is a key structure in the appearance of aging of the midface. A major anatomic basis for the appearance of festoons seems to be the downward descent of tissues superior to a lax orbicularis retaining ligament and orbicularis muscle against the resistance of the stronger lower border. The focus of treating festoons involves addressing the laxity of the orbicularis retaining ligament along with redistribution of muscle, skin, and fat within the lid-cheek junction. Surgical approaches involve direct excision of the affected tissue or indirect redraping of the affected soft tissue.
Key points
- •
The orbicularis retaining ligament (ORL) is the structure responsible for defining the palpebromalar groove and is a key structure in the appearance of aging of the midface.
- •
A major anatomic basis for the appearance of festoons seems to be the downward descent of tissues superior to a lax ORL and orbicularis muscle against the resistance of the stronger lower border, effectively creating a surface trough.
- •
The focus of treating festoons involves addressing the laxity of the ORL along with redistribution of muscle, skin, and fat within the lid-cheek junction to re-establish a smooth and youthful contour.
- •
Historically, surgical technique addressed maximizing excision of the skin-muscle responsible for the visible appearance of the festoons; currently, surgical approaches involve direct excision of the affected tissue or indirect redraping of the affected soft tissue.
Introduction
Aging of the midface and lower lid complex can be evident even in the late 30s, making this one of the earliest detectable areas of facial aging and frequently requested sites for surgical rejuvenation. When present, malar festoons can complicate successful rejuvenation because they present a difficult problem to treat. Festoons occur when portions of the orbicularis oculi muscle attenuate, thereby undergoing a progressive course of sagging muscle that becomes visible to even the most casual observer. Beyond aesthetic concerns, severe festoons can cause visual field obscuration on downgaze, leading to difficulty with near-vision tasks. Although typically seen and referred to in the lower eyelid, because the orbicularis oculi encircles the eye, festoons can occur in the upper or lower eyelid. Because upper eyelid festooning is uncommon and the emphasis in the literature is on lower eyelid festoons, the latter are the focus of this article.
Although a genetic basis for the etiology of festoon formation is suspected, the precise reason why some individuals are susceptible to this condition whereas others are not is largely unknown. When present, festoons can impart the appearance of being excessively tired and when more severe can be deforming, resulting in issues of self-confidence. Every effort should, therefore, be made to improve the appearance of patients with this condition to enhance self-image and social well-being. Limitations in surgical correction are, however, a genuine challenge confounded by their unclear cause.
Anatomy
The midface is a complex anatomic area that separates the orbital cavity from the oral cavity. It is often defined as the area of the cheek medial to a line extending from the frontal zygoma to the oral commissure and the medial border defined by a line extending from the medial canthus to the nasolabial fold. The midcheek is composed of 2 functionally distinct parts :
- 1.
The prezygomatic part that overlies the midcheek skeleton
- 2.
The infrazygomatic part that covers the vestibule of the oral cavity
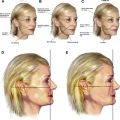
The prezygomatic area can be considered a transition zone where the skeletal attachments of the lower lid, including the ORL, are attached to the upper border of maxillary bone. The ORL (or malar septum) is the structure responsible for defining the palpebromalar groove; the junction between the preseptal portion of the lower lid and the cheek and is a key structure in the appearance of aging of the midface ( Fig. 1 ). The ligament acts as a functional and structural barrier defining the lower extent of several clinical entities, including malar mounds, malar edema, periorbital ecchymosis, and malar festoons.
Patients presenting for periorbital rejuvenation commonly complain of eyelid bags with a resulting tired look. The anatomic basis of eyelid bags is multifactorial, where orbital fat prolapse, eyelid fluid, tear trough depression, loss of skin elasticity, orbicularis prominence, and malar mounds and festoons can each contribute to their development. Correct diagnosis of the cause of eyelid bags is, therefore, critical when addressing this problem, with festoons one possible unique clinical entity among the possible causes.
A major anatomic basis for the appearance of festoons seems to be the downward descent of the tissues superior to a lax ORL and orbicularis muscle against the resistance of the stronger lower border, effectively creating a surface trough ( Fig. 2 ). The festoon phenomenon can affect any part of the upper or lower eyelid, with 5 distinct type of festoons described. They are divided bythe level of the orbicularis that they affect ( Figs. 3–5 ):
- 1.
Upper eyelid
- 2.
Pretarsal
- 3.
Preseptal
- 4.
Orbital
- 5.
Malar
The outward appearance of this process can differ among individuals and can range from the sagging of individual levels in a cascade of festoons with overlapping folds to the coalescence of layers together, sagging into a single festoon. When present in the malar region, a festoon is defined superiorly by the ORL over the previously described prezygomatic area and inferiorly by the stout zygomatico-cutaneous ligament, which is considerably stronger than the ORL. The ORL is also important because it is the inferior boundary of the inferior orbital fat compartment and provides an area of fixation against which the prolapse of fat can lead to the appearance of eyelid bags and be confused with malar festoons.
The focus of treating festoons involves addressing the laxity of the ORL along with redistribution of muscle, skin, and fat within the lid-cheek junction to re-establish a smooth and youthful contour.
Evaluation
Prior to surgical intervention, a full examination of the periorbital and malar contents and anatomy should be performed. Patients should be evaluated with the head in neutral position, while they are either standing or sitting upright in good lighting. Examination should occur initially with the eyes at neutral gaze followed by upward and downward gaze to evaluate for any vision obstruction.
During evaluation, as well as preoperative marking, the surgeon should manipulate the periorbital skin with fingers or forceps. This allows for proper diagnosis as to the level of orbicularis affected and the amount of tension in the skin. Pinching the festoon (the pinch test) allows a surgeon to judge the composition of the festoon (skin muscle or skin only) (see Fig. 2 ). A lower lid snap test should be performed as well to assure the integrity of the tarsoligamentous complex to determine if a canthoplasty is required. Finally, patients should also be instructed to squinch (the squinch test [ie, tightening and lifting the lower lid]) to determine the integrity of the orbicularis muscle and its relationship to the underlying orbital and suborbicularis fat as well as the laxity of the orbital septum. In cases of lax septum, orbital fat can be seen protruding anteriorly into a separate septal pouch. In these cases, a squinching motion causes orbicularis contraction, which elevates and compresses the fat back into the orbit. It can, therefore, be appreciated how correction of festoons will improve the lower eyelid, whereas correction of the lower eyelid alone will not correct the festoon.
Surgical procedure
Currently there is no standard treatment of effective management of malar festoons, a fact that reflects the difficulty and dissatisfaction with repair. Nonsurgical options, including radiofrequency thermoplasty, carbon dioxide laser resurfacing, trichloroacetic acid peels, and the use of dermal fillers, have been reported, all with mixed results. Historically, operations were designed with the intent of maximizing excision of the skin-muscle responsible for the visible appearance of the festoons. Currently, surgical approaches can be divided into techniques involving direct excision of the affected tissue versus indirect redraping of the affected soft tissue. These indirect redraping techniques have in common limited skin excision and aggressive tightening as opposed to excision of the lax orbicularis muscle to optimize results with variations on those themes reported.
Direct Excision
Excisional correction procedures have historically been used as a means of festoon correction as a result of the belief that the sagging of muscle resulted in excess muscle and skin that require removal for treatment.
- •
The procedure begins with a subciliary incision 2 to 3 mm below the lid line followed by creation of a split-level flap consisting of a skin-only flap laterally and a skin-muscle flap medially.
- •
The lateral skin-only flap is dissected from the orbicularis muscle until the pretarsal orbicularis is reached wherein elevation of the skin-muscle flap is begun using blunt dissection and proceeding downward with wide exposure of the orbital septum. Any identified excess fat is excised off the flaps during this dissection.
- •
Excision of a portion of the orbicularis muscle is then planned and designed to be perpendicular to the direction of the muscle fibers.
- •
The muscle is gathered and folded along the proposed myomectomy axis and the optimal pattern (rectangle, trapezoid, triangle, and so forth) is chosen for the myomectomy and marked.
- •
The muscle is excised layer by layer until only a thin layer of muscle fibers and posterior fascia remains. The remaining muscle and fascia act as a protective layer for the underlying facial nerve branches.
- •
The cut edges of the orbicularis muscle are then joined with simple and horizontal mattress sutures and the upper border of the orbicularis is anchored to the periosteum or deep fascia of the lateral canthus.
- •
Excess skin is excised next in the form of a wedge resection guided by the initial skin markings.
- •
A trial suture is placed subcutaneously to close the skin wedge, and the tautness of the lid and level of the lid margin are adjusted as necessary.
- •
The lateral wedge is resected and closure is completed with fine absorbable suture.
Indirect Redraping
More recent recognition of the effect that gravitational migration has on the formation of festoons and midface descent has resulted in a paradigm shift that has focused more on enhancing lower lid–cheek shape and contour rather than simple elevation and tissue removal. Where segmental myectomy and myorrhaphy of the orbicularis previously dominated treatment plans, now extensive dissection with aggressive redraping of the muscle and limited skin excision are key elements of surgical management and the preferred techniques of the senior authors (SB and SD). Variations of these techniques have been reported in the literature and are described.
The extensive dissection necessary to address festoons involves some form of subperiosteal midface lift to properly correct the gravitation descent of all involved structures while creating an aesthetically pleasing eyelid and midcheek unit.
- •
The redraping technique begin with a subciliary incision followed by creation of either a skin-only or skin-muscle flap. The senior authors’ preferred technique is use of a skin-only flap initially, with the amount of elevation based on how much skin excision is planned, followed by a skin-muscle flap.
- •
Once elevation to the level of the orbital rim is complete, an incision is made in the orbicularis oculi muscle lateral to the lateral canthal angle down to the level of the bone.
- •
A subperiosteal dissection is then carried inferiorly to at least the inferior border of the festoon and can extend to below and around the zygomaticofacial nerve and vascular complex.
- •
The ORL is released during this dissection and care is taken to avoid injury to the neurovascular bundle.
- •
Once the dissection is complete and mobility confirmed, redraping of the soft tissue is performed through a variety of techniques.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree