The Inframammary Fold: Histologic and Anatomic Description, Classification and Definitions, and Options for Repair and Reinforcement
Bradley P. Bengtson
The inframammary fold (IMF) is the keystone and most important foundational element of the breast. Prior to 2000, there was a great deal of time, attention, and body of research dedicated to the study of the IMF, and recently there has been resurgence in the recognition of its importance. This chapter presents and discusses the histology and anatomic nuances of the IMF, the terminology and classification of the deformities that may occur surrounding it, and a few techniques for recreating the fold if malposition occurs.
An excellent description of the superficial fascial system of the breast in this area appeared in a review by Nava et al. in a prior edition of this text (1). They described the fascial system of the breast and how it relates to the fold, and they further broke it down anatomically by contour, level, angle, and symmetry (see Fig. 43.1). Histologically, they showed in cross section how the superficial fascial fiber inserted in an oblique vertical position into the chest wall (see Fig. 43.2).
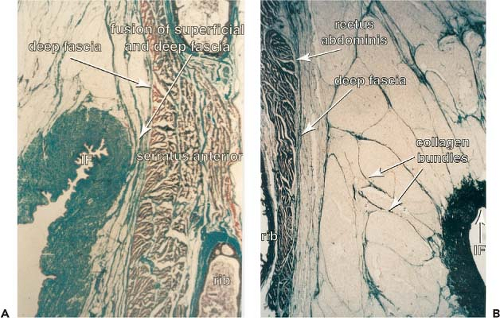
Further histologic and anatomic description is available from Acland’s group in Louisville (2) (Fig. 130.1). They showed in detail the region of the IMF and specifically how the fusion of the deep and superficial fascia insert in an oblique fashion from a vertical direction. Why is this important clinically? Every plastic surgeon who has performed a breast reduction with a transverse incision placed originally in the fold has seen the incision ride up to a higher location on the base of the breast postoperatively, particularly if the closure is tight. A similar effect occurs in breast augmentation. If this anatomy is not taken into consideration, an implant may shift down into the slot beneath this vertically oriented fascia, with the incision moving up into a higher location on the breast than originally planned. Furthermore, if these fascial fiber insertions are released either intentionally or unintentionally, the breast or implant can descend even further down onto the chest wall.
I define the IMF anatomically as a resting or sitting fold position and a true fold position where the actual base of the fold resides: where these superficial fascial fibers actually insert into the deeper fascia. This is a minimum of 1 cm, and may be up to 3 cm lower than where the visible, natural, resting skin fold junction is in relation to the chest wall (Figs. 130.2 to 130.5). The resting fold position may also be demonstrated by retracting the fascia of the breast and noting its attachments transmitted through the lower pole of the breast skin (Fig. 130.6). This can also be seen anatomically in every breast augmentation through an IMF incisional approach, and this is why the dissection after the skin incision is made should go directly at a vertical oblique angle of 60–80 deg to avoid disruption of the IMF, preserving the true fold position. In addition I prefer to leave a medial fascial shelf at this true or actual fold at the time of placing a partial submuscular implant, helping to maintain the final fold position in breast surgery. This aids to further support the device and avoid fold malposition (Fig. 130.7).
One further pearl relates to the ideal nipple to inframammary (N-IMF) distance based on certain styles, sizes, and volumes of breast implants. These principles are based on work by Tebbetts and Adams originally described in terms of the TEPID system (tissue characteristics of the breast, envelope, parenchyma, and implant and dimensions and dynamics of the implant relative to the soft tissues) and more recently the “high five” selection system (3,4). We expanded these concepts further and also defined a selector tool that simplifies this relationship and is based on more than 2,000 breast augmentations and measurements (5). For example, If the final implant volume is 300 cc, the N-IMF distance should be approximately 8 cm on maximum stretch. If the skin and tissues are tight, one should add 5 mm; if they are loose, one should subtract 5 mm. Then for each 50 cc one should add or subtract 5 mm, or 1 mm for each 10 cc. So a 400-cc implant should have an ideal fold of 9 cm with normal skin dynamics, and when one is using a 250-cc implant, the ideal N-IMF should be approximately 7.5 cm. This is extremely accurate and is important especially with a shift back to the inframammary incision and for gel devices, particularly future form-stable devices. This is even more critical when a patient has a constricted breast or high IMF. The plastic surgeon needs to be confident about where the new IMF should be set before placing an incision on the breast, and if planned and designed properly, the incision should be directly in or a few millimeters adjacent to the final IMF position (Fig. 130.8A, B). When moving the fold to a new planned or required location, further reinforcement by placing a 2-0 Vicryl from the deep fascia triangulating to the fascia of the upper portion of the incision is important (personal communication, Charles Randquist). This maneuver helps set the fold. It is a less common to lower the fold beyond the true or resting fold except in severely constricted breasts or in revisional breast surgery.
It is key to define and clarify what we are describing, at a minimum, so we can all be sure of speaking the same language. There are many terms and classifications when it comes to the anatomy of this area and subsequent types of deformities that may occur. My goal is not to convert others if they have a specific way to describe these terms, but to make sure that we are using the same semantics, or at least understand what the other person is talking about. The inframammary fold is a
well-agreed-upon structure. If an IMF incision is planned, the primary surgeon knows accurately where the fold is located and where ideally he or she wants the fold to be placed. The fold is also then measured on maximal stretch from the midnipple point to the fold (N-IMF). Some surgeons also take a measurement from the umbilicus as an additional fixed point of reference. The incision is made and is a reference point for the future. If an implant or breast tissue in the case of a reduction or mastopexy slips below this point with the incision riding up on the breast, by definition I would term this a fold malposition.
well-agreed-upon structure. If an IMF incision is planned, the primary surgeon knows accurately where the fold is located and where ideally he or she wants the fold to be placed. The fold is also then measured on maximal stretch from the midnipple point to the fold (N-IMF). Some surgeons also take a measurement from the umbilicus as an additional fixed point of reference. The incision is made and is a reference point for the future. If an implant or breast tissue in the case of a reduction or mastopexy slips below this point with the incision riding up on the breast, by definition I would term this a fold malposition.
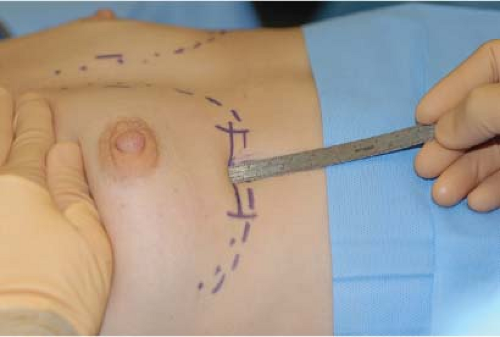 Figure 130.2. The resting fold in the sitting position. When the patient is upright, the breast fascial fibers insert into the skin in this position, creating the skin fold. |
 Figure 130.3. This image of the patient in Figure 130.2 shows the position of the true fold where the deeper fascial fibers insert into the chest wall. This position is usually 1 to 2 cm below the resting fold position.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|