BASICS
I. STRUCTURE
A. Tendons are strong, dense, uniform connective tissue structures that attach muscles to bones.
B. Consist of long collagen fibrils produced by specialized fibroblasts called tenocytes that are embedded in a matrix of proteoglycans.
1. Type 1 collagen → longitudinal bundles→ fibrils → fascicles → tendons
C. Endotenon
1. Composed of loose areolar tissues
2. Surrounds individual fascicles and supports blood vessels, lymph, and nerves
3. Continuous with the perimysium proximally and the periosteum distally
D. Tendons within synovial sheaths are surrounded by an outer fibrous layer called epitenon, while tendons found outside tendon sheaths are surrounded by loose connective tissue called paratenon.
E. Both epitenon and paratenon are highly cellular and vascular and are continuous with the endotenon.
F. The tendon sheath is a synovial-lined canal that originates from the periosteum and extends from the distal palmar crease to just beyond the distal interphalangeal (DIP) joint.
1. It provides synovial fluid for low-friction gliding.
2. In general, tendons that take sharp turns around joints (e.g., flexor digitorum superficialis [FDS], flexor digitorum profundus [FDP], and flexor pollicis longus [FPL]) are surrounded by synovial sheaths.
3. Tendons that move in straight lines (e.g., extensor carpi radialis longus [ECRL]) are surrounded by paratenon and are not contained within a sheath.
II. FLEXOR TENDON ANATOMY
A. The FDS, FDP, and FPL muscles provide flexion to the fingers and thumb
B. FDS, FPL (to the index and middle fingers), and FDP (to the ring and small fingers) are innervated by median nerve
C. FDP to the ring and small finger innervated by ulnar nerve
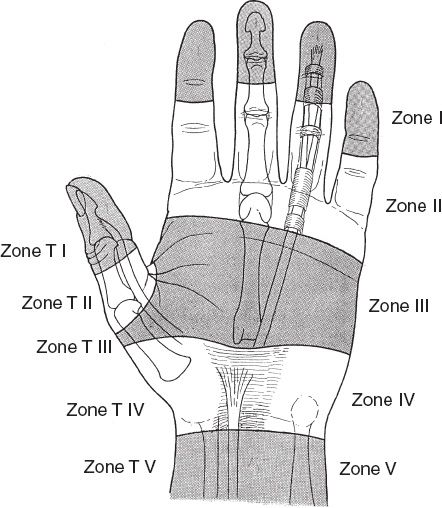
D. Flexor tendons are divided into five zones (Fig. 40-1)
E. The FDS flexes the proximal interphalangeal (PIP) joint
1. In the wrist, the FDS to the middle and ring fingers lie superficial to the small and index fingers
2. The tendon consists of two slips at the level of the metacarpal head
3. The slips travel dorsally and laterally around the FDP tendon and rejoin deep to the FDS tendon at Camper chiasm and insert as two slips on the volar surface of the middle phalanx
III. EXTENSOR TENDON ANATOMY
A. Innervated by radial nerve
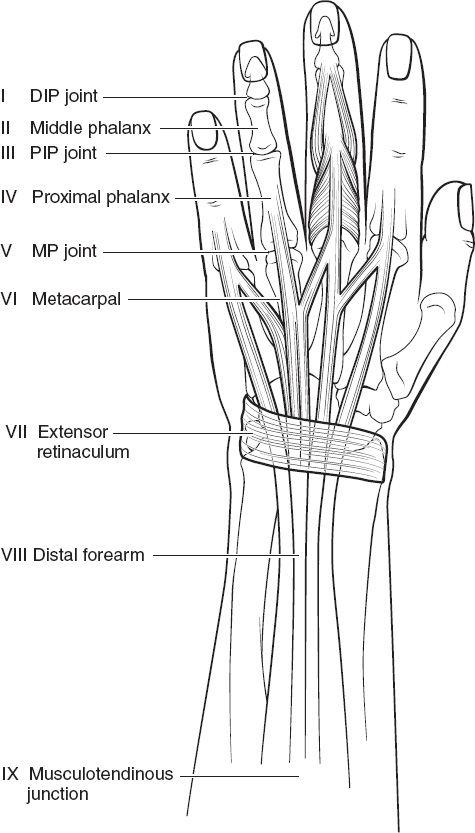
B. Extensor tendons consist of nine zones (Fig. 40-2)
______________
*Denotes common in-service examination topics
Figure 40-1. Flexor tendon zones. T, thumb.
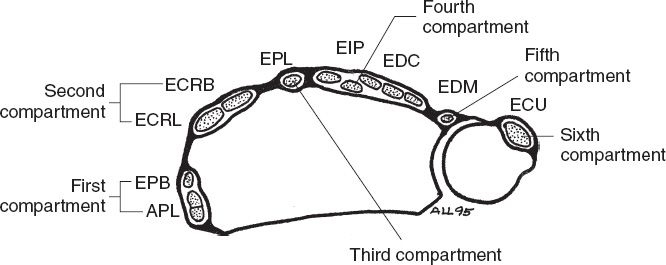
C. Under extensor retinaculum, the extensors are divided into six compartments (Fig. 40-3)
D. Juncturae tendinae
1. Variable fibrous cross-connections between extensor digitorum communis (EDC) tendons, arising and inserting on the dorsal surface of the hand just proximal to metacarpophalangeal (MP) joint.
2. Can lead to misdiagnosis of extensor tendon injury proximal to juncturae, given their ability to provide motion to adjacent tendons.
E. Intrinsics
1. Innervated by the ulnar nerve
2. Palmar interossei (3)
a. Adduct fingers, flex MP joints
b. Extend interphalangeal (IP) joints when MP joints are flexed
3. Dorsal interossei (4)
a. Abduct fingers, flex MP joints
b. Extend IP joints when MP joints are flexed
F. Extensor mechanism
1. Complex structure with contributions from EDC (plus extensor indicis proprius [EIP] and extensor digiti minimi [EDM]), lumbrical, and interosseus tendons.
2. The extensor digitorum (ED) expands over the MP joint to form the extensor hood, which then divides into the central slip (CS) and two lateral slips
a. CS inserts on the base of the middle phalanx to provide PIP extension
b. Lateral slips receive contributions from the lumbrical (L) and interossei (IO) to form the lateral bands (LBs), which continue distally to insert on the base of the distal phalanx as the terminal tendon to provide DIP extension.
c. LBs are stabilized dorsally over the middle phalanx by the triangular ligament (TL).
3. *Oblique retinacular ligament (ORL) connects the fibrous digital sheath on the volar surface to the extensor expansion connecting the PIP and DIP.
Figure 40-2. Extensor tendon zones.
4. Transverse retinacular ligament (TRL) prevents excessive dorsal shift of the LBs when the PIP extends.
5. Along with the intervolar plate ligament (IVPL), the sagittal band (SB) originates from volar plate at the level of the MP joint and contributes to the extensor hood to help centralize extensor tendon over MP joints and prevent lateral subluxation.
IV. PULLEY ANATOMY
A. General considerations
1. Pulleys are fascial condensations along flexor sheath
2. Hold tendon close to phalanges and improve biomechanics of flexor tendons by preventing bowstringing of tendons during flexion
B. Fingers: annular (5) and cruciate (3) pulleys
1. Annular pulleys
Figure 40-3. Dorsal wrist compartments. APL, abductor pollicis longus; ECRB, extensor carpi radialis brevis; ECRL, extensor carpi radialis longus; ECU, extensor carpi ulnaris; EDC, extensor digitorum communis; EDM, extensor digiti minimi; EIP, extensor indicis proprius; EPB, extensor pollicis brevis; EPL, extensor pollicis longus.
a. Odd-numbered pulleys arise from volar plates over MP and IP joints
b. Even-numbered pulleys arise from periosteum of proximal and middle phalanges
c. *A2 and A4 are the most important biomechanically to prevent bowstringing
2. Cruciate pulleys are between the annular pulleys
a. Thinner, compressible, and less biomechanically important than annular pulleys
b. C1 is located between A2/A3, C2 between A3/A4, and C3 between A4/A5 pulleys
C. Thumb: annular (2) and oblique (1) pulleys
1. Annular pulleys: A1 at MPJ and A2 at IPJ
2. *Oblique pulley: Extension of adductor pollicis attachment. Lies between A1 and A2. Most important pulley to prevent bowstringing in the thumb.
V. TENDON NUTRITION
A. Unsheathed
1. Unsheathed tendons are surrounded by paratenon and are considered vascular tendons.
2. Vessels enter from vessels in perimysium, at bony insertion, and at many points along the course of the tendon. They anastomose through a longitudinal system of capillaries.
B. Sheathed
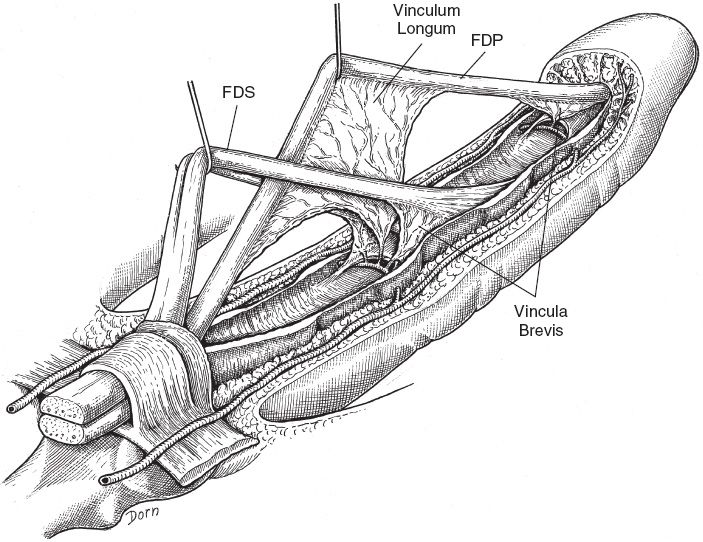
1. Within the tendon sheath, blood supply emanates from vessels in the perimysium, at bony insertion, and through “mesotenon” conduits called vincula at discrete points along the tendon (Fig. 40-4)
2. Synovial fluid, rich in protein and hyaluronic acid, provides additional tendon nutrition
3. Sheathed tendons are considered avascular tendons.
4. Areas between vincula are watershed zones that receive nutrition by synovial diffusion.
VI. TENDON HEALING
A. Phases of tendon healing
1. Inflammatory (first week): Injured tendon bathed with exudate, cells proliferate, and tendon is debrided by macrophages.
2. Proliferative (weeks 2 to 4): Capillary buds sprout and fibroblasts arrive, producing collagen at random.
3. Remodeling (months 2 to 6): Longitudinal organization of collagen fibers in line with stress.
Figure 40-4. Anatomy of the vincula longus and brevis. FDP, flexor digitorum profundus; FDS, flexor digitorum superficialis.
B. For unsheathed tendon, fibroblasts and capillary buds from paratenon migrate into the injured area.
C. Sheathed tendons are believed to have both intrinsic and extrinsic healing capabilities
1. Extrinsic: Fibroblasts migrate from sheath into the injured site (also form adhesions).
2. Intrinsic: Tendon cells can migrate across closely approximated ends and heal with nutrients from synovial fluid.
TIMING OF REPAIR
I. PRIMARY REPAIR (<24 HOURS)
A. Emergency repair is generally not necessary
B. Contraindications to primary repair include lack of stable soft tissue coverage, gross contamination, infection, and human bites
C. Under clean conditions, extensor tendon lacerations can be repaired in the emergency department; however, all flexor tendon injuries should be repaired in the operating room (OR)
II. DELAYED PRIMARY REPAIR (1 TO 14 DAYS)
A. Consider a delayed primary repair if the wound can be pulled open without making an incision.
B. Similar results to primary repair if done within the first week.
C. The risk of adhesions is increased after 1 week.
D. Generally a better option for heavily contaminated wounds.
III. SECONDARY REPAIR (>2 WEEKS)
A. Ideally, repair is performed before significant muscle shortening is present, which typically occurs after 3 weeks.
B. For functionally independent muscles (e.g., EPL), earlier repair is needed since they will retract faster than tendons with shared muscle bellies.
C. Tissue edema and tendon softening occur with longer delays.
D. Tricks if tendon ends will not easily come together
1. Gradual sustained traction of proximal segment to lengthen contracted sarcomeres.
2. Fractional lengthening at musculotendinous junction to provide 1 to 1.5 cm additional length.
TENDON GRAFTING
I. PRIMARY TENDON GRAFT
A. Only appropriate if flexor sheath and pulleys are intact, there is stable soft tissue coverage, and full passive motion is present
B. Indications
1. Segmental tendon injury
2. Neglected digital laceration with flexor tendon transection
3. Inability to perform delayed primary repair due to retraction of tendon ends
4. FDP avulsion
5. Failed flexor tendon repair
II. TWO-STAGED TENDON GRAFT
A. Staged reconstruction is preferred if above requirements for primary tendon grafting are not met and inflammation subsides (3 to 4 weeks after injury).
B. Indicated for severe soft tissue contractures, inadequate flexor sheath or pulleys, or when tendon repair is complicated by rupture, infection, or other soft tissue problems.
C. First stage
1. Native tendon is excised and temporary silicone implant (Hunter rod) is sutured to distal tendon stump.
2. Hunter rod encourages the formation of a pseudo-sheath, thus creating a bed for the graft.
3. At this time, any necessary pulley reconstruction, tenolysis, correction of joint contractures, soft tissue reconstruction, or nerve or artery repair is performed
D. Second stage. After 2 to 3 months, the Hunter rod is exchanged for a tendon graft (palmaris longus, plantaris, or toe extensor).
OPERATIVE CONSIDERATIONS
I. GENERAL CONSIDERATIONS
A. Atraumatic handling of tendon ends limits adhesion formation.
B. Some believe closure leads to less adhesion formation and improved healing.
C. Tendon ruptures should be explored immediately and repaired
D. Tensile strength–time relationship
1. Repair is weakest 7 to 10 days after repair
a. *Post-op day 10 is the most common time for rupture after primary repair.
b. Treat rupture with prompt exploration and repair.
2. Majority of strength back 4 to 6 weeks after repair.
3. Maximum strength at 6 months after repair
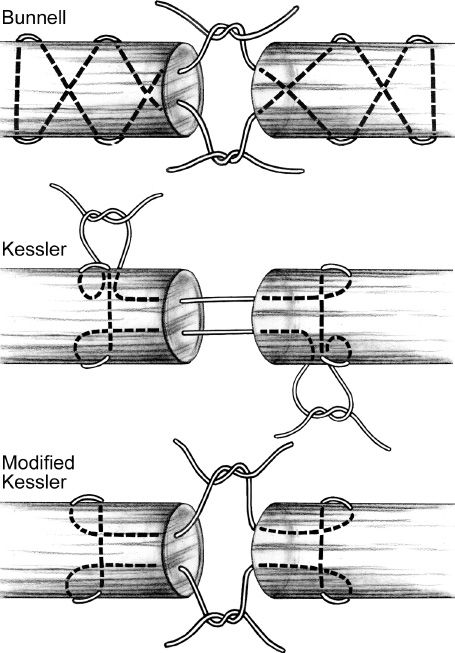
A. Core sutures (Fig. 40-5)
1. *Strength of repair is proportional to the number of core strands crossing the repair.
2. Larger caliber suture increases strength of repair (synthetic braided nonabsorbable 3-0 or 4-0 suture)
3. Tendons should be repaired using at least four strands, but usually six or more for greater strength and early active motion.
4. Although many techniques have been described, all have common features
a. Small grasping stitches avoid pullout
b. Knots buried in the repair site assist in smooth gliding
B. Epitendinous suture
1. Consists of a continuous circumferential 5-0 or 6-0 monofilament polypropylene stitch.
2. *Can add 10% to 50% strength to the core sutures.
3. Leads to decreased gap formation, which is the first step toward failure
4. Smoothens edges for gliding
5. Decreases adhesion formation
Figure 40-5. Core suture techniques. Generally modified Kessler is favored among contemporary surgeons. (From Berger RA, Weiss AC, eds. Hand Surgery. Philadelphia, PA: Lippincott Williams & Wilkins; 2004.)
FLEXOR TENDON INJURIES
I. GENERAL CONSIDERATIONS
A. Flexor tendons have a propensity to retract. Repair should be done in the OR under loupe magnification.
B. Neurovascular injury is common with flexor tendon injuries, so a detailed examination is paramount prior to local anesthetic infiltration.
C. A flexor tendon laceration will cause the affected finger to be more extended, disrupting the resting cascade.
D. The skin laceration does not always correlate with the level of injury. Lacerations that occur with the finger in flexion will result in the tendons being cut more distally than the skin.
II. PARTIAL LACERATIONS
A. Suspected if full range of motion (ROM) is present, but patient has weakness or pain with resisted flexion.
B. Should be explored
C. Repair laceration if greater than 60% of the tendon width, to prevent entrapment, late rupture, adhesions, and triggering.
D. If less than 60%, laceration should be left alone, as the repair may impede blood supply and/or create adhesions.
III. MANAGEMENT BY ZONES
A. Zone I: Middle of the middle phalanx to fingertip (distal to insertion of FDS, includes only FDP)
1. Laceration
a. Vincula usually keep proximal tendon end from retracting into palm.
b. Treat with direct repair
c. End-to-end repair is preferred
d. If distal end is short or nonexistent, reattach proximal end to bone via pull-out suture over a dorsal button or directly to bone with a suture anchor
e. *Avoid advancing FDP greater than 1 cm, which can result in the *“quadriga effect”—incomplete flexion of FDPs of uninjured fingers when the shortened FDP reaches maximum flexion too early
2. *Profundus avulsion (“jersey finger”): Leddy–Packer classification and treatment are based on level of retraction of tendon end
a. Type I
i. Proximal tendon end retracts into palm due to vinculae disruption.
ii. Requires treatment within 1 week because tendon will degenerate without nutrition from vincula or synovium.
b. Type II
i. Retracts to level of the PIP joint (PIPJ) because long vinculum remains intact.
ii. Tendon avulsed with or without small fragment of bone that gets caught at A3 pulley.
iii. Treatment can be performed up to a few months out
c. Type III
i. Retracts to A4 pulley (middle of the middle phalanx) because large bony avulsion fragment gets stuck on the pulley.
ii. Bone fragment may be seen proximal to DIP on X-ray
iii. May be repaired with K-wire fixation if fragment is large enough.
iv. Salvage procedures include DIP arthrodesis, tendon grafting, or tenodesis.
B. Zone II: Distal palmar crease to middle of the middle phalanx (both FDS and FDP tendons, with FDP volar, proceeding distally)
1. Within the fibrosseous sheath
2. Historically known as “no man’s land” due to high risk of adhesions and poor outcomes.
3. Both tendons should be repaired when possible
i. Results in better balance and prevents hyperextension deformity at the PIP
j. Improves gliding of FDP
k. Adds strength to finger
4. In cases of extensive injury (e.g., amputation) repair of FDP alone is acceptable.
5. Care should be taken to explore and repair any lacerated digital nerves.
6. FDS avulsions are less common. Patients may exhibit a mass at the A1 pulley and limited PIP motion. Treatment includes tendon excision.
C. Zone III: Transverse carpal ligament to distal palmar crease
1. Outcome is generally better than for zone II injuries.
2. FPL is rarely injured in this zone because of the overlying thenar muscles.
3. Associated injury to the common digital nerves and superficial palmar arch are common.
4. Lumbricals are within this zone and are on radial side of flexor tendon.
D. Zone IV: Under transverse carpal ligament (carpal tunnel)
1. Tendons injured in various combinations
2. Treat with operative repair before muscle contraction occurs.
3. Examine median nerve closely for injury
4. Transverse carpal ligament should be repaired and wrist should be splinted in neutral position to prevent bowstringing.
E. Zone V: Proximal border of transverse carpal ligament to musculotendinous junction
1. Generally have favorable outcomes unless there is associated neurovascular injury.
2. Repairs may be done without epitendinous suturing.
F. General exposure for flexor tendons
1. Brunner incision is standard. If using this technique, do not cross the flexion crease at right angles.
2. Do not create flaps with narrow tips.
3. Midaxial incisions are preferred. (Midaxial–bend the finger, marking the ends of the flexion creases with dots; connect the dots in an axial line. Dissection proceeds just dorsal to the neurovascular bundle.)
4. Do not cross web-space
G. Retrieval of proximal end
1. Do not struggle for too long
2. Follow a set pattern
a. One attempt at milking from proximal to distal
b. Single blind attempt with small mosquito forceps
c. Feeding tube: FPL lies below FCR and ulnar to radial artery
H. Repair
1. Core suture plus epitendinous suture
2. Core: 3-0 coated braided polyester suture which should be placed approximately 1 cm from the cut end
3. Epitendinous: 6-0 prolene
EXTENSOR TENDON INJURIES
I. GENERAL CONSIDERATIONS
A. Dorsum of hand and forearm divided into nine zones, which guide management and predict outcome.
B. The odd zones are over joints, while the even zones are in between
C. Can result from either laceration or avulsion injury
D. Compared to flexor tendons, extensor tendons exhibit little retraction due to multiple attachments.
E. In general, closed disruptions are treated with splinting, while open injuries are treated surgically.
F. Extensors are thin and often more difficult to suture.
G. For more distal injuries, the tendon is flat and may be repaired using figure-of-eight or horizontal mattress sutures repair.
II. PARTIAL LACERATIONS
A. Repair is indicated if greater than 50% of tendon width is injured.
B. For lacerations less than 50% of width, treat by splinting for 10 days, followed by protected range of motion.
III. MANAGEMENT BY ZONES
A. Zone I (mallet finger): Caused by disruption of the terminal tendon over the DIP joint usually due to forced flexion at DIP.
1. Type I: Rupture at tendon insertion, with or without small bone fragment.
a. Treat with extension splinting of the DIP joint (Stack splint) for 8 weeks.
b. Do not splint PIP
c. Percutaneous pinning of the DIP joint may be indicated for children or other circumstances of noncompliance.
2. Type II: Laceration at, or just proximal to the DIP joint
a. Treat with repair and extension splinting
b. Repair may be performed as single layer with the skin, using nonabsorbable suture—“dermotenodesis”.
3. Type III: Deep abrasion with loss of tendon and overlying soft tissue. Treat with soft tissue coverage and tendon grafting or joint fusion.
4. Type IV: Avulsion fracture (bony mallet)
a. Treat with splint if fragment is easily reducible and there is no subluxation of distal phalanx.
b. Treat with K-wire fixation and pinning of the DIP joint if subluxed.
5. Late presentations may also benefit from splinting, or, in some cases, extension block percutaneous pinning.
B. Zone II: Over the middle phalanx
1. Only one LB needed in its entirety to preserve active extension.
2. Lacerations are usually partial
a. For lacerations greater than 50% of tendon width, repair and splint DIP for 6 weeks while keeping the PIP free. Avoid shortening the extensor mechanism, which may lead to loss of flexion.
b. For lacerations less than 50%, splint DIP for 10 to 14 days, followed by motion exercises.
C. Zone III: Over the PIP (CS injury)
1. One of the most complex regions of the extensor mechanism
2. Open injury
a. Explore the PIPJ and thoroughly irrigate
b. Repair primarily using four-strand core suture technique or reconstruction using a slip of LB and extension splinting versus trans-articular K-wire immobilization for 4 to 6 weeks
3. Closed injury
a. Easily missed in emergency department or misdiagnosed as jammed finger
b. Patients present with swelling and tenderness at the proximal middle phalanx, with mild extensor lag at the PIPJ, and weak extension against resistance.
c. *Boutonniere deformity (flexion of the PIP and hyperextension of the DIP) usually develops if LBs sublux volarly.
d. Treat by splinting of the PIPJ only for 6 weeks; DIP flexion exercises are initiated with the PIP immobilized (draws LBs and CS distally, taking pressure off CS repair).
e. Trans-articular K-wire fixation of the PIPJ is an alternative to splinting.
D. Zone IV (and Zone II of thumb): Over the proximal phalanx
1. Injuries in this area are typically due to laceration
2. Tendon is flat and broad and partial lacerations are common
3. Treat like a Zone II injury
E. Zone V (and Zone III of thumb): Over the MP joint
1. Open injuries
a. Carefully review X-rays to rule out metacarpal head fracture or foreign body.
b. Always suspect human bite wound (“fight bite”) with any open injury even if not the history given.
i. Acute
a) Irrigate and debride aggressively in the OR, repair tendon, apply antibiotics, and leave wound open.
b) Suspect and rule out joint involvement.
c) May require several trips to the OR.
d) Tendon injuries are typically proximal to skin lacerations. Be wary of deeper penetration.
ii. Old/chronic: May require delayed treatment of tendon, until infection is controlled and soft tissue equilibrium reached
c. SB lacerations must be repaired to prevent extensor subluxation.
2. Closed injuries
a. Most often include SB tears
b. Patients present with pain, swelling, and inability to extend the MP joint
c. Extensor tendon subluxes ulnarly (most common) or radially (rare)
d. Treat with extension splint for 4 to 6 weeks.
e. May require open repair for chronic injuries or in cases where extensor mechanism remains malpositioned.
F. Zone VI (and Zone IV of the thumb): Over the metacarpals
1. Injuries in this area generally have a better prognosis than more distal injuries.
2. Tendons are of sufficient thickness for core suturing.
3. If tendon ends are easily retrievable, repair in the ED; otherwise, repair in the OR.
G. Zone VII (and Zone V of the thumb): Over the wrist joint, beneath the extensor retinaculum.
1. Repair tendon ± partial retinacular excision to prevent adhesions
2. Zone V thumb injuries often involve the abductor pollicis longus (APL) and extensor pollicis brevis (EPB) tendons. Explore and repair the superficial radial sensory nerve as indicated.
H. Zone VIII: Over the distal forearm
1. Repair at myotendinous junctions is often difficult.
2. Associate neurovascular injury is common.
3. May require tendon transfers if function is lost.
I. Zone IX: Muscles of proximal forearm
1. Injury to muscle often from penetrating trauma.
2. Repair of muscle bellies is difficult and requires multiple figure-of-eight sutures using large bites.
3. Tendon transfers may be needed as salvage procedures if function is lost.
POSTOPERATIVE CARE AND THERAPY
I. GENERAL CONSIDERATIONS
A. Early controlled mobilization is now the standard of care
B. Early motion increases gliding, prevents adhesions, increases collagen fibril size, and improves excursion, healing, and strength of tendon repairs
C. Requires cooperative patient and close interaction with physician and hand therapist
II. SPLINTING
A. Flexor tendons: Postoperatively, wrist should be splinted in 20 degrees flexion, MP joints in 60 degrees flexion, and digits should be held in full extension to avoid contractures
B. Extensor tendons: Extension splinting of involved joints with wrist in 45 degrees of extension and MP in slight hyperextension. Zone V and above injuries do not need joints distal to MPs splinted.
C. Small children or noncompliant patients may need elbow included in splint to hinder its removal
III. THERAPY
A. Protocols have common features
1. Most protocols are not applicable for uncooperative or noncompliant patients. For noncompliant children, a protocol of 3 or 4 weeks of cast immobilization followed by unrestricted motion is used.
2. Needs supervision by a well-trained hand therapist.
3. During periods of rest, the wrist and MP joints are splinted in flexion and the PIP and DIP joints are splinted in extension.
4. Six-core strand techniques in flexor tendons generally permit early active motion.
B. Flexor tendon therapy
1. Active extension with rubber band flexion (Kleinert and modifications)
a. Rubber band is attached to dynamic dorsal blocking splint with wrist and MP joints in flexion and IP joints in extension.
b. The rubber band passively flexes fingers, but the patient is able to actively extend.
2. Controlled passive motion (Duran and similar)
a. Allows passive motion of the digits in a resting splint.
b. At 4 weeks, active motion is started.
c. At 6 weeks, passive flexion and blocking exercises are started
d. At 8 weeks, strengthening exercises begin.
e. Thought to decrease flexion contractures compared to Kleinert.
3. Controlled active motion protocols
a. Resting splint exchanged for tenodesis splint during therapy.
b. Wrist motion is allowed as long as MP joints remain flexed past 60 degrees.
c. With wrist extended, IP joints are passively flexed and held for a brief period of time.
C. Extensor tendon therapy: A variety of early controlled motion protocols are available, depending on the injury. Generally rest for 3 to 4 weeks and then begin active motion.
COMPLICATIONS
I. TENDON RUPTURE
A. Often occurs with overly aggressive use of hand or in cases of patient non-compliance.
B. Diagnosis may be aided by MRI or ultrasound.
C. *Rupture should be explored immediately and repaired.
D. For recurrent rupture, tendon grafting, tendon transfer, or arthrodesis may be indicated.
II. ADHESIONS
A. May occur despite the best repair and post-operative rehabilitation.
B. Generally, adhesions following flexor tendon repair more common than with extensor tendon injuries.
C. Tenolysis
1. *Indicated when adhesions limit motion and there is a failure to improve ROM after 3 months.
2. Diagnosed when there is a discrepancy between active and passive ROM.
3. In flexor tendons, A2 and A4 pulleys should be preserved to prevent bowstringing.
4. SBs should be preserved for extensor tendon tenolysis
5. Dorsal capsular release may be needed with extensor tenolysis
a. Tenolysis should not be considered until the patient is 3 to 6 months out from repair and progression with therapy has reached a plateau.
b. Therapy should be maximized to obtain full passive motion of all joints.
c. Soft tissues should achieve equilibrium and tendon should be healed.
7. Immediate range of motion excises and therapy are started postoperatively.
8. Complications include tendon rupture and need for staged reconstruction.
9. When wound beds are densely or extensively scarred, tendon transfers may be indicated.
10. Flexor tenolysis is tedious, and its technical difficulty should not be underestimated.
III. SWAN-NECK DEFORMITY (*DIP FLEXION AND PIP HYPEREXTENSION)
A. Nonrheumatologic cases typically from chronic mallet finger and PIP volar plate injury.
B. Transverse retinacular ligaments become stretched eventually causing dorsal subluxation of the LBs.
C. Splinting may suffice in mild cases, but surgical correction of underlying deformity is often needed in severe cases.
IV. BOUTONNIERE DEFORMITY (*PIP FLEXION AND DIP HYPEREXTENSION)
A. Nonrheumatologic causes typically include CS or FDP disruption or injury to the TL that holds the two terminal ends of the LBs together.
B. Transverse retinacular ligaments become stretched with eventual volar subluxation of the LBs.
C. Surgery may be needed to correct underlying deformity in severe cases.
V. *QUADRIGA
A. Weakness and incomplete flexion of the unaffected digits following repair of the FDP tendon of the long, ring, or small finger due to their common muscle origin.
B. Results from functional shortening of profundus tendon.
C. Shortened tendon achieves full excursion, while the unaffected digits do not
D. Less likely to result following injury to the index profundus since it has an independent muscle origin.
E. Often occurs following advancement of the FDP tendon during repair, excessive tension of tendon graft, or scarring of the FDP tendon after amputation.
F. Treatment includes tenotomy, tenolysis, or tendon lengthening.
TENDONITIS
I. STENOSING TENOSYNOVITIS (TRIGGER DIGIT)
A. Enlargement of the flexor tendon, causing a size discrepancy between the tendon and annular pulley, causing catching and locking symptoms during tendon excursion.
B. May be nodular or diffuse, as seen with rheumatoid arthritis.
C. A1 pulley is the most common site. Proximal edge is located at the distal palmar crease in the little and ring fingers, between the proximal and distal creases in the middle finger, and at the proximal crease in the index finger and thumb.
D. Order of frequency of the affected digits: Thumb most common, then ring finger, middle finger, index finger, small finger.
E. Middle-aged women are the most common group.
F. Most cases are idiopathic, but there is an increased incidence with diabetes, rheumatoid arthritis, gout, and amyloidosis.
G. Presenting symptoms
1. Catching, sticking, or occasional locking of fingers in flexed position.
2. Pain in distal palm, commonly referred to the PIPJ.
3. Symptoms are often worse on awakening.
4. Nodule palpable on tendon with movement.
1. Splinting
a. Low success rate
b. Extension splint of the affected digits (especially at nighttime if AM symptoms)
2. Injection of steroid (with local anesthetic)
a. Successful in 50% to 90% of cases, but recurrence is high.
b. Less successful in diabetics, chronic cases, and when diffuse rather than nodule tenosynovitis is present.
c. Steroid (with local anesthetic) is injected into tendon sheath at the level of the A1 pulley
d. Use small gauge needle; insert down to bone; back out slowly, with pressure on plunger, stopping when solution flows easily into tendon sheath. A fluid wave can be felt down the finger in most cases.
e. Remind diabetics that steroids will affect their blood sugar levels
3. Surgery
a. Indications
i. Long-standing triggering
ii. Persistent triggering that fails injection and splinting
b. A small transverse or Bruner-type incision at proximal edge of pulley and division of the entire A1 pulley is made under direct vision.
c. The digital neurovascular bundles should be visualized and protected, especially at the thumb where radial bundle courses directly over the A1 pulley.
d. Percutaneous release may be performed but is contraindicated in the thumb and index finger due to the risk of digital nerve injury.
II. DEQUERVAIN’S TENOSYNOVITIS
A. Stenosing tenosynovitis of the tendon in the first dorsal compartment of the wrist (APL and EBL)
B. Common cause of radial-sided wrist pain
C. *Signs and symptoms
1. Radial-sided wrist pain with thumb use
2. Tenderness over first dorsal compartment (radial styloid)
3. No pain with axial grind test, which is positive in first CMC joint arthritis
4. Positive Finkelstein’s test: Pain with thumb tuck and ulnar deviation of wrist.
D. Treatment
1. Splinting (forearm-based thumb spica) and NSAIDs for mild or early cases
2. Steroid injection into first dorsal compartment
a. Inject steroid (plus local anesthetic) into distal end of compartment.
b. Limited success due to multiple slips of APL (two to four), each in their own subcompartment.
3. Surgery
a. Release of the first dorsal compartment with tenosynovectomy.
b. All subcompartments must be released
c. Superficial radial nerve should be visualized and avoided during dissection.
d. Subluxation of the first compartment may occur if the retinaculum is released too far radially.
III. INTERSECTION SYNDROME
A. *Inflammation and pain of the dorsal wrist where the first dorsal compartment (APL and EPB) crosses the second dorsal compartment (ECRL and ECRB), approximately 4 cm proximal to the wrist.
B. Often a history of repetitive wrist motion
C. Crepitus can sometimes be felt at the intersection site
D. Treatment
1. Activity modification, splinting (forearm-based thumb spica), and NSAIDs for mild or early cases.
2. Steroid injection (with local anesthetic)
3. Although uncommon, surgery is indicated for refractory cases and consists of release of the second compartment followed by postoperative splinting.
IV. FLEXOR CARPI RADIALIS TENDONITIS
A. Inflammation and tenderness along FCR and pain with resisted wrist flexion and radial deviation.
B. Associated with repetitive, forceful wrist flexion
C. More common in women
D. Linburg syndrome (tenosynovitis due to tendinous connection between FPL and FDP to index finger) must be ruled out
E. Treatment
1. Splinting, NSAIDs, and activity modification
2. Steroid injection
3. Surgical release of FCR considered if conservative measures fail. Care must be taken to avoid injury to palmar cutaneous branch of median nerve.
V. FLEXOR CARPI ULNARIS TENDONITIS
A. Inflammation and tenderness along FCU and pain with resisted wrist flexion and ulnar deviation.
B. Caused by chronic repetitive trauma and overuse
C. More common in women
D. Pisotriquetral arthritis should be ruled out
E. Treatment: Same as for FCR tendonitis. Surgery is rarely required.
1. Splinting, NSAIDs, and activity modification
2. Steroid injection
3. Surgical release of FCU considered if conservative measures fail. Care must be taken to avoid injury to palmar cutaneous branch of ulnar nerve
VI. EXTENSOR CARPI ULNARIS TENDONITIS
A. Associated with overuse
B. Tendon subluxation may be associated with triangular fibrocartilage complex (TFC) tears
C. Patients who fail conservative treatment measures may require tenosynovectomy with sheath release and arthroscopic evaluation to rule out a TFC tear
VII. OTHER FORMS OF TENDONITIS
A. ECU, EPL, EIP tendonitis
1. Associated with overuse
2. Treatment: NSAIDS, splinting, activity modification, and injections
3. Surgery for EPL tendinitis to prevent rupture
PEARLS
1. Flexor tendons should be repaired using four to six stranded core sutures
2. Earlier flexor tendon repair is associated with better results
3. Avoid advancement of flexor tendons during repair, which can result in the quadriga effect
4. Always repair flexor tendons in the OR under loupe magnification
5. Do not be fooled by juncturae tendinum when evaluating for an extensor laceration
6. Partial injuries are common with extensor tendon lacerations
7. Know relationship of flexor tendons within carpal tunnel (FDS to MF and RF are volar to IF and SF)
QUESTIONS YOU WILL BE ASKED
1. Describe the flexor and extensor zones.
See Figures 40-1 and 40-2.
2. Name the tendons within the 6 extensor compartments.
See Figure 40-3.
3. Describe the location of the pulleys, and identify which ones are most important to preserve.
See “Hand and Wrist Anatomy and Examination” Chapter 38—Figure 2. Most important digital pulleys are A2 (over the proximal phalanx) and A4 (over the middle phalanx). Most important thumb pulley is the oblique.
4. Describe the Leddy-Packer classification for “jersey finger” injury.
Type I: Retracts to the palm.
Type II: Retracts to the PIPJ, held by vincula.
Type III: Remains near DIP with bony fragment trapped by A4 pulley.
5. What is the “quadriga effect” and where did the name originate?
The “quadriga effect” refers to limited excursion of the middle, ring, and small fingers due to tethering connections between the profundus tendons due to a common muscle belly. It can be from scarring of an FDP tendon or iatrogenic from an overly tight tendon repair or suturing of the FDP to the extensor. The name refers to the reins of a 4-horse roman chariot, which was called a quadriga.
Recommended Readings
Blair WF, Steyers CM. Extensor tendon injuries. Orthop Clin North Am. 1992;23(1):141–148. PMID: 1729662.
Lisney SJ. The proportions of sympathetic postganglionic and unmyelinated afferent axons in normal and regenerated cat sural nerves. J Auton Nerv Syst. 1988;22(2):151–157. PMID: 3379252.
Strickland JW. Flexor tendon injuries: I. Foundations of treatment. J Am Acad Orthop Surg. 1995;3(1):44–54. PMID: 10790652.
Strickland JW. Flexor tendon injuries: II. Operative technique. J Am Acad Orthop Surg. 1995;3(1): 55–62. PMID: 10790653.
Verdan CE. Primary repair of flexor tendons. J Bone Joint Surg Am. 1960;42-A:647–657. PMID: 13855215.
< div class='tao-gold-member'>