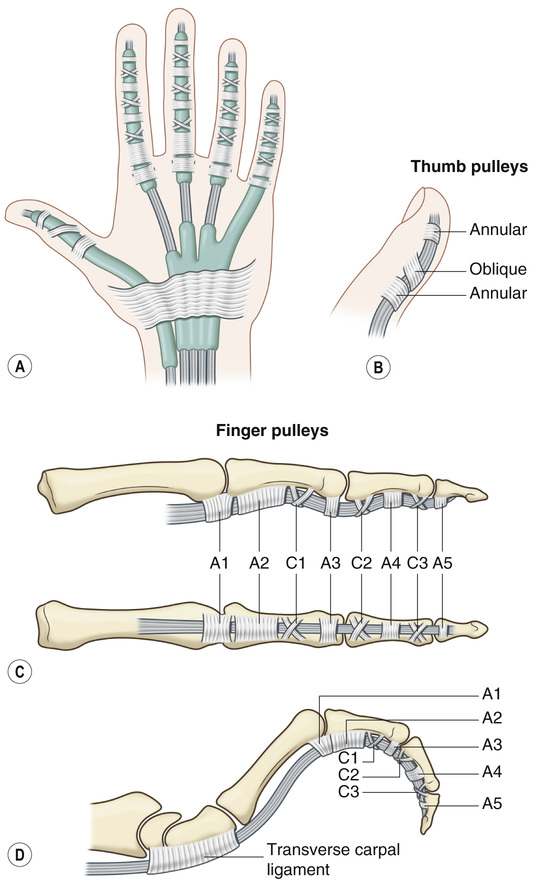
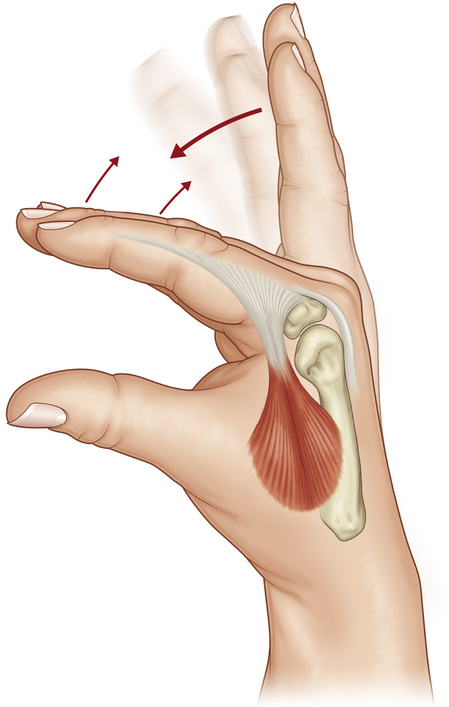
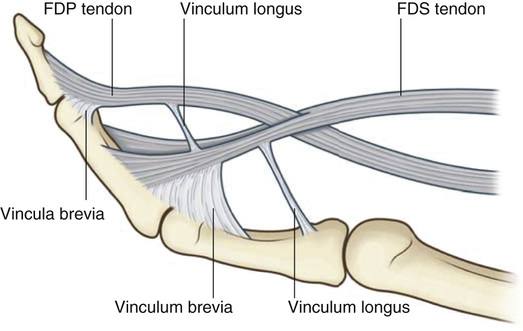
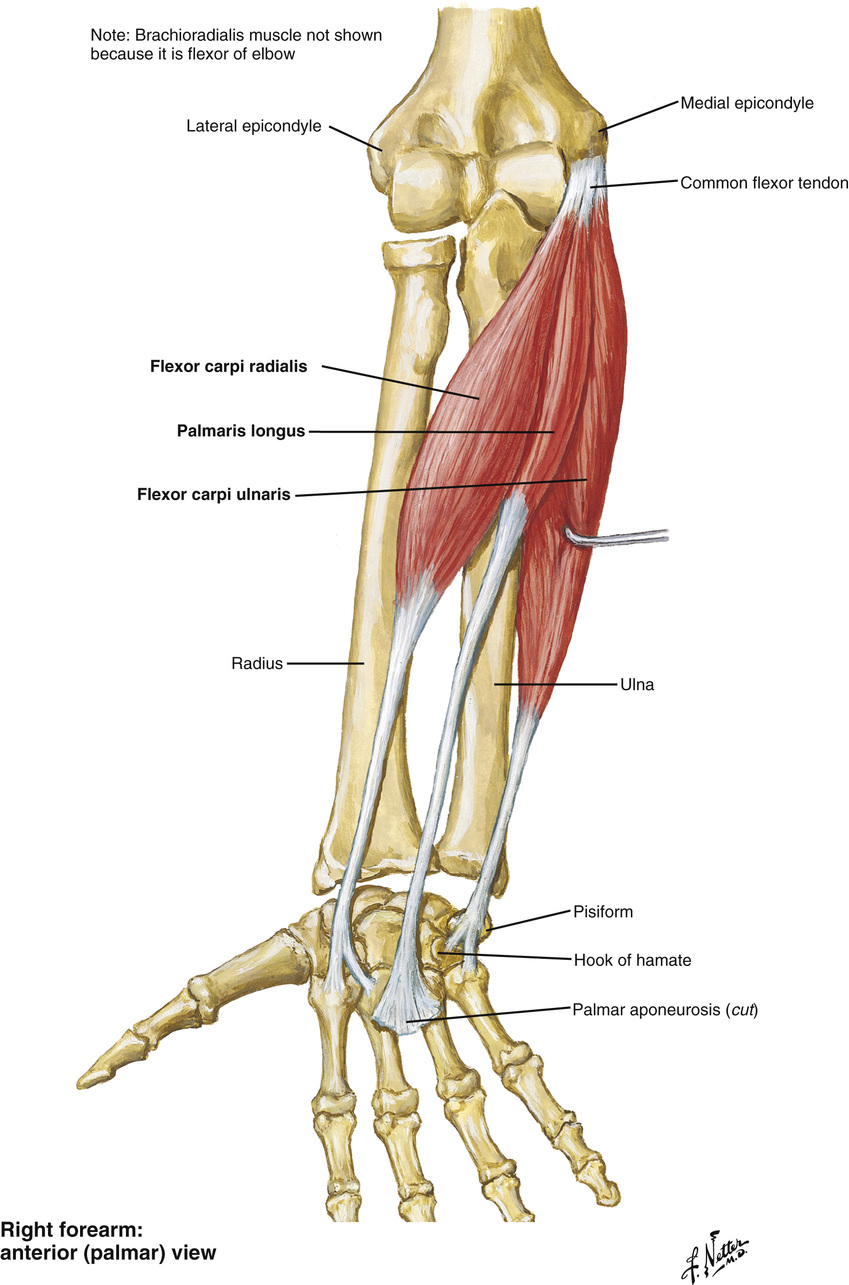
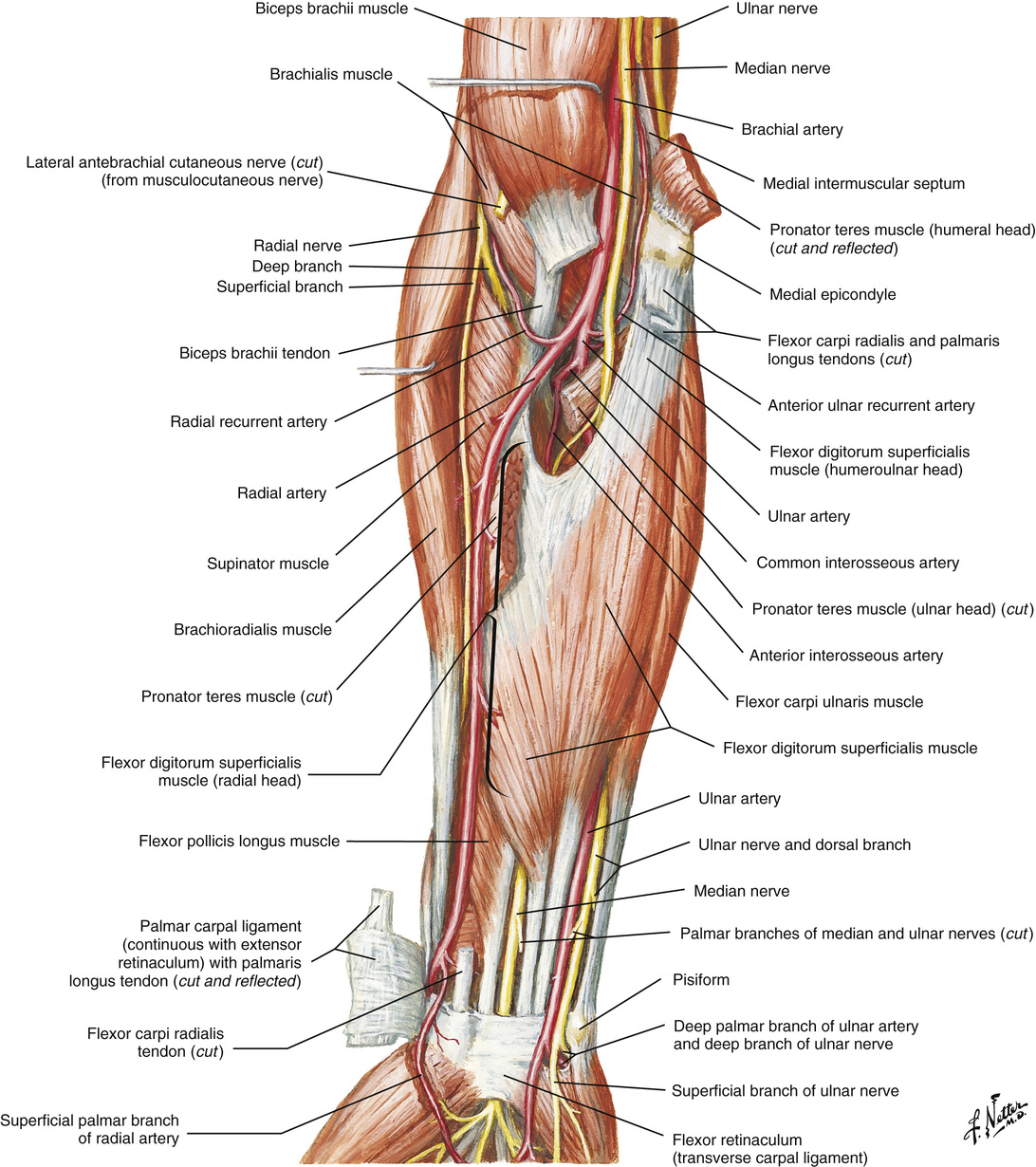
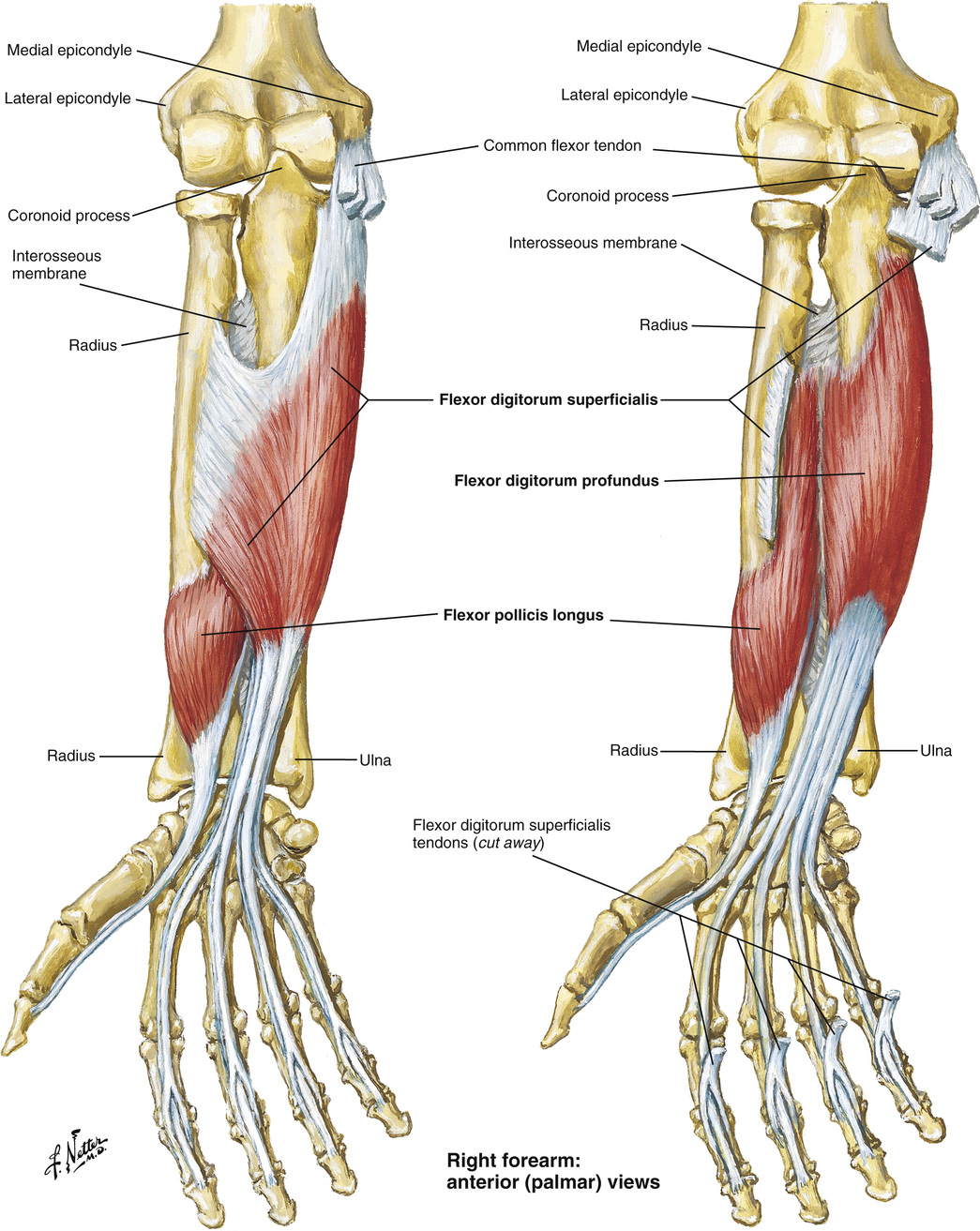
1. There are 12 flexor tendons in the hand and forearm. Common flexor group arises near the medial epicondyle. Most are median n. innervated, except the flexors to the 4th and 5th digits and interossei. ▪ Flexor digitorum superficialis (FDS) ○ Separate muscle belly origin, allowing independent finger motion ○ Flexes the proximal interphalangeal (PIP) joint ▪ FDP ○ Inserts into the volar aspect of the distal phalanx ○ Flexes the distal interphalangeal (DIP) joint ○ Lumbrical muscles originate from FDP tendon in the palm. ▪ Flexor pollicis longus (FPL) ○ Arises from the midaspect of the radial shaft and interosseous membrane ○ The only tendon inside the flexor sheath of the thumb; inserts onto the distal phalanx ○ Flexes the thumb interphalangeal (IP) joint ○ Inserts onto the base of the 2nd and 3rd metacarpals ○ Inserts onto the base of the 5th metacarpal, hook of hamate, and pisiform ○ Overlies ulnar artery and nerve ♦ Laceration to FCU is concerning for injury to the ulnar a. and n. ○ Ends in the fan-shaped palmar fascia ○ Lies volar to median nerve traveling within carpal canal ○ Lacerations to PL are concerning for median nerve laceration. ▪ Interossei muscles act as prime flexors of the MCP joints and extensors of the IP joints through their pull on the lateral bands (see Figure 19.5). • Nutrition of flexor tendons occurs through the synovial sheath, insertion, and vincula, which provide blood vessels directly to the tendon proper (see Figure 19.6). 3. Flexor tendon zones: Divisions of the flexor tendon anatomy within the hand that have important implications in fundamentals of repair (see Figure 19.7) 4. Carpal canal anatomy: Contains 9 tendons (4 FDS, 4 FDP, and 1 FPL) and the median nerve. Anatomic relationships within the canal are consistent; knowledge of these relationships is important when repairing injuries in this zone (zone 4). • FDP tendons lie on the dorsal floor of the carpal canal. • FPL tendon lies radial, deep, and adjacent to the scaphoid and trapezium 1. Indications and contraindications to flexor tendon repair (see Box 19.1) 3. Strength of the tendon repair is affected by • Number of core suture strands across the repair site ▪ Strength proportionate to the number of strands ▪ Relevant to gap formation and stiffness ▪ Tendon–suture locking technique, diameter of suture locks, suture caliber and material • Holding capacity of the tendon • Early mobilization and range of motion may also increase the strength of repair. 4. Recommended repair technique: A 3-0 or 4-0 core coated nylon or woven/braided polyester suture (4 to 6 strands) on a tapered needle (with approximately 1 cm of tendon purchase), with a locking tendon–suture junction and a 6-0 nylon epitendinous suture • Lacerations <50% to 60% of the tendon do not require repair. • Trim frayed edges to prevent a trigger site within the annular pulley system. • In the fingers, the A2 and A4 pulleys are the largest and most important to hand function. • Incision of the A2 pulley up to ▪ May be required for assistance with repair • In the thumb, A1 and oblique pulleys are most important to function. 7. Common complications of tendon repairs ▪ Can develop from traumatic technique during repair, excessive scarring, and prolonged immobilization • Rupture ▪ Most commonly occurs within 1 to 2 weeks and at suture knots ▪ Secondary tendon grafts, or staged reconstruction with Hunter rods, may be required in the presence of delayed rupture, multiple surgical failures, and retraction or excessive scarring. ○ One-stage tendon grafting is contraindicated in joints with absent passive range of motion. 8. Early postoperative motion of repaired tendons is critical for prevention of adhesions and strengthening the repair. • Motion typically begins 2 to 5 days after repair. • Early postoperative motion protocols ○ Allows active extension with passive flexion (“Kleinert” method) ○ Under supervision, allows active extension and active flexion. • Characterized by inability to flex the DIP • Tendon may be held out to length by vinculum • Proximal zone injuries are usually amenable to direct suture repair. • Take care to preserve the A4 pulley. • Avulsion and fracture/avulsion injuries of the FDP tendon (“jersey finger” injuries) require special consideration (see Chapter 16: Hand Fractures and Dislocations) • Often involves both FDP and FDS tendons • May disrupt the vincula, with retraction of the proximal tendon ends into the palm • Adequate exposure requires Bruner incisions and windows or releases within the synovial sheath and/or pulley system. ▪ Attempts to preserve the A2 pulley (at least • Many surgeons advocate repairing both FDP and FDS tendons. • Repair techniques almost identical to those for zone 2 • Injuries in zones 3 to 5 have better prognosis because of a richer vascular supply and less constricting tissue overlying the tendons (i.e., pulleys). ▪ Zone-5 repairs have the best outcomes because of the greater area allowed for tendon gliding. ▪ Zone-4 injuries are often associated with concomitant injuries to the median n. ▪ May require lengthy repair, with intermittent deflation and reinflation of the tourniquet during surgery to allow episodic hand perfusion ○ Often allow 20 to 30 minutes of perfusion between 2-hour intervals of tourniquet ischemia. 4. FPL injury • Repair techniques and principles similar to those for repair of the FDP tendon in the fingers • Proximal tendon end frequently retracts into the thenar musculature. • Closed injuries can occur with fracture and/or rupture from attrition (e.g., scaphoid malunion). 5. Stenosing tenosynovitis (“trigger” finger/thumb) • Characterized by entrapment of the flexor tendon at the A1 pulley, resulting in pain and catching, popping, or “locking” of the involved digit during flexion and extension ▪ May be associated with a painful, palpable nodule along the flexor tendon • Caused by hypertrophy of the A1 pulley or occasionally intratendinous swelling 2. The common extensor tendon arises from the lateral epicondyle of the humerus. 3. The extensor retinaculum prevents bowstringing of the extensor tendons across the wrist. 4. Unlike the flexor tendons, the extensor tendons do not lie within synovial sheaths. 5. Extension of the phalanges is dependent on the extrinsic extensors at the MCP joints, and the extrinsic and intrinsic muscles at the IP joints. 7. The extensor digitorum tendons are interconnected by intertendinous bridges (juncturae) that can provide some backup finger extension (albeit weak) in the setting of proximal extensor tendon injury. 8. There are 6 dorsal extensor compartments at the wrist; knowledge of their location and contents is important. • Extensor compartment 1: Abductor pollicis longus (APL) and EPB ▪ APL tendon can have multiple slips. ▪ May have septations between APL and EPB ▪ Dorsal sensory branch of the radial n. lies superficial to extensor compartment 1 • Extensor compartment 2: Extensor carpi radialis longus (ECRL) and extensor carpi radialis brevis (ECRB) ▪ Insert on the 2nd and 3rd metacarpal base, respectively ▪ ECRB is the prime wrist extensor (because of insertion). ▪ Crosses wrist above extensor compartment 2 and then reorients around Lister’s tubercle to the thumb ▪ Vulnerable to rupture (e.g., distal radius fractures) • Extensor compartment 4: Extensor digitorum communis (EDC) and extensor indicis proprius (EIP) ▪ EIP rests ulnar and deep to the EDC tendon to the index finger. ▪ Posterior interosseus n. lies deep to extensor compartment 4. ▪ Typically has 2 tendon slips ▪ Rests ulnar and deep to the EDC tendon to the small finger • Extensor compartment 6: Extensor carpi ulnaris (ECU) • The palmar interossei arise from the medial side of the 2nd, 4th, and 5th metacarpal, cross volar to the MCP joint, and join the extensor apparatus at the level of the proximal phalanx. ▪ Function to adduct the fingers, flex the MCP joint, and extend the IP joints • The dorsal interossei arise from the adjacent sides of the 5 metacarpal bones and join the extensor apparatus. ▪ Function to abduct the fingers, flex the MCP joint, and extend the IP joints • The lumbrical muscles arise from the radial side of the FDP tendons at the level of the metacarpal and join the extensor apparatus on the radial side. ▪ Function primarily as IP extenders 10. Extensor tendon zones: Divisions of the extensor tendon anatomy within the hand that have important implications in fundamentals of repair (see Figure 19.11)
Tendon Injuries and Reconstruction
Flexor Tendon Anatomy (see Figures 19.1–19.4)
General Flexor Tendon Repair Principles
 or 2/3rds its length, or release of the entire A4 pulley, can be tolerated without significant functional deficits.
or 2/3rds its length, or release of the entire A4 pulley, can be tolerated without significant functional deficits.
Flexor Tendon Injuries
 to
to  ) are important, functionally.
) are important, functionally.
Extensor Tendon Anatomy (see Figures 19.8–10)
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Tendon Injuries and Reconstruction
Chapter 19