Technique for Ptosis Correction
Ashley A. Campbell
Christopher C. Lo
Richard D. Lisman
DEFINITION
Blepharoptosis, or ptosis, is the abnormally low position of the upper eyelid in primary gaze. Ptosis is classified by its etiology as congenital, involutional, neurogenic, myogenic, and mechanical.
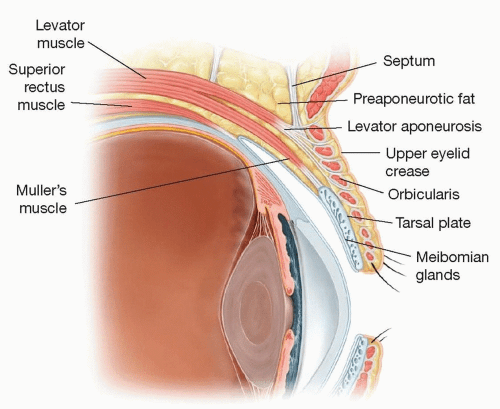
ANATOMY (FIG 1)
In normal eyelid anatomy, the upper eyelid retractors are the levator muscle (innervated by cranial nerve III) and the Mueller muscle (innervated by the sympathetic system).
The levator muscle extends from the lesser wing of the sphenoid just above the annulus of Zinn to Whitnall ligament; at this point, it transitions to become the levator aponeurosis.
The lid height is determined by the attachment of fine strands from the levator aponeurosis to the pretarsal skin and orbicularis muscle.
The upper eyelid fold is subsequently created by the overhanging skin, fat, and orbicularis muscle superior to the crease.
Mueller muscle originates from the undersurface of the levator aponeurosis to the superior tarsal margin. It provides about 2 mm of elevation to the upper lid.
The upper eyelid tarsus is a dense plate of connective tissue that acts as structural support to the eyelids. It measures 10 to 12 mm in the vertical dimension.
PATHOGENESIS
The most common type of ptosis is involutional (also referred to as aponeurotic).
This occurs gradually with age and is thought to be related to dehiscence of the levator from its attachment to tarsus.
Involutional ptosis may be related to contact lens use, prior eye or periocular surgery, eye rubbing, and chronic ocular allergy. These all produce a levator dehiscence.
NATURAL HISTORY
Involutional ptosis typically presents as a gradual decrease in lid height over time.
PATIENT HISTORY AND PHYSICAL FINDINGS
Patient’s primary complaint is often eyelid height or crease asymmetry and/or a gradual decrease in the size of the palpebral aperture.
This often produces the complaint of a tired appearance in patients presenting for aesthetic correction.
Visual symptoms include superior visual field loss and even central loss of vision in severe cases.
This often presents with highly elevated/arched eyebrows with deep frontalis contraction in an involuntary attempt to open each aperture. Less commonly, the patient may present with a chin-up posture in an involuntary attempt to look
out from under the resultant “canopy effect.” If long standing, neck pain or postural problems can result.
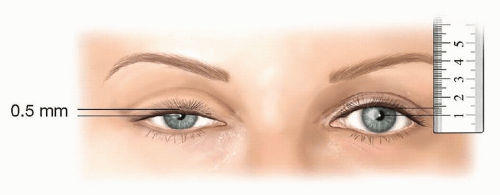
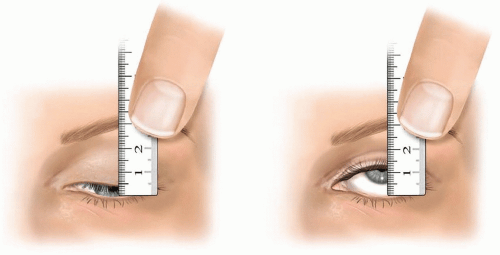
FIG 2 • Marginal reflex distance is measured from the central corneal light reflex to the upper eyelid while the patient sustains a neutral gaze in primary position.
Pertinent questions to ask in the patient’s history include onset of ptosis, a history of trauma, a history of contact lens wear, prior surgery or botulinum toxin injections, fluctuations in the eyelid height, diplopia, and any associated systemic manifestations.
Ocular history, especially including the history of dry eyes, should be obtained.
Old photographs are useful in determining onset and degree of prior ptosis.
Important aspects of the physical examination include the following:
Margin reflex distance (MRD): measured from the central corneal light reflex (usually the center of the pupil) to the upper eyelid margin. Normal measurement is 3 to 4 mm. In ptosis patients, this is reduced (FIG 2).
Palpebral fissure (PF): measured from the lower to upper eyelid margin in the midpupillary axis. Normal measurement is 8 to 10 mm. In ptosis patients, this is reduced.
Levator function (LF): measures the upper eyelid excursion from extreme downgaze to extreme upgaze while the brow is neutralized (FIG 3). This is critical in determining what ptosis repair technique is most appropriate. Normal measurement is 14 to 16 mm, and a value less than 5 mm indicates that either congenital blepharoptosis or acquired neurogenic etiologies need to be investigated prior to ptosis correction.
Lid crease height (LC): should evaluate shape and height. In the case of involutional ptosis, the LC is often elevated as the levator muscle is disinserted from its attachment to the tarsus.
Bell phenomenon: the involuntary upward movement of the eye on lid closure. This needs to be assessed to determine the degree of corneal exposure should there be any lagophthalmos postoperatively.
In asymmetric ptosis, Hering law should be evaluated by mechanically lifting one ptotic eyelid and observing the contralateral eyelid positional change.
Pupillary examination should be performed to assess symmetry and reactivity in light and dark to rule out a Horner syndrome.
Humphrey visual field testing performed with and without taping of the upper eyelid can be performed to demonstrate a superior visual field defect that is often present in patients with severe ptosis.
IMAGING
Imaging is not typically required in the ptosis workup, unless there is any indication of a myogenic or neurologic etiology for ptosis.
If the patient describes any variation in the amount of ptosis throughout the day or any double vision, a myogenic cause of ptosis (such as myasthenia gravis, chronic progressive external ophthalmoplegia, and myotonic dystrophy) should be considered. In this case, a referral to neuro-ophthalmology for further lab testing is indicated.
If there is any evidence of unilateral ptosis in the context of a meiotic pupil (suggesting a Horner syndrome) or abnormal eye movements (suggesting a cranial nerve III palsy), a referral to neuro-ophthalmology for further workup is also indicated.
DIFFERENTIAL DIAGNOSIS
Congenital ptosis
Myogenic
Myasthenia gravis
Chronic progressive external ophthalmoplegia
Myotonic dystrophy
Neurogenic
Horner syndrome
Cranial nerve III palsy
Mechanical
Traumatic
Dermatochalasis/blepharochalasis
SURGICAL MANAGEMENT
Many operative techniques have been described for the correction of involutional ptosis associated with moderate or good levator function. These include levator reinsertion, mullerectomy, and the Fasanella-Servat procedure.
Here, we describe the modified Fasanella-Servat procedure, which is our procedure of choice out of many for aesthetic patients who obviously demand the most symmetry and have a good tear film and tear production. It is also possible to perform this ptosis correction in conjunction with other aesthetic procedures, and it does not require the patient’s cooperation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree