CHAPTER 28 Suture suspension for brow and upper face
History
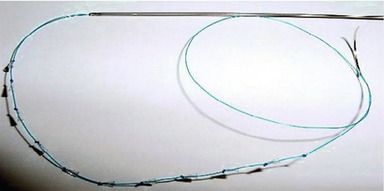
Both barbed suture design and treatment have evolved since their introduction. The original APTOS suture was a multiple-dented suture meant to provide additional traction in tissue. This design was modified to be bi-directional, with the barbs oriented so that tissue would be retained in the central region of the suture without the need for anchoring at either end (Fig. 28.1A). It was then re-designed as a multiple-barbed polypropylene suture intended to provide traction and suspension unidirectionally (Fig. 28.1B). Approval from the FDA for the extended length unidirectional barbed suture was obtained by two different companies in 2004 and 2005, respectively. No other variant of the barbed suture has received approval, but a newer technology called the Silhouette suture (Figs 28.1, Fig. 28.2), which involves the use of clear, flexible, absorbable cones with accompanying small knots on a polypropylene thread, to allow for more effective soft tissue elevation, received FDA approval in November 2006.
Physical evaluation
Closed suture suspension of the brow
In the brow area there is questionable longevity because of the amount of tissue excursion that naturally occurs in this area, but it does provide a non-surgical alternative. The technique is best supplemented with Botox injections before the procedure and also continuing afterwards in order to relax the frontalis, corrugator, and lateral orbicularis muscles to decrease dynamic activity. In a presentation by Dr Nicanor Isse at the American Society of Plastic Surgery in New Orleans in 2005, his review of cases showed a 70% failure rate of brow suture suspension. Patients who might be considered good candidates would be those with mild bilateral brow ptosis with very modest expectations and accepting of an uncertain, but limited, longevity, and who wished to avoid a more extensive surgical procedure. Also, patients who have unilateral ptosis either due to facial asymmetry or neuropraxia of the temporal branch of the facial nerve, occurring after a previous surgery, may find this as a means of temporarily improving facial symmetry while awaiting return of nerve regeneration. In some patients who have a more pronounced soft tissue glide plane after open or endoscopic surgery, brow elevation with threads may provide a modest, but temporary, improvement, with a much less invasive procedure.
Closed suture suspension of midface (closed melopexy)
In considering facial rejuvenation, there are four main areas where correction is required:
The closed midface melopexy only minimally improves tissue descent and volume loss and does nothing for muscle-induced lines or skin changes. Rating each of these areas on a scale of 1 to 4 with the highest score being 4, closed suture suspension provides for tissue descent at best at 0.5 and volume lost at best 0.5 (Table 28.1). It provides no effect on muscle-induced lines or skin changes, giving it a total of one out of four or 25%. For this reason, I call this the 25% rule or 25% lift, meaning that the closed melopexy with sutures provides a 25% improvement with the mini–open face lift, 25% of recovery, 25% of duration, and 25% of cost (Table 28.2). There is an important reason for the disappointing outcome. Suture lifting or suture traction by the threads lifts only the soft tissue which has not previously been dissected. For truly effective lifting to occur, tissue dissection needs to be performed so that tissues can be transposed and anchored under less tension, maintaining the lift until the tissue planes have healed in their new position. In summary, the results are not long-lasting, but they do provide a solution for certain unique situations.
Table 28.1 Effects of thread lift
| Tissue descent | 0.5 |
| Volume loss | 0.5 |
| Muscle induced lines | 0.0 |
| Skin changes | 0.0 |
| 25% | 1 out of 4 |
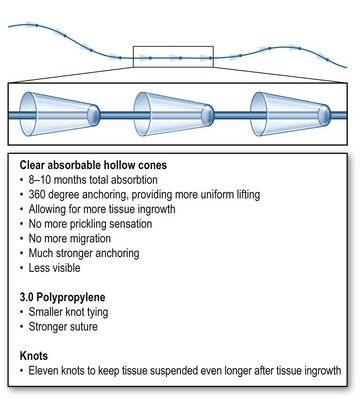
The new Silhouette suture is stronger than the conventional barbed sutures, it stands less chance of breakage, and it interacts with normal tissues through surrounding collagen tissue formation for better results. The suture consists of a 25 cm long 3-0 non-absorbable polypropylene suture that is 50% thinner than the 2-0 used in the design of the barbed sutures. This decreases knot palpability and pain in the temporal area. Suture strength is maintained by avoiding oblique cuts in the suture, in order to create the “barbs” (30–50% loss of suture strength). Each suture holds 11 clear, flexible, absorbable hollow cones that allow for tissue growth inside and around the cones (co-polymer of glycolic acid and lactic acid) (see Fig. 28.2). An immediate anchoring effect is created by the cones. A delayed anchoring effect is produced by a series of knots created on the distal 10 cm of the suture, which is intercolated with the cones (Fig. 28.3). The knots control the position of the cones and create further anchoring of the soft tissue, in turn creating collagen deposition around and inside each loop of the knot. These sutures can easily and safely be removed after the cones are completely absorbed using a small microphlebectomy hook.
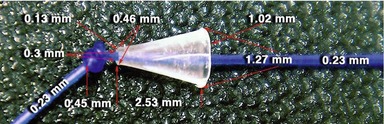
The co-polymer cones (Fig. 28.4) are soft and avoid the pinprick effects of the barbed suture. Their large size (1.0 mm × 2.5 mm) creates a strong grasping effect on the fibrous soft tissue. The cones are hydrophilic, resulting in absorption of water and in a softer feel. They generate more collagen formation, due to the chemical interaction with the tissues, as well as the physical design of the device. A stronger soft tissue support is the result. The cones are absorbed over 8–10 months, with 50% of the device volume being absorbed in approximately five months (Fig. 28.5).
Current status of barbed sutures for cosmetic and wound closure applications
A bi-directionally barbed suture has many barbs serially placed along its length, changing directions somewhere near the suture mid-point, in order to create a mirror image array of barbs in the opposite direction (Figs 28.6, 28.7
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 circle 26 mm.
circle 26 mm.