INITIAL ASSESSMENT OF WOUNDS
I. EXAMINE ETIOLOGY OF THE WOUND AND ASSESS FACTORS THAT PROVIDE THE FOUNDATION FOR WOUND HEALING
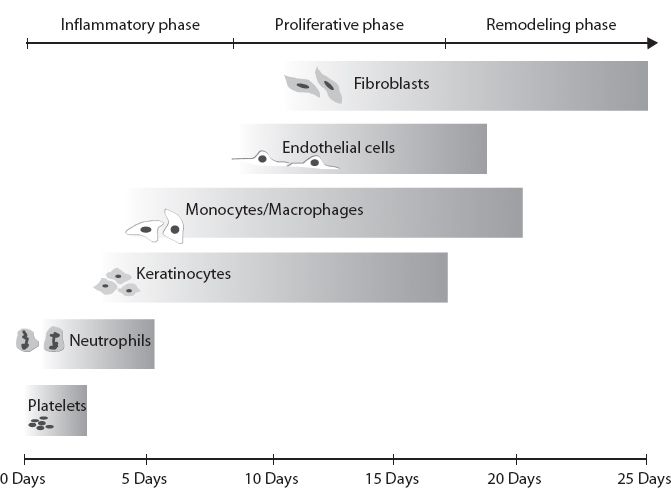
A. Acute versus chronic (see Fig. 2-1)
1. Origin and duration of wound
a. Traumatic versus atraumatic
i. Zone of injury is larger in high- versus low-impact traumas
ii. Assessment of other associated injuries
b. Timing: Injuries that are closed after 6 to 8 hours of remaining open have increased rate of infection.
c. Extent of contamination
i. Antibiotics are not needed for most wounds unless they demonstrate signs of active infection (e.g., cellulitis in chronic venous stasis ulcers).
ii. Bite wounds are always contaminated and have a high likelihood of infection.
a) Assume that the contamination is polymicrobial, and always treat with antibiotics that cover Gram-positive and anaerobic organisms (e.g., ampicillin/sulbactam or amoxicillin/clavulanate, ciprofloxacin + clindamycin if allergic to penicillin).
b) Bacteria specific to wounds
1) *Human bite wounds are contaminated by Eikenella corrodens S.aureus, Eikenella corrodens and anaerobes.
2) *Cat bite wounds are also contaminated by Pasteurella multocida
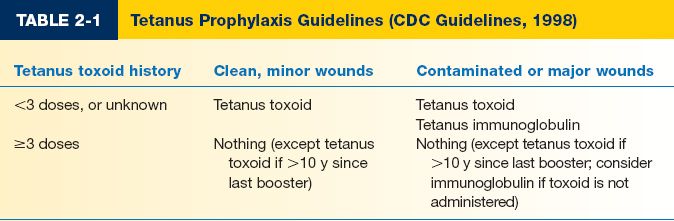
iii. Tetanus prophylaxis (see Table 2-1)
d. Size of wound
i. Extent of exposed tissue: Dermis versus subcutaneous tissue versus fascia versus muscle versus bone
a) >85% chance of osteomyelitis in wounds with exposed bone
2. Assessment of patient local and systemic factors
a. Presence of ischemia–reperfusion injury
b. Hypoxia in the wound bed
c. Bacterial load of the wound
i. Contaminated: Bacteria present without proliferation
ii. Colonized: Bacteria present and proliferating but without causing host response.
iii. Critically colonized: Bacteria present, proliferating, and causing host response, but not enough to overcome host’s resistance.
iv. Infected: Expanding bacterial counts that have overcome the host’s ability to respond.
II. PHYSICAL EXAM
A. General assessment
1. Overall health of the patient
2. Quality of tissue surrounding the wound
______________
*Denotes common in-service examination topics
Figure 2-1. The phases of wound healing.
a. Presence/absence of
i. Radiation-induced chronic skin changes
ii. Edema
iii. Color: Dependent rubor versus erythema
iv. Induration/focal fluid collections
v. Hemorrhage
vi. Foreign bodies
vii. Other wounds in the area
3. Condition of wound bed
a. Location: Evaluate the area for excess pressure or dependent positioning
b. Depth: Evaluate for damage to surrounding structures, including blood vessels, nerves, bone, muscle, and subcutaneous tissues
c. Characteristics of wound bed
i. Amount of granulation tissue versus fibrinous exudate
ii. Odor
iv. Foreign bodies
v. Sinus tract/tunnel formation
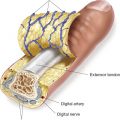
4. Neurosensory exam
a. Gross sensation based on dermatomes involved
b. Two-point discrimination: Normal two point: <5 mm
c. Vibration sensation
5. Vascular exam
a. The presence of both palpable peripheral pulses and Doppler signals in vascular territories adjacent to the wound
b. Temperature of extremity or digit
c. Skin changes consistent with venous stasis, peripheral arterial disease, and lymphedema
III. LABORATORY/RADIOGRAPHIC TESTING
A. Complete blood count (CBC): Evaluate for elevated white blood cell (WBC) count and anemia
B. Albumin
1. 2.8 to 3.5 g/dL: Mild malnutrition
2. 2.1 to 2.7 g/dL: Moderate malnutrition
3. <2.1 g/dL: Severe malnutrition
C. Erythrocyte sedimentation rate and C-reactive protein: May signal the presence or recurrence of osteomyelitis, but are nonspecific inflammatory markers that may be elevated in any pro-inflammatory state, so should be interpreted in the context of the entire clinical picture.
D. Hemoglobin A1C
E. Creatinine
1. Renal failure may predispose patients to chronic wounds and poor wound healing.
2. Calciphylaxis is an important underlying cause of chronic wounds in patients with end-stage renal disease.
F. Plain films: Assess for fractures, orthopedic plates/screws, foreign bodies, and osteomyelitis
G. Computed tomography (CT): Assess for abscesses, chronic sinuses, extent of wound, and involved structures
H. Three-phase technetium bone scan: Radioactive study designed to indicate areas of abnormal bone metabolism or remodeling.
I. Magnetic resonance imaging (MRI): To evaluate the extent of osteomyelitis, especially if spine is involved
J. Ankle–brachial indices
1. >1.2: Calcified vessels (e.g., diabetes)
2. 0.9 to 1.2: Normal
3. 0.5 to 0.9: Mixed arterial/venous disease
4. <0.5: Critical stenosis, symptomatic claudication
5. <0.2: Ischemia and gangrene
K. Angiography: To evaluate the extent of vascular disease
1. If there is evidence of significant peripheral vascular disease, wounds should not be debrided until revascularization procedures are complete to optimize wound healing.
a. Exception: Wounds must be debrided regardless of vascular status if there are signs of overt infection (e.g., “wet” suppurative gangrene).
L. Biopsy/cultures
1. Help target antibiotic regimens and durations.
2. Evaluate for malignancy for atypical or chronic nonhealing wounds.
3. Quantification of bacterial colonies helps in diagnosis and in following progression of treatment.
DEBRIDEMENT
I. SURGICAL, ENZYMATIC (COLLAGENASE), MECHANICAL (VERSAJET, WATERPIK), AND AUTOLYTIC
A. Reduces bioburden by removing inflammatory component of wound, biofilms, fibrinous tissue, which contains cytotoxic mediators that inhibit wound healing.
1. Promotes wound healing by converting a chronic wound into an acute wound to promote keratinocyte migration.
2. Eradicates biofilm and reduce bioburden in wounds with exposed plates or foreign bodies.
B. Vital structures (e.g., nerve, tendon, bone, and vessels) should not be debrided whenever possible unless gross infection or ischemia is present.
C. Complete debridement with irrigation and application of appropriate dressing.
DRESSINGS
I. GOALS
A. Protect the wound from the external environment and mechanical forces.
B. Absorb secretions/maintain a clean environment.
C. Promote granulation tissue formation and reepithelialization: Moist environment leads to increased granulation tissue formation and tissue reepithelialization as compared with dry environment.
D. Optimize patient comfort.
II. TYPE OF DRESSINGS
A. Nonocclusive dressings (e.g., Gauze)
1. Permeable to both gas particles and fluids
2. “Wet to dry” dressing
a. Allowing the gauze to dry prior to removal results in mechanical debridement of the wound during each dressing change.
b. Removal of the dry gauze also creates a mild pro-inflammatory state, which can inhibit wound healing.
c. Coarse gauze provides greater debridement compared with fine gauze.
3. “Wet to wet” dressing: Used over exposed tendon, bone, and neurovascular structures to minimize desiccation.
B. Semiocclusive dressings (e.g., Tegaderm)
1. Sheet dressings that are impermeable to fluids but allow passage of gas molecules.
2. Usually used to cover graft donor sites to keep area moist.
3. Must be cautious in using on areas of thin/fragile skin.
4. Should not be used in contaminated wounds.
C. Occlusive dressings
1. Hydrogel (e.g., Aquasorb and Hydrosorb)
a. Composed of complex polysaccharides, nonadhesive
b. Use in wounds with mild, superficially exudative regions and in painful wounds.
c. Rehydrate wounds and maintain moisture independent from the moisture that is inherently present in the wound.
d. Can be used in infected wound beds.
2. Hydrocolloids (e.g., Duoderm)
a. Comes in paste, powder, and sheet forms
b. Fully adhesive, minimally absorptive
c. Cannot use in infected wounds
d. Induces autolytic debridement within wound
e. Use in mild, superficially exudative wounds
a. Usually composed of nonadhering polyurethane
b. Highly absorptive, but nonhydrating
c. Use in moderately to heavily exudative wounds
4. Alginates (e.g., Algiderm)
a. Derived from seaweed
b. Comes in ribbon/rope forms
c. Can absorb 20× the dry weight of the dressing
d. Use in highly exudative wounds
D. Antimicrobial dressings
1. Silver-coated or -impregnated dressings (e.g., Silverlon)
2. Xeroform: 3% bismuth tribromophenate–impregnated gauze
E. Negative pressure wound therapy
1. “Wound vac” therapy
2. Consists of using a sponge, occlusive dressing, and vacuum
a. Reduces edema
b. Removes exudates from leaky blood vessels/lymphatic channels to improve oxygen diffusion
c. Removes harmful enzymes and inflammatory mediators
3. Most commonly used in
a. Venous stasis ulcers
b. Lymphatic leaks
c. Diabetic wounds
4. *Must not use over
a. Normal skin
b. Infected tissues
c. Tissues harboring malignant cells
d. Inadequately debrided wounds
e. Neurovascular structures
SURGICAL WOUNDS
I. CLASSIFICATION OF SURGICAL WOUNDS
A. Clean (class I): Nontraumatic, no entry into respiratory, gastrointestinal (GI), genitourinary (GU) systems prior to incision, no break in sterile technique (<2% risk of infection).
B. Clean–contaminated (class II): Nontraumatic, minor breaks in sterile technique, entry into GU, GI, and/or respiratory tracts, but without significant spillage (<10% risk of infection).
C. Contaminated (class III): Traumatic, may include gross entry and spillage from GI or GU systems, involves grossly infected tissues/fluid (~20% risk of infection).
D. Dirty (class IV): Traumatic, dirty wound, significant devitalized tissue, fecal matter, foreign bodies, evidence of perforated viscus, and inflammation (40% risk of infection).
II. GENERAL CONSIDERATIONS WHEN CREATING INCISIONS AND FOR WOUND CLOSURE
A. Type of skin and location on the body
1. Specific areas are prone to scar widening and hypertrophy (e.g., shoulder/sternal areas), whereas others tend to heal more favorably (e.g., eyelid and dorsum of the hand).
2. Hair-bearing skin: Scalp incisions are typically beveled to allow for hair growth after incision has healed by avoiding disruption of the hair follicles.
3. Extremity
a. Longitudinal incisions are preferred to avoid crossing joint surfaces to minimize tension and lessen the chance of mobility-limiting scar contracture.
b. Excisional and incisional biopsies should always be oriented longitudinally in order to prevent later morbidity and complexity if additional resection and reconstruction is required (e.g., sarcoma).
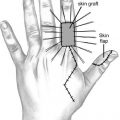
4. Hand incisions.
a. Mid-axial or volar zigzag (Bruner) incisions are preferred to approach the digit volarly.
b. S-shaped, C-shaped, or curvilinear incisions are preferred to approach the digit dorsally.
B. Direction and length of the incision
1. Langer lines of tension (relaxed skin tension lines): Incisions that are able to be planned should be made parallel to the relaxed skin tension lines.
C. Surgical technique
1. Minimize damage to skin edges with atraumatic technique
2. Debridement of necrotic or foreign material
3. Tension-free closure
4. Wound edge eversion
5. Placement of suture that should not leave permanent suture marks
6. Prompt removal of sutures
a. Face: 5 to 7 days
b. Hand/foot: 10 to 14 days
c. Trunk/breast: 7 to 10 days
III. TYPES OF CLOSURE
A. Primary closure: Tissues are reapproximated (using sutures, staples, etc.) on initial presentation.
1. Edges must be under minimal tension
2. Wound cannot be infected
a. Bacterial counts of >105 CFU/g of tissue heal very poorly without debridement.
b. β-Hemolytic streptococci can inhibit wound healing at concentrations >103 CFU/g of tissue.
B. Secondary intention closure: Wound heals with time through accumulation of granulation tissue, usually with frequent dressing changes.
C. Delayed primary closure: Wound initially heals through secondary intention. Once wound bed is clean and under minimal tension, wound edges can be reapproximated using primary closure techniques.
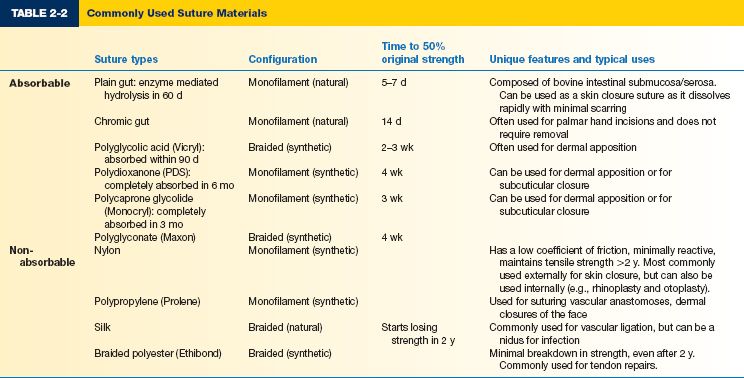
IV. CLOSURE MATERIALS (SEE TABLE 2-2)
A. Suture
1. Classified as absorbable versus nonabsorbable; monofilament versus braided; synthetic versus natural
a. Absorbable
i. Lose at least 50% of strength in 4 weeks.
ii. Often used in children to avoid suture removal.
b. Non-absorbable: Permanent, body induces a cell-mediated reaction around the suture which eventually encapsulates the suture.
c. Monofilament versus braided: Braided sutures are easier to work with, but have slightly increased risk of infection.
d. Synthetic versus natural: Silk and gut are the only natural sutures available, the rest are synthetic.
B. Staples
1. Quick closure
2. Good for hair-bearing regions
3. Use forceps to initiate wound eversion and staple in place
C. Surgical adhesives
1. Cyanoacrylate (Dermabond)
a. Used in conjunction with a proper closure initiated by suture material, which is under minimal tension.
b. Pros: Decreased time for closure, improved cosmetic outcome, possible decreased risk of infection due to decrease in suture use.
c. Cons: Must have a tension-free closure, must not be used on mucosal surfaces.
D. Surgical tapes. Steristrips: Can be used in conjunction with sutures or alone if the closure is completely tension free.
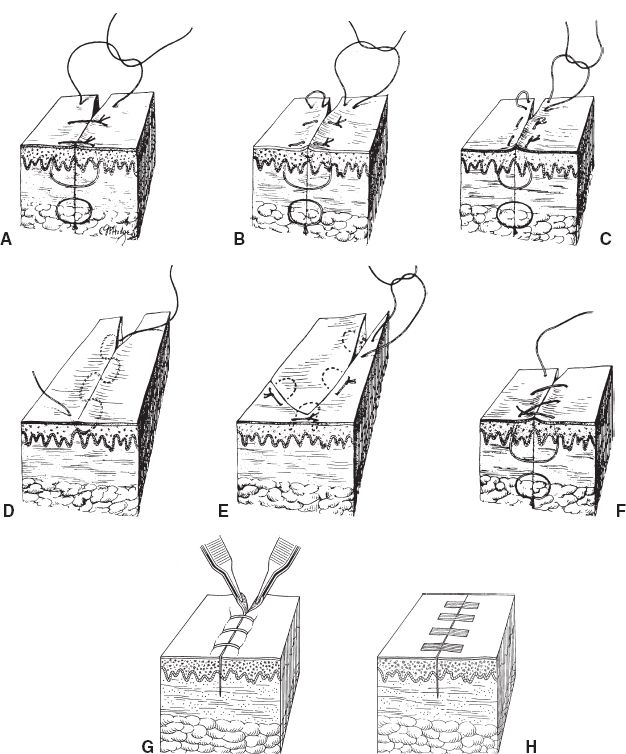
V. METHODS OF WOUND CLOSURE (SEE FIG. 2-2)
A. Simple interrupted: Needle is placed perpendicular to the skin and drawn into the targeted layers of tissue on one side, then out through the same layers/levels of tissue on the opposite side, then tied in place.
1. The needle pathway allows the width of the suture at the base to be wider than at the epidermal entrance to allow eversion of the skin edges.
2. Place sutures 5 to 7 mm apart and 1 to 2 mm from the skin edges to allow for appropriate wound closure.
Figure 2-2. A: Simple interrupted closure. B: Interrupted vertical mattress pattern. C: Interrupted horizontal mattress pattern. D: Running subcuticular (intracuticular) sutures. E: Half-buried horizontal mattress (applicable in corners). F: Simple running (“over-and-over”) suture. G: Stapled closure. H: Steristrips (adhesive tape).
B. Vertical/horizontal mattress suture
1. Good for glabrous skin and wounds under tension.
2. Horizontal mattress causes more hypoxia to tissues than vertical mattress.
C. Subcuticular: Avoids marks on the external surface of the incision to result in a more favorable scar; left in place for 2 to 3 weeks if permanent suture is used.
D. Running suture: Best used when wound edges are already somewhat approximated, fast closure. Use locking running stitch if hemostasis is needed.
PEARLS
1. Antibiotic ointments (e.g., Bacitracin) should only be used for 2 to 3 days as patients can develop hypersensitivity and rash that may be mistaken for cellulitis/infection if used for prolonged periods of time.
2. Absorbable suture should be used in children whenever possible, or when suture removal is anticipated to be difficult or may disrupt closure.
3. Wounds should be examined at regular intervals, and wounds that fail to heal or improve over several weeks should be reassessed for potential barriers to healing such as inappropriate dressings, presence of infection or malignancy, need for additional debridement, and need for more complex reconstruction (graft or flap coverage).
QUESTIONS YOU WILL BE ASKED
1. Describe the classification of sutures and what factors of a wound/incision affect the choice of suture.
Sutures are classified as absorbable versus nonabsorbable, natural versus synthetic, and braided versus monofilament. The suture chosen should effectively minimize tension on the closure, promote eversion of the skin edges, and remain in place for the optimal length of time necessary to maintain a strong and durable closure while minimizing the body’s inflammatory response to the suture itself to optimize the appearance of the scar.
2. Describe the timing of suture removal for the extremities, face, and trunk. Extremities: 10 to 14 days; face: 5 to 7 days; trunk/breast: 7 to 10 days.
3. What are the contraindications to wound vac therapy?
Do not use a wound vac over normal skin, infected tissues, tissues harboring malignant cells, inadequately debrided wounds, or directly on top of neurovascular structures.
4. What dressings are good for highly exudative wounds?
Alginates and foam (e.g., Mepilex) are good for highly exudative wounds.
5. Describe the treatment of animal/human bite wounds.
Bite wounds should be washed out aggressively and thoroughly on presentation given the predisposition of such wounds for infection. If closure is needed, tissues should be loosely approximated to allow for egress of debris and infected fluid. Antibiotics that provide coverage against anaerobic and Gram-positive organisms should be prescribed. Patients should be followed closely to monitor for signs of infection.
Recommended Readings
Leach J. Proper handling of soft tissue in the acute phase. Facial Plast Surg. 2001;17(4):227-238. PMID: 11735055.
Singer AJ, Quinn JV, Hollander JE. The cyanoacrylate topical skin adhesives. Am J Emerg Med. 2008;26(4):490-496. PMID: 18410821.
Ueno C, Hunt TK, Hopf HW. Using physiology to improve surgical wound outcomes. Plast Reconstruct Surg. 2006;117(7 Suppl):59S-71S. PMID: 16799375.
< div class='tao-gold-member'>