Fig. 31.1
The anatomy of the internal nasal valve showing the relationship of the most anterior portion of the inferior turbinate, the caudal aspect of the upper lateral cartilage, and the nasal septum (Reprinted from Schlosser and Park [8], February 1999, with permission from Elsevier). The image required enhancement and adaptation for final publication
Structural Anatomy
The majority of the nasal septum is composed of bone and cartilage covered on both sides by mucosal epithelium. The most caudal portion of the nasal septum, the membranous septum, is covered by skin with associated hair follicles, vibrissae, and it is continuous inferiorly with the columella. By pushing the membranous septum laterally in either direction, the most caudal portion of the nasal septal, or quadrangular, cartilage may be identified. A transition of the epithelium from hair-bearing skin to mucosa occurs near the junction of the membranous septum and the nasal septal cartilage. The nasal septal cartilage provides structural support to the nasal dorsum. Lack of support in this area will lead to a saddle nose deformity or supratip depression. The anterior nasal spine of the maxilla and the maxillary crest provide an inferior attachment for the nasal septal cartilage at or near the midline. Unilateral deficiency of the nasal spine and maxillary crest on one side, as can be found in unilateral cleft palate, may be associated with deviation of the cartilaginous septum away from the deficient side [9].
The perpendicular plate of the ethmoid bone lies posterior and superior to the nasal septal cartilage. It continues further superiorly to join the skull base at the thin cribriform plate of the ethmoid bone. The vomer sits posterior and inferior to the septal cartilage. Inferiorly, the vomer is attached to the hard palate by the maxillary crest and the crest of the palatine bone. The posterior superior aspect of the vomer is attached to the anterior face of the sphenoid bone in the midline. Aeration of the sphenoid bone extending into the posterior septum can occur. Spurs and bony septal deflections are prone to occur near the junction of the vomer and the perpendicular plate of the ethmoid bone. The actual amount of contact between these two bones is dependent upon the amount of intervening nasal septal cartilage. The frontal bones also make small contributions to the bony portion of the nasal septum.
Blood Supply
The nasal septum has a robust submucosal blood supply which receives contributions from the internal carotid artery by way of the anterior and posterior ethmoidal arteries as well as from branches of the external carotid artery. These include the sphenopalatine artery via the posterior septal artery, a contribution from the greater palatine artery traveling through the incisive foramen, and the facial artery from the septal branch of the superior labial artery. Kiesselbach’s plexus (Fig. 31.2) [10], a confluence of superficial terminal arterial branches along the caudal nasal septum, is a common location for anterior epistaxis [11].
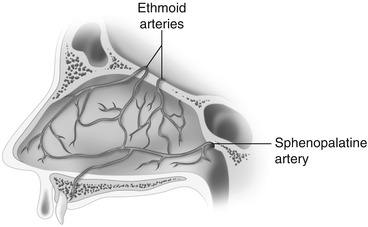
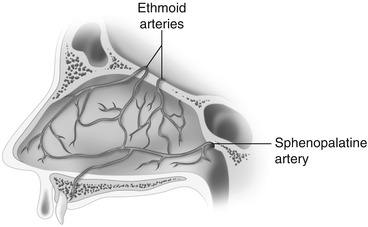
Fig. 31.2
The arterial blood supply and the confluence of blood vessels in Kiesselbach’s area of the nasal septum (Image reprinted with permission from Watson [10]. University of California, San Diego, School of Medicine). The image required enhancement and adaptation for final publication
A bloodless dissection along the nasal septal cartilage can be accomplished by entering the subperichondrial plane. This is possible because the nutrient supply to the chondrocytes within the cartilage occurs via diffusion down the concentration gradients from the vascular perichondrium through the avascular extracellular matrix of the cartilage [12].
Anatomy of the Inferior Turbinates
The inferior turbinates consist of a solitary bone, the inferior nasal concha, which is covered with a thick mucous membrane. This membrane contains cavernous tissue which is active in the nasal cycle, a periodic swelling of the nasal mucous membranes. In addition to its physiologic role in regulating humidification and nasal airflow, the nasal cycle may contribute to the perception of nasal airway obstruction, and often individuals with significant nasal septal deviation will have a heightened awareness of their own nasal cycle.
Innervation
The nasal cavities including the septum and the inferior turbinates have a complex pattern of innervation related to the multiple functions of the mucosal lining of the nose. The superior portion of the nasal cavity including a portion of the superior nasal septum is covered with olfactory epithelium which transmits neurons through the olfactory bulbs along CN I. General sensory innervation from the remaining nasal cavity is transmitted by way of branches of CN V1 and V2. The anterior and superior portions of the nasal septum are innervated by branches of V1 via the anterior ethmoidal nerve which arises as a branch of the nasociliary nerve within the bony orbit, while the inferior and posterior portions of the nasal septum and the inferior turbinates are supplied by branches of V2 arising from the sphenopalatine and greater palatine nerves [12]. Autonomic innervation of the nasal cavity occurs along branches of V2 which distribute both postganglionic parasympathetic and postganglionic sympathetic fibers.
Indications
The evaluation of a patient for septal and/or turbinate surgery starts with a thorough history and physical exam evaluation. Some patients will present with a diagnosis already established or suggested by a referring physician that needs confirmation. However, most will be seen with a chief complaint of nasal obstruction that then requires a full otolaryngologic evaluation. In addition to a standard medical history, the physician should specifically ask questions regarding time onset, laterality of symptoms, time variation (intermittent vs. constant), epistaxis, facial pain or hypesthesia, improvement with prior use of nasal medications or antihistamines, as well as symptoms suggestive of atopy (e.g., seasonal variation, environmental triggers, sneezing, rhinorrhea, ocular symptoms, eczema). The past medical and social history should include an inquiry regarding the history of preceding or ongoing illness, recurrent sinusitis, confirmed diagnosis of environmental allergies, facial trauma, abuse of topical decongestants, or intranasal illicit drug use. The differential diagnosis for a patient with nasal obstruction is outlined in Table 31.1.
Table 31.1
Differential diagnosis of nasal obstruction
Structural/anatomic |
Nasal septal deviation |
Internal nasal valve collapse |
External nasal valve insufficiency |
Nasal tip ptosis |
Nasal turbinate hypertrophy |
Septal perforation |
Empty nose syndrome |
Neoplastic |
Malignant |
Benign |
Inflammatory |
Nasal polyposis |
Rhinosinusitis |
Allergic rhinitis |
Nonallergic rhinitis |
Hormonal (e.g., rhinitis of pregnancy, hypothyroidism) |
Primary vasomotor rhinitis |
Rhinitis medicamentosa |
Granulomatous and autoimmune disease |
Granulomatosis with polyangiitis (Wegener’s granulomatosis) |
Sarcoid |
Churg-Strauss syndrome |
Foreign body |
Medications |
Intranasal illicit drug use |
Congenital |
Choanal atresia (unilateral or bilateral) |
Nasolacrimal duct cyst |
Encephalocele |
The physical exam is a key aspect of the initial evaluation. The exam should start with close attention to the external anatomy looking for potential areas of structural deficits contributing to the patient’s symptoms of nasal obstruction. While patients may present with a chief complaint of functional limitations, they may also have further expectations regarding cosmetic outcomes from nasal surgery. It is best to establish up front the purpose of a septoplasty in order to avoid any misunderstandings about the ultimate goals of therapy.
Major external structures to examine include the nasal tip, nasal dorsum, and nasal valve regions. Nasal tip ptosis is more common with advanced age and requires open rhinoplasty techniques to correct. Severe dorsal septal deflections as well may require open techniques. One of the initial key elements in deciding on a septoplasty approach is to first determine if the patient would be better served by an open septorhinoplasty. Most importantly, the nasal valve region should be examined carefully since this is a major reason for failed outcomes after surgery. The most traditional maneuver used to evaluate nasal valve collapse is the Cottle maneuver. The examiner places his or her hand along the nasolabial groove to provide tension and pull the nasal wall lateral while the patient takes an inspiratory breath through the nose. A subjective improvement in nasal airflow can indicate potential internal nasal valve collapse [13]. Becker et al. [2] performed a large review of 577 patients who underwent septoplasty looking at outcome failures and identifying risk factors in patients who required revision surgery. Multivariate analysis confirmed that patients who had nasal valve surgery in conjunction with their primary septoplasty were significantly less likely to undergo revision surgery. For those that did require revision septoplasty surgery, 40 % had nasal valve surgery done at the time of the second procedure [2]. Overall, there is a lack of strong primary evidence in the literature regarding outcomes in nasal valve surgery with many uncontrolled observational studies. This is an area for future research as cited by the most recent clinical consensus statement by the American Academy of Otolaryngology – Head and Neck Surgery (AAO-HNS) [14].
The examination proceeds to anterior rhinoscopy after completing the external nasal examination. Direct anterior rhinoscopy with a nasal speculum provides a working perspective of the anterior nasal anatomy. Attention is first brought to the caudal septum and the degree of deformity that may exist. This portion of the examination requires direct visualization with the speculum removed and while inserted gently in the nose. Palpation is also useful to determine the structural pathology present in this region. The anterior half of the septum and particularly the nasal valve region can be visualized well along with the inferior turbinates. This should be done before instilling any decongestant solution so as to appreciate a true understanding of the degree of visible nasal obstruction. While posterior septal deflections can be partially viewed using adequate illumination along with appropriate nasal decongestion, a complete examination for complaints of nasal obstruction typically necessitates a formal nasal endoscopy. Both rigid and flexible techniques are acceptable with flexible endoscopy allowing for further evaluation of the lower pharynx and larynx at the same time if clinically indicated. Flexible instrumentation may also be necessary for patients with severe septal deflections in order to fully visualize the middle meatus and posterior anatomic structures. Most importantly, a nasal endoscopy examination will provide a complete evaluation of the entire nasal cavity to identify any synchronous pathology such as nasal polyps, rhinosinusitis, or nasal tumors.
Clinical indicators developed by the AAO-HNS for septoplasty surgery include nasal airway obstruction, frequent epistaxis, atypical facial pain of nasal origin (rhinogenic or contact point headaches), and deformity that prevents surgical access for other nasal procedures including functional endoscopic sinus surgery and skull base operations [15]. Clinical indicators outlined by the AAO-HNS for inferior turbinate surgery include a history of chronic nasal obstruction, failure of directed medical management, failure of treatment of rhinitis medicamentosa, or symptoms of OSA [16]. Septal deviation has been identified as a risk factor in patients with epistaxis. O’Reilly et al. [17] studied a group of 54 patients with recurrent epistaxis compared to controls. They demonstrated a significant association with nasal septal deviation (p <.001) [17]. Another study determined that 16/75 patients with intractable epistaxis had a septal deviation near the site of bleeding [18]. Patients with post-traumatic epistaxis are also more likely to demonstrate an external nasal deformity [19]. Contact point or rhinogenic headaches have been a topic of interest for some time with many studies published on the topic. Harrison and Jones [20] completed a systematic review of the topic in 2013. They identified 65 potential studies with 22 included in the final analysis. They concluded that nasal contact points can be identified in many asymptomatic subjects. Also, the literature that supports the removal of contact points is mostly retrospective and uncontrolled in design and does not consistently use the International Headache Society criteria [20]. For now, it is a continuing topic of clinical interest and further research. Septoplasty can be necessary as an adjunct procedure for surgical access during endoscopic sinus procedures. Rudmik et al. [21] reviewed 221 patients undergoing endoscopic sinus surgery. All patients had chronic rhinosinusitis (CRS) without nasal polyposis. Approximately half (108/221) required a septoplasty. Compared to those patients who did not have septal surgery, concurrent septoplasty did not appear to affect surgical outcomes (CRS-related HRQoL) [21]. Van Lindert et al. [22] reviewed 185 patients undergoing endoscopic transsphenoidal pituitary surgery. About 50 % of patients had a deformity of the nasal septum or anterior septal spine. Overall, 16 patients (8.6 %) required some form of surgical correction to allow for anatomic access to the sphenoid sinus [22]. Nasal surgery is playing a growing role in the treatment of patients with obstructive sleep apnea (OSA). Overall, studies to date have demonstrated limited efficacy of nasal surgery in improving objective polysomnographic measures of OSA disease. However, studies have shown improvement in subjective measures including snoring, quality of life, and sleepiness [23–28]. It should be noted, though, that the literature is limited to uncontrolled case series and there is continued interest in regard to the use of nasal surgery in multilevel sleep apnea surgery. The efficacy of nasal surgery in improving CPAP compliance use has also been investigated in the literature with promising results [29–31].
For septoplasty surgery, the AAO-HNS clinical indicators [15] state that nasal endoscopy and CT scan are optional tests in the preoperative period. We would encourage the use of nasal endoscopy in the preoperative workup as emphasized above in our discussion. Radiologic testing is not typically done routinely for every patient presenting for nasal obstruction especially given the increasing concerns regarding the risk of iatrogenic radiation exposure. Karatas et al. [32] did a study of patients who underwent septoplasty with preoperative screening CT scan. The most common findings were concha bullosa, inferior turbinate hypertrophy, and chronic sinusitis [32]. Given the cost and inherent risks of CT, it is most appropriate to reserve this testing for patients with specific clinical indications. For nasal turbinate surgery, the AAO-HNS [16] lists an allergy evaluation, rhinomanometry, and acoustic rhinometry as optional tests in the preoperative setting. Allergy testing is appropriate when clinically suspected and the patient does not respond to conventional medical therapy. The use of rhinomanometry and acoustic rhinometry in the conventional ambulatory clinical setting is limited and typically reserved for research purposes.
Surgical Technique
Preoperative Decision Making
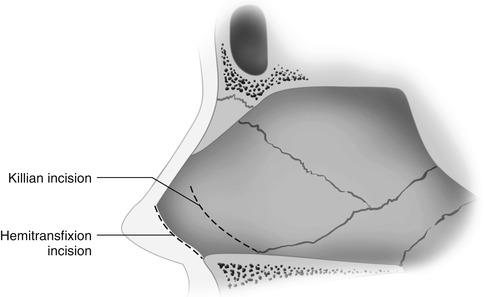
While precision technique and experience are critical to a successful surgical outcome, strategic preoperative planning is the most important step in the care of these patients. The nasal surgeon should not prescribe to any one septoplasty “style.” The vast array of different septal pathology demands an armamentarium of surgical approaches and techniques to manage the individual patient. While a classic submucous resection is certainly no longer necessary for every patient, at the same time, an overly conservative septoplasty can leave inadequate results. The first step after performing your evaluation is to decide if the patient can be approached using an endonasal vs. open septorhinoplasty technique. Conditions that may necessitate an open approach include severe dorsal septal twisting or deviations contributing to airway obstruction, nasal tip ptosis, severe caudal septal deflections, and deficient nasal valve architecture requiring open cartilage grafting. Standard incisions involve either a hemitransfixion or Killian’s incision and should be adapted to the individual patient (Fig. 31.3) [10].
Surgical Preparation
Surgery can be performed using either general anesthesia or local techniques with/without sedation. After anesthesia induction, a throat pack is typically placed to prevent the collection of blood in the hypopharynx and stomach. However, there is no evidence that this reduces postoperative nausea and vomiting. Recent work suggests it may be more efficacious to remove blood using an orogastric tube at the end of surgery [33]. The septum is prepped in the same fashion regardless of whether the patient receives general anesthesia. The two main purposes of a septal injection are hydrodissection and vasoconstriction. This is critical and the first technique taught to anyone learning the art of septal surgery. A topical solution of oxymetazoline (0.05 %) is placed in the nasal cavity bilaterally using nasal pledgets or cotton balls. Next, 1 % lidocaine with 1:100,000 solution is injected using a 25-gauge needle or smaller along the septum in a subperiosteal and subperichondrial plane. A stepwise injection technique is used where the edge of the dissection bleb from the prior injection is used as a starting point to develop the next area of hydrodissection. The oxymetazoline pledgets are then replaced while scrubbing and prepping the patient to allow time for adequate effect. Higgins et al. [34] completed a systematic review of topical vasoconstrictors used in nasal surgery. They emphasized safe and judicious use of these medications and recommended avoiding topical phenylephrine if possible along with cautious use of topical cocaine [34]. Beta-blockers should be avoided to treat hypertension during cases using alpha adrenergic agonists to avoid unintended development of pulmonary edema [35, 36].
The efficacy of hydrostatic injections is controversial. Studies do demonstrate that the perichondrial layer provides the largest amount of tensile strength and thus a subperichondrial dissection is logical and favored [37]. However, the technique of hydrodissection has been questioned. A cadaveric study by Dubach et al. [38] demonstrated only 25 % (5/20) of experimental cases with injections performed in the correct dissection plane. Most injections were either in the perichondrium itself or supra-perichondrial [38]. This may be an area for further investigation and research.
Submucous Resection
The traditional submucous resection of the septum dates back over half a century with the instrumentation and surgical technique mostly unaltered over time. After appropriate surgical preparation, the procedure begins with one of the traditional incisions (Fig. 31.3). Typically, for a classical submucous resection, a Killian’s incision is made on the left side of the septum. This approach is generally taken due to the predominance of right-handed surgeons. However, a right-sided incision can be made as well if deemed necessary for the particular clinical circumstance. A no. 15 blade knife is used to incise through the mucosa and perichondrium. This is a key part of the procedure, and much time will be saved later in the procedure if some additional patience and attention are paid to this step. If the dissection starts in the incorrect surgical plane, the operation will inevitably be more difficult with an increased likelihood of mucosal tears and loss of subsequent flap integrity. The proper plane of dissection is determined by visualization and tactile feedback with the instrumentation. With modern-day halogen headlights used in the operating room, the septal cartilage will reflect back almost a slight bluish hue that is bright white in color. With proper vasoconstriction, the subperichondrial plane should be avascular with minimal bleeding. Excessive bleeding from inside the flap indicates that the dissection may be progressing at the incorrect depth. It is even acceptable to begin dissecting just slightly into the superficial layer of the cartilage itself to ensure that one is deep enough within the plane of dissection and then back off into the proper layer. In an atraumatic patient with no prior nasal surgery, the subperichondrial plane will dissect quite easily also providing an indicator of a correct surgical dissection level. After incising with the scalpel, a sharp elevator is used such as a Cottle elevator or Tebbetts™ septal elevator. Carefully, the flap is elevated using this instrumentation until an adequate length of flap is raised to allow for the introduction of a nasal speculum in a vertical orientation. At this point, one can use a less aggressive instrument such as a Freer elevator if preferred or continue with a sharp elevator if needed to continue flap dissection. The dissection is carried posterior to the bony-cartilaginous junction. There is usually a small area of flap adhesion at this line that requires some careful elevation. Once dissection proceeds to the bone, the surgeon needs to reconfirm if he or she is working in the correct plane. At any point in the dissection, when transitioning between different bones or from cartilage to bone, there is usually a small amount of flap adhesion at these suture lines. As the surgery proceeds along the perpendicular plate of the ethmoid bone, care is taken to avoid dissection near the cribriform plate but high enough so that all areas of structural deviation are addressed. The flap is elevated down to the floor of the nose. The septal flaps may fold over and sit deeply in the groove between the quadrangular cartilage and maxillary crest. Therefore, this area of flap elevation should typically be done last. A Pierce elevator may be useful in this circumstance especially with more inferiorly located spurs. Next, a transcartilaginous incision is created along the caudal septal cartilage. Care is taken to leave at least a 1-cm caudal strut. This can be performed using a scalpel knife or sharp elevator. Typically, an elevator is adequate and less likely to create a contralateral perforation in the mucosa. A contralateral flap is raised on the opposite side similar in fashion to the initial dissection. A long nasal speculum is then inserted fully back to the face of the sphenoid rostrum once the flaps have been fully developed. At this point, a swivel knife can be used to remove a large section of deviated cartilage and set aside for later replacement if necessary. Deviated portions of the perpendicular ethmoid plate and vomer are removed using Jansen-Middleton cutting forceps. Care is taken not to use any torsional force when removing these superior portions of the bone to avoid a CSF leak. Once the superior attachments are free, the lower sections of the bone and spurs can be removed more aggressively using a grasping instrument such as Takahashi forceps. Large 90° oriented spurs that prevented adequate flap elevation earlier in the procedure can now be fractured off the floor of the nose using an elevator and gently teased away from the attached mucosa. Anterior, there is typically a strip of cartilage still in place along the maxillary crest that can be removed using a Freer elevator. Small deviations in the maxillary crest are typically not responsible for symptomatic nasal airway obstruction as opposed to high septal deviations along the nasal valve region. Aggressive removal of the maxillary crest can lead to subsequent postoperative dental anesthesia. Therefore, discretion must be used in judging whether to remove portions of this bone. If necessary, a 4-mm chisel and mallet can be utilized to remove any deviated sections. Care should be taken throughout the procedure to preserve a 1-cm caudal and dorsal strut for structural support and prevention of postoperative nasal tip ptosis and/or dorsal saddle nose deformities. Upon completion of the resection, the amputated cartilage graft can be reformed and flattened using a press and replaced between the flaps. This is generally more important in scenarios where a bilateral opposing septal mucosal tear exists after flap elevation. Care must be taken upon closure to not allow the cartilage graft to “slip” inferior and sit alongside the remaining maxillary crest creating a new postoperative septal deformity. The incision can be closed using absorbable suture such as 4–0 chromic gut. Especially if a cartilage graft was replaced, quilting sutures are recommended using absorbable suture such as 4–0 plain gut with a straight needle to avoid mucosal trauma. Running quilting sutures should be used with caution which can cause strangulation of the septal mucosa if done in a circumferential fashion. Sutures placed in an interrupted fashion can avoid this potential problem. If a mucosal tear does not already exist from the prior dissection, a drainage incision needs to be created posterior-inferior to prevent postoperative hematoma formation. Use a scalpel blade to create a puncture site in conjunction with angled scissors.
Septoplasty
Evolution from the days of Gleason and Watson to the contemporary septoplasty has been slow and stepwise. The modern-day septoplasty emphasizes structural support and tissue conservation. A hemitransfixion incision is typically utilized to open the caudal septum, but some variation starting more posterior is also appropriate depending on the location of the pathology. Again, emphasizing that every septum is unique, thus the surgery should be tailored and adapted to the individual patient. A subperichondrial flap is raised again on the left side typically as with the submucous resection. However, instead of removing the quadrangular cartilage, the bony-cartilaginous junction is identified and divided using the Freer elevator with contralateral flap elevation. At this point, deviated sections of bone are removed using cutting forceps. Since the cartilage is still in place, this dissection takes place in a smaller space. Care must be taken not to perforate the posterior superior flap and injure the middle turbinate. Surgical treatment of the anterior cartilage is an expansive topic with volumes of text written on individual subunits such as the caudal septum. Techniques emphasize different variations of conservative cartilage removal with repositioning of the remaining structural elements. Commonly, an inferior thin strip of cartilage is removed allowing the cartilage to realign into proper position classically known as the “swinging door” technique. Remaining memory might require further scoring using a sharp instrument such as a Freer knife. Curvature can still remain in a severely deviated septum, and many times, it is also prudent to raise a contralateral flap anterior through the hemitransfixion incision fully isolating the anterior cartilage and removing any attachments of the opposing mucosa. Despite cartilage scoring techniques, the contralateral mucosa can remain a barrier to allowing the cartilage to relax into a neutral position. Further suturing may be required to hold the septum in position along the maxillary crest. A caudal septal deviation can be a challenging and vexing problem. If treated through an endonasal septoplasty approach rather than an open rhinoplasty, full bilateral flap elevation is typically necessary. The question at this point is whether to remove the cartilage and replace it with a reformed cartilage graft or try to realign the cartilage in situ. If cartilage segments are removed from the caudal septum, it can be difficult to replace these grafts in an endonasal fashion. Some authors have advocated the use of polydioxanone (PDS) foil (Ethicon Inc, Johnson & Johnson) as an adjunct to septal reconstruction [39–42]. Sections of resected cartilage are laid out on a piece of PDS foil and sutured in place. A second piece of foil can be placed on the opposite side for further support. The graft is then sutured in place between the septal flaps. The incisions are closed in a standard fashion as with a traditional submucous resection.
Endoscopic Septoplasty/Blended Techniques
Endoscopic septoplasty is a newer technique that has come about with the advent of endoscopic sinus surgery. The ideal candidate for a minimally invasive pure endoscopic septoplasty is the patient with an isolated posterior bony spur or anatomic deformity. The area is injected directly with local anesthetic solution to hydrodissect the mucosa off the bone. This is done under direct endoscopic guidance using either a long 25-gauge spinal needle or tonsil needle. A small limited mucosal flap is raised off the spur exposing the bone. The spur can be directly removed using a small diamond burr. Otherwise the section of deformed bone can be fully cut out and isolated with dissection off the contralateral flap. The small mucosal flap is just laid down without any suturing. If done in conjunction with sinus surgery, the middle turbinate can many times be sutured in place against this area for support. A “blended” or “back-and-forth” technique is now becoming more common [43]. A variation of endoscopic septoplasty, the septal incisions are made through a traditional approach, but the endoscope is used between the flaps intermittently throughout the procedure to provide magnified visualization of the posterior structures and assistance in raising flaps in challenging areas.
Traditional Submucous Turbinate Resection
Aggressive partial or complete inferior turbinate resection including the overlying mucosa can lead to long-term complications of atrophic rhinitis or “empty nose syndrome.” This procedure is not advocated by the authors and will not be detailed for that reason. A traditional submucous resection involves first injecting the turbinate in a submucosal fashion along its length on each side using a standard local anesthetic solution used in septal surgery. An incision is made along the anterior two-thirds of the turbinate and a mucosal flap raised along the bone. Cutting instruments such as a Jansen-Middleton forceps or long scissors are used to remove a section of the bone. The flaps are then laid back in position and not typically sutured in place. The turbinates can be outfractured to provide additional expansion of the airway.
Microdebrider-Assisted Turbinate Reduction
Microdebrider-assisted turbinate reduction is widely used today to address inferior turbinate pathology. The technology is readily available during endoscopic sinus surgery cases further lending to its convenience and surgeon comfort with the device. The anterior turbinate head and body are again injected with local anesthetic solution, allowing time to have its effect. Under direct endoscopic visualization, the tip of the blade can be used to make a puncture incision along the anterior head of the turbinate and subsequently raise a small submucosal pocket as far posterior as necessary to address the degree of turbinate hypertrophy. Alternatively, a no. 15 blade knife can be used to make a small anterior incision with a standard Freer elevator then utilized to raise the flap. As the flap is raised, care must be taken not to tear a lengthwise flap or create posterior perforation sites. Various microdebrider blades exist from different manufacturers with some designed specifically for inferior turbinate use. In general, the blade is passed into the pocket with the cutting edge of the blade facing lateral. Debridement is performed posterior to anterior but can move back and forth if necessary. Attention should be paid anterior-superior to the area of the internal nasal valve. The blade needs to be angled superior to reach this area when moving anterior, which can be a critical area of obstruction. The turbinates are then outfractured if deemed necessary.
Radio-frequency Turbinate Ablation
Radio-frequency ablation can be done alone as an office-based procedure or in the same setting as other concurrent nasal surgery. Again, settings for the equipment vary based on the manufacturer. The general principle involves making multiple passes using a needle electrode tip device in a submucosal plane along the length of the turbinate. Energy is delivered through the tip to the surrounding tissue. Care must be taken not to burn the edge of the nasal vestibule when using these devices.