Subfascial Breast Augmentation
Ruth Maria Graf
Maria Cecília Closs Ono
André Ricardo Dall’Oglio Tolazzi
Introduction
The number of breast augmentation procedures has increased over the years (1,2). Along with this increase have come controversies regarding surgical approach, implant selection, and especially the issue of implant plane or pocket plane. There are basically two pocket planes into which to put a silicone implant: above (subglandular) and behind (submuscular) the pectoralis major muscle. Both have advantages and disadvantages.
The subglandular approach gives better projection to the breast and usually fulfills the expectations of patients who want to augment their breasts. In very thin patients, however, this approach ends up with an artificial look of the breasts, with the entire implant contour being visible under the skin. In this type of patient, the submuscular breast augmentation offers more natural results with round implants. It also reduces the incidence of clinically visible capsular contractures, once the pectoralis action helps to prevent the capsular restriction around the implant, and also serves as an anatomic barrier for mild distortions. The submuscular approach has some drawbacks as well. It has more limitations on the volume to be used, because the pocket is a little bit smaller than the subglandular one. In the middle and long term postoperatively, pectoralis muscle action can move the implant when the patient is exercising, which looks unpleasant and can also cause displacements of the implants. Due to muscle action, the implant usually does not follow the breast parenchyma descent, which drops over the implant, resulting in a “double-bubble” appearance.
In order to better compensate for the pros and cons of subglandular and submuscular breast augmentation, we have been using the subfascial approach since 1998. This chapter describes in detail three different accesses for performing a subfascial breast augmentation and discusses some advantages compared with the subglandular and submuscular approaches.
Operative Techniques
Preoperative Markings and Anesthesia
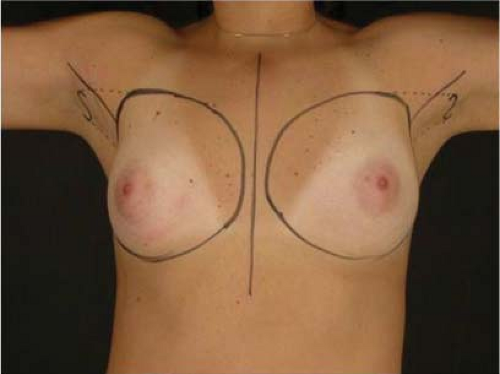
Preoperative markings are done with the patient in the upright position. The limits of the breast pocket are marked, passing at least 1 to 2 cm lateral to the mid-sternum line, not extending laterally to the anterior axillary line, and connecting superiorly at the level of second intercostal space. The natural inframammary fold and the future inframammary crease are marked, considering the nipple-areola complex (NAC) position, the implant base diameter (radius), the subcutaneous thickness, and the skin stretchiness (Fig. 112.1).
The operation can be performed under general anesthesia, epidural, intercostal, or local anesthesia, and sedation. We prefer epidural blockage associated with sedation. Patients are positioned with the arms abducted 90 deg and the dorsum slightly elevated. The incision and pocket limits are infiltrated with a normal saline-epinephrine solution (1:300,000), but the whole pocket area is not infiltrated, to avoid difficulty in dissecting the fascia.
Axillary Access
An S-shaped, 4-cm-long incision is made in the main axillary fold, about 1 cm behind the lateral border of the major pectoralis muscle. It is important never to cross beyond the lateral edge of the pectoralis muscle, keeping the scar hidden in the axilla. Transaxillary breast augmentation can damage lymphatic vessels during subcutaneous tunnel dissection and insertion of the implant into the breast pocket. To minimize lymphatic injuries, a subcutaneous tunnel should be dissected up to the superior lateral border of the muscle, preserving an inferior lateral triangle of soft tissue containing most of lymphatic structures (Fig. 112.2) (3,4).
The pectoralis fascia is incised, and the subfascial breast pocket is dissected with electrocautery. This can be done using an endoscopic retractor or through direct view using long, lighted retractors (Figs. 112.3 and 112.4).
Areolar Access
Periareolar breast augmentation can be performed with or without mastopexy. Skin is usually incised in the lower half of the areolar margin, preserving the upper half as a superior pedicle for the NAC. If a mastopexy is planned, a donut-shaped area of skin is deepithelialized, also preserving the upper half of the dermis. The outer limits of the deepithelialization area are as follows: new superior areola position (point A), 9 to 10 cm from midline (medially), about 12 cm from anterior axillary line (laterally), and 5 to 8 cm from the future inframammary fold (inferiorly). The inferior pole of the breast is dissected in an oblique direction, between the breast parenchyma and the subcutaneous tissue. Once the pectoral fascia is reached, it is incised about the nipple level, and the subfascial pocket is created in all directions up to the marking limits (Figs. 112.5 to 112.7).
Another option of incision is the transareolar approach, which can be indicated for patients with an areolar diameter of at least 3.5 cm. A geometric broken line incision is done horizontally in the areola, merging and not transecting the nipple, without disturbing the lactiferous ducts or mammary gland (5). Dissection of the breast is performed as in the periareolar approach.
Inframammary Access
A 4-cm incision is made in the future inframammary crease. The new inframammary fold and the incision should be carefully planned in order to have a good-quality and well-placed scar. The site of the new inframammary fold and future scar should consider the implant diameter, the subcutaneous
thickness, and the skin elasticity. Gently stretching up the NAC, the new inframammary fold distance from the nipple is marked, adding the implant radius size and the subcutaneous thickness. This distance (nipple–new inframammary fold) usually ranges from 5 to 8 cm. After the skin and subcutaneous tissue are incised, the pectoral fascia is identified, and the subfascial pocket is dissected superiorly (Figs. 112.8 and 112.9).
thickness, and the skin elasticity. Gently stretching up the NAC, the new inframammary fold distance from the nipple is marked, adding the implant radius size and the subcutaneous thickness. This distance (nipple–new inframammary fold) usually ranges from 5 to 8 cm. After the skin and subcutaneous tissue are incised, the pectoral fascia is identified, and the subfascial pocket is dissected superiorly (Figs. 112.8 and 112.9).
Subfascial Breast Pocket Dissection
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree