14 Structural fat grafting
Synopsis
 The concepts of aging are changing, placing more emphasis on volume loss and volume restoration.
The concepts of aging are changing, placing more emphasis on volume loss and volume restoration.
 Fat grafting provides a long-lasting, minimally invasive means to restore volume and rejuvenate the face, hands, or body.
Fat grafting provides a long-lasting, minimally invasive means to restore volume and rejuvenate the face, hands, or body.
 Proper harvesting, refinement, and placement of the fat is essential for consistent results.
Proper harvesting, refinement, and placement of the fat is essential for consistent results.
 The most forgiving area to learn structural fat grafting is the dorsum of the hand and the least forgiving area is the eyelid.
The most forgiving area to learn structural fat grafting is the dorsum of the hand and the least forgiving area is the eyelid.
 Fat grafting can be used to replace tissue lost due to aging, trauma, and/or disease, as well as to rejuvenate and dramatically alter the contours of the face, hands, and/or body.
Fat grafting can be used to replace tissue lost due to aging, trauma, and/or disease, as well as to rejuvenate and dramatically alter the contours of the face, hands, and/or body.
 The future use of adipose-derived stem cells in regenerative medicine and tissue engineering is promising.
The future use of adipose-derived stem cells in regenerative medicine and tissue engineering is promising.
 Numerous aesthetic and reconstructive problems can be addressed with structural fat grafting, but patient selection is very important.
Numerous aesthetic and reconstructive problems can be addressed with structural fat grafting, but patient selection is very important.
 Fat must be harvested gently to preserve its natural architecture.
Fat must be harvested gently to preserve its natural architecture.
 Predictable volume changes are possible when fat is refined and condensed by centrifugation and decanting.
Predictable volume changes are possible when fat is refined and condensed by centrifugation and decanting.
 Centrifugation at 1286 g is considered optimal (Yoshimura) and may enhance fat graft take and prevent long-term atrophy of the transplanted tissue.
Centrifugation at 1286 g is considered optimal (Yoshimura) and may enhance fat graft take and prevent long-term atrophy of the transplanted tissue.
 Oil present after centrifugation can indicate adipocyte destruction as well as the desired separation of oil from fatty components.
Oil present after centrifugation can indicate adipocyte destruction as well as the desired separation of oil from fatty components.
 Growth factors and stem cells have been isolated and appear to be concentrated in the densest portions of centrifuged fat.
Growth factors and stem cells have been isolated and appear to be concentrated in the densest portions of centrifuged fat.
 Frozen or stored fat is not considered viable and should not be used.
Frozen or stored fat is not considered viable and should not be used.
 Fat should be grafted in very small aliquots using multiple passes of the cannula and should not be molded after placement.
Fat should be grafted in very small aliquots using multiple passes of the cannula and should not be molded after placement.
 While technically considered minimally invasive, significant bruising and tissue edema generally result from fat grafting.
While technically considered minimally invasive, significant bruising and tissue edema generally result from fat grafting.
 Continued research on the applications of adipose-derived stem cells is of utmost importance.
Continued research on the applications of adipose-derived stem cells is of utmost importance.
Introduction
Basic science/disease process
Since the 1890s when fat grafting first began, there has been controversy regarding the predictability and consistency of results that may be obtained with fat grafting. With some studies reporting up to a 70% rate of reabsorption, this is not surprising, especially with the dramatic variations in technique which have been used to transplant and study fat.15 Initially, a reasonable explanation for this was based on Lyndon Peer’s cell survival theory,16 whereby the number of viable adipocytes transplanted correlates with the volume of grafted fat that survives. Pu and colleagues have looked at a number of different laboratory assays that determine the viability of fat grafts, including viable adipocyte counts, colorimetric assays, adipocyte-specific enzyme assays, and routine histologic examinations.17,18 Their in vitro studies have looked at fat grafts obtained by direct excision, conventional liposuction, a fat graft harvest and transfer device, and the Coleman technique.19 The results favored the Coleman method, as it yields a greater number of viable adipocytes and maintains a more optimal level of cellular function.
The future
An exciting new potential of fat grafts is in reparative and regenerative medicine. Fatty tissue has been found to not only contain adipocytes, but also a subpopulation of cells consisting of adipose-derived stem cells (ADSCs), MSCs, endothelial cells and their progenitor cell lines, smooth muscle cells and smooth muscle progenitor cell lines, and numerous other stem cells that are multipotent and have the potential to aid in tissue regeneration.20 ADSCs serve a number of functions and may be induced to differentiate into many different cell types in culture, including ectodermal, mesodermal and endodermal lineages. Additionally, ADSCs have been shown to induce blood vessel formation, mitigate fibrosis and promote bone formation and wound healing. It is now believed that this particular population of cells within a fat graft may be a major contributor to the therapeutic potential of the graft.21
Rigotti et al. have used fat grafting in the irradiated breast and consistently showed an improvement or complete healing of the damaged tissues.22 As our understanding of fat and its constituent cells improves, so will our ability to positively affect other areas of medicine.
History
The first report of fat grafting was in 1893 by German surgeon Gustav Neuber1 when he transplanted adipose tissue harvested from the arm to correct a depressed facial scar that had resulted from osteomyelitis. This was followed 2 years later by Vincenz Czerny, who transferred a fist-sized lipoma from the buttock to the breast.2 Even then, fat grafting was considered difficult, time consuming to perform, and somewhat unpredictable; therefore new solutions were sought.
Looking for a solution to the problems caused by paraffin, Eugene Holländer proposed the use of fat injected through a cannula to correct deformities.3,4 He noted considerable reabsorption of the fat and therefore began mixing human fat with fat from a ram in an attempt to stabilize it. This resulted in a painful rash which lasted several days, however a good cosmetic result was obtained. Later, in 1919, Erich Lexer published a two-volume book dedicated to the technique of fat grafting.5 In this book, he presented a wide variety of conditions such as depressed scars, breast asymmetry, knee ankylosis, tendon adhesions, and micrognathia and the successful results after treatment with fat grafting. Charles Miller also described the injection of transplanted fat for the correction of facial folds and wrinkles in his 1926 publication, Cannula Implants and Review of Implantation Technics in Esthetic Surgery.6 Despite some favorable results from these pioneers, fat grafting was still unpredictable and it thus fell out of favor.
It wasn’t until the 1950s when Lyndon Peer studied the gross and microscopic appearance of transplanted fat that we began to understand and improve the predictability of fat grafting.7 He discovered that adipose grafts lose approximately 45% of their weight and volume at 1 year due to cell rupture and subsequent death. The fat cells that do not rupture, however, will survive and volume will be maintained. Improper handling of the fat prior to and during transplantation was also found to decrease the survival of the fat. Graft size also appeared to play a role in survival. A graft the size of a walnut was found to lose volume more rapidly than multiple smaller grafts of similar weight, likely due to the increased surface area of the smaller grafts. Revascularization, as seen microscopically, was noted by Peer to be essential for fat graft survival.
With the advent of liposuction in the 1980s by Fournier8 and Illouz,9 there was a renewed interest in fat grafting. Results, however, were only partially successful and the thought at the time was that perhaps better preparation of the fat was essential for its survival. Chajchir10 and Benzaquen took this advice and made some recommendations based on their own favorable results; yet there was still great confusion as to what really worked until the 1990s, when Coleman standardized the technique. This technique, called Lipostructure®, emphasizes gentle extraction of fat, centrifugation, and micro particle injections in multiple tissue planes. Dr Coleman has used this technique for more than 20 years and has documented the longevity and stability of fat grafting performed in this manner.11–14
Aging and atrophy
What is the process by which we age?23 Our concepts of how the face and body change with time are evolving, and the traditional ways of thinking about the problems and their solutions are being modified. We have been taught that over time, there is loss of elasticity of the tissues which results in descent and sagging of the skin. In the face, our traditional response to the descent has been to resuspend the tissues and to remove the excess skin. What we have ignored is the reason for the descent in the first place. While there are obvious environmental and genetic components to aging, one of the main reasons that the tissue starts to sag is lack of support, or lack of volume beneath it. One component of this volume is fat, but there are also components including collagen, elastin, hyaluronic acid, etc. that are involved. The goal then should be to replace the missing fullness, which will support and reposition the skin. In most cases, the body supplies us with a significant source of filling material to restore the volume lost with aging in the form of fat. There are, of course, limitations as to the ability of volume to support the overlying tissues. If there is a tremendous amount of sagging or excess skin, then manual resuspension and trimming may be necessary.
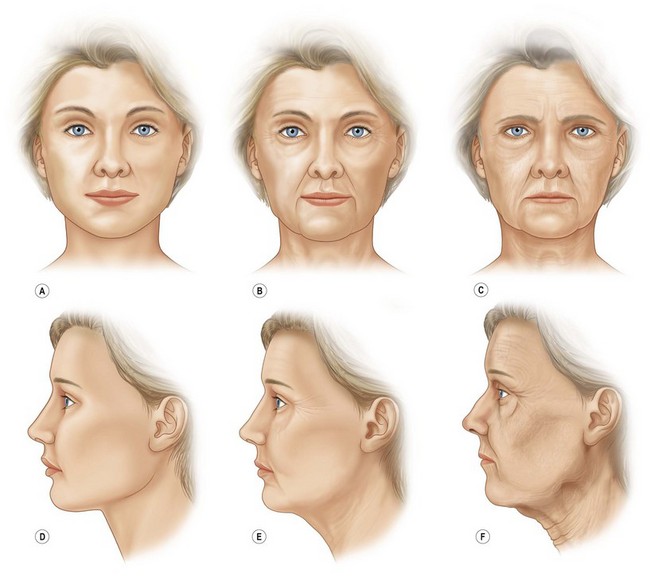
The easiest way to analyze a face to determine how it has changed is to study photographs of patients when they were younger compared to their current state. Depending on the degree of aging, one can often easily see that as the face ages, typical patterns emerge. The model shown in Figure 14.1 exemplifies the changes that occur, from left to right, going from age 20 to 50 to 70 years.
Diagnosis, patient presentation, indications
Patients may also present for facial fat grafting for corrective purposes. This includes patients with congenital deformities such as hemifacial microsomia and Treacher Collins syndrome. In addition, patients who have sustained previous trauma resulting in significant scarring or tissue loss can often benefit from fat grafting.24 Patients who have undergone previous facial cosmetic surgery often present with iatrogenic deformities such as hollow upper and/or lower eyelids and flattening of the posterior jaw line. These areas can be restored to a more youthful and natural appearance with fat grafting.
Facial atrophy from etiologies other than aging25,26 have been increasing over the last few decades, especially drug-related lipodystrophy seen in patients taking antiretroviral and protease inhibitor therapies. These patients often present with a maldistribution of not only facial fat but also body fat. While an excess of fat may appear as a dorsal hump on the upper back/lower neck, the face usually appears hollow in the temples and buccal cheeks, creating an appearance pathognomonic for the drug-related lipoatrophy. Fat can be removed from the dorsal hump by suctioning, but should probably not be used for grafting purposes, as it could have an unusual growth pattern.
What happens to the hands over time that will give away the age of the patient if the face does not? Again, there is a loss of volume, or soft tissue coverage over the veins and tendons of the dorsal hand. The hands of a 20-year-old are generally smooth and full, with the extensor tendons and dorsal veins barely visible. There is naturally little fat over the dorsum of the hands, but with thinning of the skin and loss of interosseous muscle fullness, the hands can take on a wasted appearance that can be reversed with fat grafting. Fat grafting not only restores a subtle fullness to the dorsal hand, but appears to thicken the skin as well, which partially obscures the tendons and veins so obvious in aging skin.27
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree