Chapter 34 Stratis ST Femoral Fixation System
Introduction
It has been estimated that approximately 200,000 anterior cruciate ligament (ACL) injuries occur annually, with approximately 100,000 patients per year undergoing reconstruction.1 Over the past decade, ACL reconstruction utilizing soft tissue grafts, such as hamstring autograft or tibialis anterior allograft, has gained increased popularity compared with bone–patellar tendon–bone (BPTB) autograft due to the decreased morbidity of hamstring harvesting, excellent clinical results, and availability of a variety of soft tissue allograft constructs. There remains continued controversy regarding graft options for ACL reconstructions. Of the graft choices available, the two most commonly used are autologous BPTB grafts and autologous hamstring tendon grafts. Even more perplexing is the number of fixation methods currently available.
For many surgeons, BPTB autograft remains the gold standard. Several long-term studies have demonstrated good outcomes with the use of this graft.2,3 Due to the morbidity associated with BPTB autograft, the use of hamstring tendon autograft has become increasingly popular. A number of prospective clinical trials comparing patellar tendon versus hamstring tendon have demonstrated comparable clinical results after 2-year follow-up.4–9 Additional studies, including a study by Feller and Webster,10 have demonstrated increased laxity based on KT-1000 in ACL reconstructions with hamstring tendon compared with patellar tendon. However, this difference was not clinically significant because patients in both groups demonstrated similar clinical scores and functional outcomes.
One of the primary advantages of using hamstring tendon in ACL reconstruction appears to be less donor site morbidity compared with patellar tendon. Namely, there is a lower incidence of anterior knee pain and a decreased risk of extension deficits, although some authors have found flexion deficits in patients with ACL reconstruction using hamstring tendon grafts.11,12 The weakness in extension or flexion following either patellar tendon or hamstring tendon harvest appears to be most pronounced early on, with differences diminishing between groups over time.13 Another concern regarding the use of hamstring tendon grafts is the phenomenon of tunnel widening associated with early forms of femoral fixation.14 With improvements in surgical technique and advances in femoral fixation devices, the differences in tunnel widening between hamstring and patellar tendon grafts have been reduced.15
The earliest forms of fixation for soft tissue grafts included post and washer and staple fixation. This required a significant lateral femoral dissection for the over-the-top or outside-in femoral guide, as well as placement of the devices used. Although the fixation strength was acceptable, the issues surrounding this technique included the surgical dissection and the rehabilitation consequences and the occurrence of painful hardware necessitating a second procedure for hardware removal and the so-called “bungee and windshield wiper effect.” Although biomechanical studies have shown that hamstring autografts have an ultimate yield strength greater than the native ACL and a stiffness curve more similar to the native ACL, the distally fixed construct placed these grafts at a disadvantage.16,17
The distal fixation also acts as a pivot point about which the graft moves during knee flexion and extension until the graft–femoral tunnel interface matures. This results in a cone-shaped tunnel widening at the articular femoral origin. Although the effect of tunnel widening on clinical outcome remains unclear, there is concern that this may affect healing of the graft–femoral tunnel interface and also create problems in the revision setting.18,19
To address these issues, different fixation devices have been devised and used. Suspensory anterior-lateral femoral cortical fixation devices have had great clinical success. They eliminate the need for a secondary lateral dissection and have good pullout strength.20 They do, however, suffer the consequences of elongation resulting from excessive length of the functional graft due to the distance of femoral cortical fixation. The use of interference screws has addressed the issue of aperture fixation at the femur. However, the concern regarding the damage the screw threads cause to the graft, as well as the less-than-optimal pullout strength, has limited their use. In addition, interference screws take up most of the space within the femoral tunnel, pushing the soft tissue graft to one side and limiting its contact with the femoral tunnel, which raises concerns of impaired graft tunnel healing.
Recently, transverse femoral tunnel pinning (transfemoral) fixation has been introduced and is gaining in popularity. These devices either spear the graft or drape the graft over a fixation pin in an anteroposterior orientation. The different designs have resulted in improved fixation and pullout strength.21,22 However, for each design there are concerns regarding graft damage and passage of the graft into the tunnel by pulling either axially or perpendicular to the tunnel, which often necessitates making a wider femoral tunnel to aid in graft passage.
Design Rationale of the Stratis ST
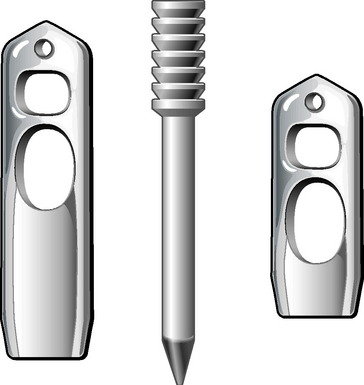
The Stratis ST femoral fixation system consists of a graft block and a ribbed transverse locking pin (Fig. 34-1). The graft block and pin are available in nonabsorbable polymer and absorbable poly-L-lactic-acid (PLLA).
1 Do Not Compromise Graft Integrity
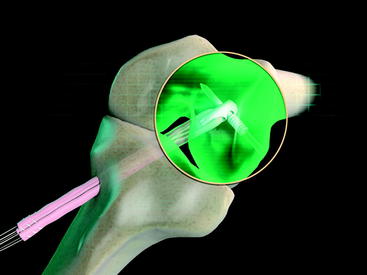
The Stratis ST femoral fixation system is designed for use with any soft tissue graft, with the quadrupled hamstring tendon being the most common autograft and tibialis anterior being the most common allograft used. The graft is passed through the distal graft portal and draped distally (Fig. 34-2). This hole is tapered smooth and contoured to deliver the graft to the distal biconcave compression fins. The transverse locking pin does not compromise or contact the soft tissue graft in any way. Instead, it locks the graft block within the femoral tunnel by docking with and traversing the more proximal locking portal. This ensures graft integrity and allows for a stiffer construct.
2 Have Excellent Pullout Strength
With the locking pin engaged in the graft block, it forms a “fixed T” construct that yields superior biomechanical characteristics. Pullout studies have shown an ultimate failure load of up to 1250N depending on which graft block is used. Cyclical loading studies of 50N to 250N showed no evidence of any creep, failure, or pin backout after 250,000 cycles.23 The locked fixed T construct also gives a theoretical decreased rotation moment because it is harder to rotate a fixed T construct through bone than it would be a simple transverse pin.
3 Have Aperture Fixation with Graft Tunnel Compression and Optimized Graft Tunnel Contact
The graft block is seated no less than 5 mm from the femoral tunnel origin. This placement allows the fin of the graft block to provide rigid fixation at the tunnel aperture. In addition, the 2-mm-thick fin provides graft compression to the tunnel wall with more than 90% graft tunnel interface23 (Fig. 34-3).
4 Be Pushed into the Femoral Tunnel
At the distal tip of the Stratis ST graft block is a docking station at which the insertion tool locks into place (Fig. 34-4). Once connected, the soft tissue graft–graft block construct can be delivered into the femoral tunnel. This locked construct allows the surgeon to better aim and guide the graft construct into the tunnel and then, once it is engaged with the tunnel, to push it into position with a mechanical advantage. This allows the surgeon to take full advantage of the compression fin and, if desired, oversize the graft but not the tunnel.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree