Abstract
Staged interpolation flaps require at least two stages to complete. They are usually reserved for defects that are deep, large (complete or subtotal subunit wound), or full thickness. These repairs achieve superior functional and aesthetic outcomes for the appropriate defect. All staged flaps contain robust muscle arterial perforators or named arteries within the pedicle. Their usage requires forethought on lining and cartilage support to preserve or augment contour. In facial reconstruction, the most useful staged flaps include the paramedian forehead flap, the Abbe’ (lip-switch) flap, and the cheek-to-nose interpolation flaps.
Keywords
flap, interpolation, staged, pedicle, cartilage, axial, full-thickness
Interpolation flaps demand exquisite planning and execution. In return, their sophistication offers rich rewards, with a highly vascularized covering that may resurface complex defects, provide tissue bulk, nourish free cartilage grafts (CG), and restore lining or contour as needed. The terms axial, indirect, interpolation, and staged flaps are synonymous, and all are variations of transposition repairs. All interpolation flaps have these shared features: (1) vascular pedicle based on a named artery and or its tributaries, (2) donor location distant and noncontiguous from the defect, and (3) two or more stages for completion (stage I for flap creation and closure, stage II for pedicle division, and often additional stages for revisions).
The success of these flaps is dependent on adhering to three key principles. First, all margins must be definitively cancer free. Second, these flaps should be considered as heavy surface coverings (skin, subcutis, muscle), and a stable infrastructure must exist to support them. A large nasal defect, for example, cannot simply be covered without stable cartilage support and mucosal lining. Third, optimal repairs often require the reconstruction of an entire subunit. Wounds that consume 50% or more of a subunit are best restored in total, with few exceptions. Patients with staged flaps require a complete preoperative consultation. Multiple visits and revisions, temporary physical deformities, and intensive wound care, as well as substantial activity and work restrictions, are the rule in staged repairs. In exchange for this demanding regimen, however, are surgical results that have no parallel. This chapter will discuss techniques for (1) paramedian forehead flap (PFF), (2) cheek-to-nose interpolation flap (CNIF), and (3) Abbé or lip-switch flap as applied to skin cancer reconstruction.
Paramedian Forehead Flap, Stage I
Indication
The PFF is a workhorse in facial reconstruction. Although it may close any wound on the central face, its best application is to the distal nose (tip, ala, and columella), where tissue thickness and sebaceous quality are closely matched by forehead skin. The PFF is ideal for recreating the convexity and projection of the nasal tip. Subtotal nasal tip and/or alar defects may be candidates for the PFF. Proximal wounds on the nasal dorsum, sidewall, nasal root, and medial canthus have inherently thinner skin and may be incongruous for the much thicker PFF, unless a substantially deep defect is present.
Anatomy
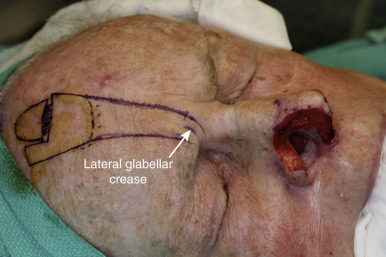
The primary and secondary vascular supply to the PFF is the supratrochlear (internal carotid system) and dorsal nasal artery (external carotid system), respectively. The supratrochlear artery (SA) is reliably located at the medial border of the eyebrow, on average 10.9 mm from the facial midline. At the medial eyebrow, a glabellar crease (if present) delineates where the SA crosses the superior orbital rim to enter the forehead ( Fig. 8.1 ). Below the orbital rim, the SA lies deep to the periorbital muscles (orbicularis oculi and frontalis) just above the periosteum. Above the rim, however, the SA pierces the corrugator supercilii muscle at 15–25 mm above the supraorbital rim and ascends superficially into the forehead, sandwiched between the frontalis muscle below and the subcutis above. Consequently, to preserve the SA near the orbital rim, dissection must be below the frontalis muscle and deep fascia. Transection of the SA during surgery is not always disastrous. The robust arterial perforators are often sufficient to nourish the flap. Indeed, histologic studies suggest that the PFF is sometimes a random pattern flap, with no discernible high caliber artery within the pedicle.
Flap Design
The ideal PFF is an aesthetic covering that restores normal contour and symmetry without creating a shapeless blob. Table 8.1 discusses the critical design issues in a PFF. The covering provided by a PFF requires a stable nasal infrastructure (cartilage support and mucosal lining). Structural cartilage grafts (SCGs) to prevent nasal valve collapse and alar rim contraction are usual considerations in PFF repairs. More neglected, however, are SCGs that restore contour to the nasal supratip. Contour grafts should be considered in patients that have thick nasal tip skin and supratip defects ( Fig. 8.2 ). Without a contour graft in these patients, a PFF alone may be insufficient to restore normal tip projection.
| Defect Considerations | Comments |
|---|---|
| Does this defect require lining support? | Replacing lining may require intranasal mucosal flaps prior to PFF execution. |
| Does this defect need cartilage support? | Cartilage grafts may be replacement or structural in nature. Replacement grafts restore missing cartilage or bone. Structural grafts add to stability and contour and prevent tissue contraction to an intact cartilage infrastructure. |
| Is the PFF sufficient to close this wound? | PFF may be combined with regional flaps, free cartilage grafts, and split- or full-thickness skin grafts for defects that extend onto multiple subunits. |
| Does the residual subunit need to be excised? | Cosmesis is often superior when entire subunits are resurfaced. |
| Flap Considerations | Comments |
| Has there been previous surgery at the proposed pedicle site? | Normal vascular anatomy may no longer be reliable and Doppler identification of a viable artery may be needed. |
| Does the flap template accurately account for the 3-dimensional contour of the nose and infratip? | A flexible template material (suture foil wrap, soft foam, Duoderm) is essential for accurately molding the template design. Two-dimensional defect measurements are inadequate. |
| Does the forehead’s vertical height (from orbital rim to anterior frontal hairline) provide adequate length to reach the defect? | A short forehead height may require modifications to the template design and/or pedicle to optimize flap extension. |

Measurements of the defect must be accurate—neither oversized nor undersized for the wound. The PFF template should be measured after the residual subunit has been outlined, but prior to the excision of any remaining skin ( Fig. 8.3 ). This avoids an artificially enlarged dimension from a retracted wound edge. A template should also reflect the three-dimensional nature of the nose, especially if a defect extends to the infratip, columella, and ala ( Fig. 8.4 ). If the vestibular mucosa is missing, the PFF may be extended and turned down to provide nasal lining. The thin soft nasal triangle is difficult to rebuild. Either second intention healing or a finely thinned PFF are options for this thin, concave area. Whenever possible, the unaffected contralateral side should be used as a template to restore symmetry. A right-sided nasal tip and ala wound, for example, should be repaired based on the normal left tip and ala.


The vertical height of the forehead (from orbital rim to anterior frontal hairline) will determine the potential reach of this flap. If the vertical length is inadequate (short forehead height relative to distal defect), then the modifications listed in Table 8.2 will significantly extend a flap’s distal reach.
| Forehead Flap Design Modifications | Comment |
|---|---|
| Vertical extension of flap into the anterior frontal scalp | Potential transfer of terminal hairs onto the nasal defect. |
| Potential disruption of frontal hairline and scarring alopecia if donor site closure is not complete. | |
| Extension of flap lateral to midline | Potential compromise of vascular supply to lateral flap extension. |
| Potential donor site morbidity with eyebrow elevation (scar contraction with second intention or distortion with complete closure). | |
| Tangential flap design that crosses the midline | Flap becomes random pattern. |
| Pedicle Modifications | Comment |
| Keeping width of pedicle at its base between 1.0 and 1.5 cm | Wider pedicles (>1.5 cm) limit flap mobility. |
| Wider pedicles increase vascular strangulation during flap rotation toward the distal defect. | |
| Mobilizing base of pedicle below superior orbital rim | Incorrect elevation and undermining may lead to periorbital trauma and compromise vascular pedicle (supratrochlear artery). |
| Limit incisions to the epidermis and dermis. Supraperiosteal undermining should be performed bluntly with a finger or cotton-tipped applicator. Alternatively, subperiosteal undermining of entire medial brow complex off of the superior orbital rim and arcus marginalis may be performed using a subperiosteal elevator. | |
| May extend flap reach by at least 2 cm. | |
| Pedicle division at stage II will require eyebrow repositioning for bilateral symmetry. | |
| Relaxing incision at medial base of pedicle (toward glabella and nasal root) | Releases dermal attachments at the pedicle base that may enhance flap mobility. |
| Incision must not extend past superficial dermis. | |
| Superficial horizontal incisions in the undersurface of the pedicle | Allows for stretching of the pedicle. |
| Incision must not extend into subcutaneous fat due to risk of transecting the supratrochlear artery. | |
| Defect Modifications | Comment |
| Temporary alar suspension stitch | Suture is passed through the alar cartilages (if present) onto the glabella above. This suspends the nasal tip superiorly to meet the forehead flap, effectively extending flap reach. Suture is then removed at time of pedicle division. |
| Prominent suture reaction at the glabella is predictable. | |
| Potential for weakening the alar cartilage integrity with excessive superior suspension. |
Design considerations for the pedicle include its position and width. Identifying the SA pedicle may be done clinically, by using the anatomic landmarks mentioned earlier, or definitively by confirming with a manual Doppler (8–10 MHz frequency). However, 8% of supratrochlear arteries cannot by detected by Doppler. Alternatively, PFF may be designed as a random flap based on the complex vascular plexus of the corrugator complex and frontalis. The pedicle width therefore rarely needs to be greater than 1.5 cm. Wider pedicles, in fact, are counterproductive and restrict flap mobility as well as vascular integrity (by increasing torque and compression on the artery during flap rotation). This author routinely develops a pedicle base of 1–1.5 cm. The glabellar frown line may be used as an anatomic landmark, with flap borders placed 8–9 mm lateral and 2–3 mm medial. Another option is to base the template on a vertical line directly above the medial canthus, since the supratrochlear vascular pedicle has been shown to lie no more than 3 mm lateral or medial to the medial canthus. The lateral pedicle incision stops at the eyebrow, whereas the medial incision should extend longer, often into the nasal root, to incorporate branches from the dorsal nasal artery (see Fig. 8.1 ). Traditionally the pedicle position is on the opposite side of where the defect is located. A left nasal tip defect, for example, would have been closed by a PFF based on the right SA. This concept applied when pedicles were much wider, to minimize twisting and tension. With more narrow pedicles (1.5 cm), there is less twisting during movement, and PFFs may be ipsilateral to the defect. Same side flaps are shorter in length than contralateral designs and conserve significant tissue.
Anesthesia
The PFF may be safely performed as an outpatient procedure under local anesthesia (LA). LA should be injected in stages. If a patient needs a CG and a PFF, then consider anesthetizing the ear and forehead first. Begin anesthetizing the nose when the forehead flap is incised. By administering LA in a stepwise fashion, the patient will be kept comfortable. Tumescent anesthesia (TA) is useful by rapidly anesthetizing large areas with minimal patient discomfort. With TA, however, waiting (at least 20 minutes) for the swelling to subside is advisable, as there is a pseudotension in tissue movement when it is edematous. LA may be supplemented by nerve blocks, oral benzodiazepines (lorazepam, midazolam), and oral analgesics. Rarely, conscious sedation may be needed and can be safely performed by dermasurgeons. Appropriate credentialing for advanced cardiac life support and sedation are essential for the latter modalities.
Execution
Prior to the first incision, all design elements should be measured and remeasured, and anesthesia must be complete. The execution sequence for this author is (1) cartilage support and nasal lining restoration (if needed), (2) flap harvesting and pedicle mobilization, (3) defect preparation, (4) flap preparation and inset, (5) donor site closure, and (6) postoperative care.
Suturing intranasally can be difficult both ergonomically and visually and is facilitated by Loupe magnification, a headlamp, Castroviejo needle drivers, Castroviejo delicate tissue forceps, or bayonet forceps.
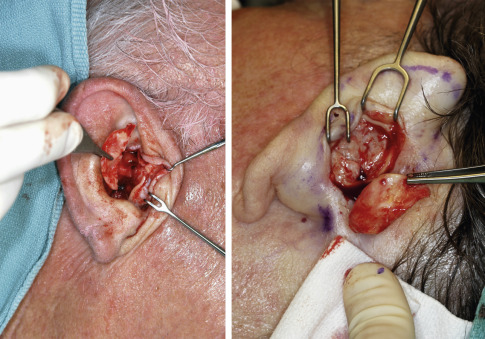
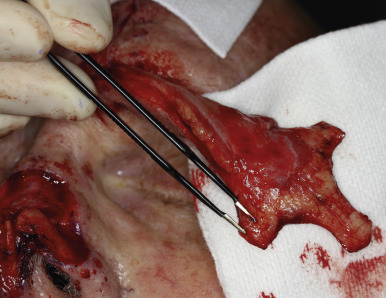
Cartilage and Lining Restoration
CG and nasal lining are essential ingredients for a stable nasal architecture. CG are either structural (native cartilage present but additional CG needed for support; Fig. 8.5 ) or restorative (replacing missing cartilage). SCG serve to (1) support heavy flap tissue, (2) maintain airway patency of the internal nasal valve (priority in nasal reconstruction), (3) minimize scar contraction, and (4) restore contour projection (nasal tip). CG may be auricular (antihelix or concha; Fig. 8.6 ), nasal (septum), or costal in nature. Auricular cartilage harvest is easiest and may be performed from an anterior or posterior approach. Anterior incisions are more accessible, but scars are more visible than posterior incisions. Postauricular access often yields a larger cartilage piece than an anterior approach. The antihelix yields cartilage that is long but thin, ideal for alar support. The concha offers thick, curved, and large grafts that may be sculpted and divided into multiple grafts, ideal for the PFF. The subject of nasal lining is beyond the scope of this chapter. General options, however, for smaller mucosal defects (<1 cm) include (1) turnover hinge flap, (2) turndown of a forehead flap extension, (3) full-thickness skin graft (FTSG), and (4) bipedicle vestibular skin advancement flap. Larger lining restoration may require (1) turnover forehead flap, (2) septal mucoperichondrial hinge flap, (3) composite septal chondromucosal pivotal flap, or (4) larger FTSG vascularized by an overlying PFF.

Flap Harvesting and Pedicle Mobilization
The PFF may be mobilized at its superior edge to include just the skin and subcutis or down to underlying galea. The former approach facilitates flap debulking during inset but results in greater bleeding. A subcutaneous level is preferred if the flap is in the hair-bearing scalp, to expose terminal hair bulbs for depilation. The level of undermining, however, delves deeper into the subgaleal plane as one approaches the eyebrow to preserve the SA. The transition from subcutis to subgalea should occur at least 3 cm above the orbital rim. Undermining past the orbital rim should be under direct visualization, as the SA is at risk of transection. Occasionally, subperiosteal release of the arcus marginalis and brow complex is required to enhance flap extension (see Table 8.2 ). The PFF should now overlie the defect without tension ( Fig. 8.7 ).

Defect Preparation
With the flap reach and pedicle secured, the flap dimension is again compared with the defect plus any planned subunit enlargement. Only when adequate cover is ensured should the remaining subunit tissue be removed. Undermining is needed peripheral to the defect, and wound borders need to be trimmed. Beveled edges should be revised to be perpendicular except for the infratip, where a beveled edge is desirable to more smoothly approximate with the flap. The PFF’s edge should correspondingly be reverse-beveled to fit the distal wound.
Flap Preparation and Inset
Prior to any suturing, the flap thickness must be revised to fit the defect. Aggressive debulking except for a thin subdermal layer is possible because of the excellent vascularity of the SA ( Fig. 8.8 ). Constant reference to the defect is mandatory to prevent excessive thinning. Flap inset begins with interrupted epidermal sutures to secure its leading edge with the defect. If dermal-buried sutures are placed, this author prefers Poliglecaprone 25 (Monocryl, Ethicon) because of its minimal tissue reaction, a desirable feature on the sebaceous nasal tip. Dermal sutures contribute to flap security and minimize incision line separation. The proximal flap as it abuts the nasal dorsum is not sutured until pedicle division.
Donor Site Closure
Donor areas are approximated as much as possible, and any remaining wound heals by second intention ( Fig. 8.9 ). Patients may be reassured that this open portion will be significantly smaller because of inevitable wound contraction ( Fig. 8.10 ). Tissue expansion and complex scalp flaps should be avoided, as they often lead to excessive morbidity on both donor and recipient tissue without cosmetic benefits. At most, unilateral or bilateral W-plasties along the frontal hairline may be considered for complete closure of the forehead wound, but excessive tension should be avoided. Forehead tension (forced donor site closure) often leads to severe headache and nausea postoperatively.


Postoperative Care
Postoperative bleeding at the sides of the exposed pedicle is common and may be prevented with meticulous electrocoagulation. Bovine collagen matrix (BCM) may be sutured with 5-0 fast absorbing plain gut onto the exposed pedicle, followed by petrolatum gauze application. BCM is also applied to any remaining secondary defect at the forehead to aid second intention healing. BCM seals the exposed tissue, facilitates hemostasis, and is incorporated into the pedicle as an epithelial covering. Alternatively, the exposed pedicle may be wrapped with Surgicel or Surgicel Nu-Knit. This oxidized cellulose gauze promotes hemostasis and its removal causes less discomfort than Vaseline gauze. Visual fields are blocked with pressure dressings, and the wearing of glasses is usually not possible without preoperatively customized devices. An optometrist may adjust the frame to temporarily fit over the dressing.
Postoperative observation for several hours is advisable, especially for patients at risk of bleeding. Hospitalization is not necessary, although patients must stay locally in the charge of a caretaker. Postoperative prescriptions include antibiotics (optional), analgesics, and antiemetics as needed. Wound care for the PFF may be intimidating and patients often express fear of detaching the pedicle. Detailed guidance with the first dressing change and the availability of a wound-dressing video will preempt much anxiety. A telephone call from the surgeon in the immediate perioperative period can also provide reassurance.
Paramedian Forehead Flap, Stage II
The second stage usually occurs approximately 3 weeks later and detaches the pedicle. Intermediate procedures may be needed (flap debulking and thinning) and should occur prior to the pedicle division. Stage II may be delayed for 4–6 weeks in patients at risk of flap compromise (heavy smokers), whereas earlier pedicle division (<3 weeks) may be safe but should not be performed routinely. In fact, the 6 weeks after stage I is a prime vascular period when revisions may be performed with impunity.
The approach to the pedicle stump after division varies. It may be closed primarily with a V–Y inset. A V–Y inset may be considered in patients who have a narrow glabellar width, or closely spaced eyebrows. The flap inset preserves the glabellar diameter and is camouflaged by existing rhytids ( Fig. 8.11 ). Eyebrow repositioning is essential in all cases and may require a curvilinear ellipse for brow plasty.