Soft Tissue Reconstruction of the Upper Extremity
Scott L. Hansen
Patrick Lang
Hani Sbitany
INTRODUCTION
Soft tissue reconstruction of the upper extremity requires strict adherence to standard surgical principles. In keeping with the reconstructive ladder, options for coverage include primary closure, skin grafting, local flaps, regional flaps, and free tissue transfer. Goals include restoration of a functional, sensate, and aesthetically acceptable hand. In addition, stable coverage of vessels, nerves, tendons, and joints throughout the forearm and arm is required. Primary wound healing is also a fundamental goal as it reduces scar formation and joint stiffness. Among the considerations involved in selecting the proper techniques are the components involved, the size of the defect, the mechanism of injury, and the cleanliness of the wound. Patient factors including handedness, occupation, age, sex, and overall health are also considered.
Classic teaching dictates that soft tissue reconstruction follows skeletal stabilization in the traumatized extremity. After bony fixation, stable soft coverage facilitates wound healing, reduces contracture, decreases infection, and improves outcomes for secondary skeletal operations such as bone grafting or distraction. The attempt to achieve a stable soft tissue envelope begins immediately following injury, as Godina espoused for lower extremity injuries.1 Although definitive soft tissue coverage may not be immediately possible, wound debridement is always performed initially. Early debridement of nonviable tissue reduces the opportunity for local inflammatory response and infection. Serial debridement is performed as many times as necessary to ensure viability of all remaining tissues. Definitive coverage is then performed once the wound is adequately debrided.
When planning definitive coverage, local tissue options are considered. Uninvolved soft tissue of the upper extremity is often superior to more distant tissue, as it offers similar sensibility and tissue match. Unfortunately, there is often a paucity of donor tissue in the upper extremity, especially following significant injuries or extirpative surgery. In such cases, distant tissue options are explored.
Basic wound care principles are as essential as the various grafts and flaps available. These principles allow the crafting of a safe and effective reconstructive plan for the upper extremity. This chapter outlines reconstructive options ranging from simple skin grafts to complex free tissue transfer. There are many instances in upper extremity soft tissue reconstruction where “less is more”—an example being the healing of a fingertip injury by secondary intention, when more complex solutions would prolong impairment. The surgeon must be comfortable with all rungs of the reconstructive ladder if the appropriate reconstruction is to be performed in a wide range of clinical scenarios.
NEGATIVE PRESSURE DRESSING
The use of negative pressure dressings has revolutionized the care of complex wounds. Although some controversy exists regarding its effect on time to heal, there is no debate over the degree of convenience that it has introduced for both the patient and the surgeon. Wounds of the upper extremity requiring serial debridement do well with negative pressure dressings between procedures provided no neurovascular structures are exposed. Thus, negative pressure dressings serve as a bridge to definitive coverage. In addition to the convenience and cleanliness of the dressings, negative pressure has been shown to promote wound contraction, improve local tissue perfusion, and promote the formation of granulation tissue—effects that make definitive reconstruction easier to achieve.2
HEALING BY SECONDARY INTENTION
The goal of upper extremity soft tissue reconstruction is primary wound healing. Healing by secondary intention is occasionally appropriate such as in certain fingertip injuries. As one of the main goals of fingertip reconstruction is the restoration of protective sensibility, this method is helpful in small, superficial tip defects. In such defects, sensation is maintained in the healed tissue as sensate skin is drawn into the defect.3
This is especially helpful for defects in both children and the elderly. Wounds heal more rapidly in children than in adults because of enhanced wound contraction. In the elderly, healing by secondary intention avoids some of the pitfalls of sensate local flaps: prolonged postoperative immobility and resultant joint stiffness, and the avoidance of necessary cortical reinnervation.
Apart from these defects, healing by secondary intention is of little use for soft tissue resurfacing elsewhere in the upper extremity because of the functional limitations from the resultant contracture.
AMPUTATION
Similar to healing by secondary intention, revision amputation is best suited for specific cases of fingertip injuries in select patients. This is often advantageous in those patients eager to return to work, and those with multiple comorbidities or clinically unstable pictures.
Although those injuries of the remainder of the extremity with large amounts of devitalized tissue may also benefit from some degree of select amputation, it is rarely indicated as the primary method for definitive treatment of upper extremity injuries.
SKIN GRAFTS
Stable skin and soft tissue coverage of the hand is essential for hand function. Volar and dorsal surfaces should be considered separate entities when considering coverage. The dorsal hand skin is thin, mobile, and has the primary function of allowing flexion, while maintaining nonadherent coverage of tendons and joints. Split-thickness skin grafts are appropriate for large defects of the upper extremity that have no vital structures exposed. In addition to improved “take” relative to full-thickness skin grafts, split grafts also offer the advantage of greater secondary contraction of the wound, and resultant reduction in the size of the grafted area. The presence of paratenon greatly enhances the survival of the graft and improves postoperative tendon gliding. The ideal thickness for skin grafts to the hand ranges between 0.012 and 0.014 inches. Meshing of the graft can be performed to increase graft surface area, and allow egress of underlying fluid.
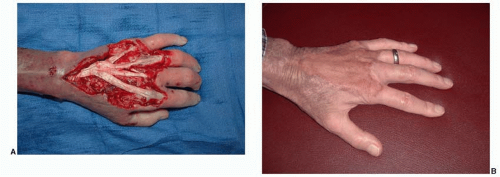 FIGURE 73.1. A. Exposed extensor tendons after IV infiltration and serial debridements. B. Reconstruction with Integra followed by delayed coverage with a skin graft. |
When resurfacing the dorsal surface of the hand, tendon adhesion to the overlying skin graft may occur, and subsequent tenolysis is often required. The authors have found that large dorsal defects with exposed tendon do well with coverage by Integra Dermal Regeneration Template, followed by split-thickness skin grafting (Figure 73.1). Other biologic templates may also be comparable and should provide the benefits of improved coverage and reduced adherence to underlying gliding tendons. Though not appropriate for all wounds, elderly patients or those with significant comorbidities precluding free tissue transfer can be reconstructed using this method.
The glabrous skin on the volar surface of the hand carries a highly specialized tactile sensory function. Because of the mechanical demand placed on the working palm, the volar skin is thick and densely adherent to the underlying fascial system, through a series of vertical ligaments. For defects involving the volar hand, primary options for resurfacing include full-thickness glabrous skin grafts from either the hypothenar eminence or the non-weight-bearing region of the plantar foot. This offers the advantage of also providing specialized nerve endings, similar to those encapsulated nerve endings in the injured volar skin, and donor sites that may be closed primarily. If necessary, full-thickness grafts for such defects may also be obtained from other areas of the upper extremity. Given that the native volar skin is devoid of pilosebaceous structures, every effort should be taken to harvest the grafts from similarly hairless areas, such as the volar wrist, or the skin just proximal to the medial epicondyle of the elbow.
Skin grafting of forearm and proximal arm defects follows a similar algorithm to dorsal hand grafting. The majority of defects can be adequately covered with meshed split-thickness grafts. Skin grafting is also an option for fingertip defects. While full-thickness skin grafts are sometimes useful for tip coverage, they are rarely a preferred primary method due to poor recovery of sensibility. In most cases, a sensate flap is a better option, as it retains the important protective sensibility of the fingertip.
LOCAL FLAPS
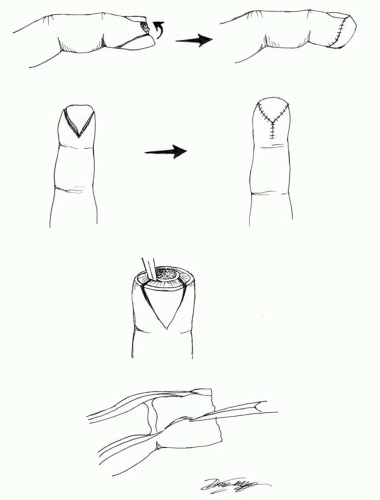
Bilateral V-Y Advancement Flap
Transverse and volar fingertip injuries can be treated with bilateral V-Y advancement flaps (Figure 73.2). As described by Kutler, these flaps are elevated from the sides of the injured digit and advanced distally.4 Because mobility is limited, division of the vertical fibrous septa is crucial to obtain adequate advancement. The terminal branches of the neurovascular bundles lie in the lateral pulp tissue of the flap, and thus, careful attention must be taken to avoid their injury during undermining. In cases where complete closure cannot be achieved due to inadequacy of advancement, the flaps can be advanced maximally, and the remaining wound can be allowed to heal by secondary intention. Due to the limited mobility of these flaps, use of the V-Y advancement flaps is usually reserved for defects distal to the midnail level.
Volar V-Y Advancement Flap
Closure of transverse or dorsally angulated fingertip injuries can often be achieved with the use of a volar V-Y advancement flap (Figure 73.3). Described by Atasoy and Kleinert, this is a V-shaped flap with the tip at the distal interphalangeal crease which is advanced distally, to achieve tension-free closure.5 Like the bilateral V-Y advancement flaps, the volar advancement flap requires division of the fibrous septa from the distal phalanx to achieve adequate advancement. Expected advancement, when incision is entirely distal to the DIP flexion crease, is 1 cm. When properly planned, the entire donor defect can be closed primarily with little tension.
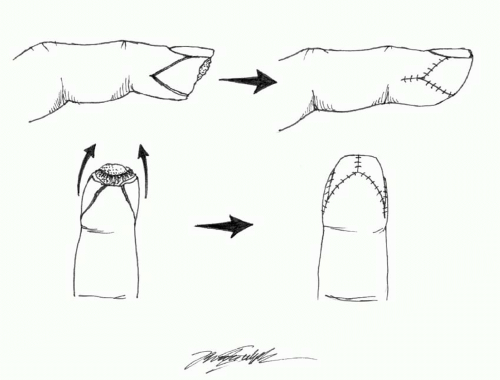 FIGURE 73.2. Kutler flap. Bilateral triangular advancement flap for patients with transverse or volar oblique amputations. |
Volar Neurovascular Advancement Flap (Moberg Flap)
Fingertip amputations can be covered with distal advancement of the entire volar finger skin as a single neurovascular flap (Figure 73.4). The volar digital neurovascular advancement flap has been described for use in all digits, but Moberg popularized its use for transverse amputations of the thumb, a procedure that persists today as the most common application of this flap.6 Two parallel longitudinal incisions are made dorsal to the neurovascular bundles, followed by elevation of the flap off of the flexor tendon sheath. The flap is designed with its base at the metacarpal phalangeal crease and advanced distally with its neurovascular bundles intact. The true Moberg flap requires splinting with some degree of flexion to allow for tension-free healing of the advanced flap. This can create problems with stiffness, particularly in older patients. Modifications include the creation of a true island flap with skin grafting of the resulting proximal defect, which may increase advancement to 1.5 cm. Alternatively, flap design into the web space proximally may increase advancement to 3.0 cm.7
This flap should be avoided in non-thumb digits due to tenuous dorsal skin perfusion following the required longitudinal incisions. It is the unique dorsal and volar blood supply of the thumb that allows for safe elevation of this flap.
Cross Finger Flap
Volar fingertip pulp amputations can be treated with the cross finger flap. Gurdin and Pangman first described the use of dorsal skin and subcutaneous tissue from an adjacent finger for volar defect coverage.8 The flap is designed over the dorsum of the middle phalanx and elevated off the underlying extensor paratenon. Preservation of the paratenon over the extensor apparatus is critical. The flap is then turned over to resurface the volar tip of the adjacent (injured) finger (Figure 73.5). The pedicle can be designed laterally, proximally, or distally. The donor site is skin grafted (full-thickness graft) and both digits are immobilized. Because this flap acts as a vascularized full-thickness flap of skin, it may be safely divided within 2 weeks; thus, stiffness of the immobilized digits is minimized.
 FIGURE 73.4. A. Moberg flap. Design of the homodigital advancement flap to cover defects of the thumb pulp. B. Advancement of Moberg flap to cover thumb pulp defect. |
Complications associated with the cross finger flap include poor aesthetics at the donor site, stiffness due to prolonged immobilization, and cold intolerance of the donor digit. In addition, the recipient digit will always have relatively poor sensibility.
Reverse Cross Finger Flap
Dorsal digital wounds can be covered with use of the reverse cross finger flap (Figure 73.6). This flap consists of subcutaneous tissue elevated from the dorsum of the middle phalanx of the adjacent finger. This is exposed by first elevating the skin of the donor digit in this region, maintaining a base laterally, on the side opposite the injured digit. The flap is turned over to cover the dorsal defect of the injured finger. The elevated skin from the donor digit is then sutured back into its native position and the flap on the injured digit is skin grafted. Delayed division of the pedicle is generally performed at 2 weeks.
Thenar Flap
The thenar flap is an excellent and reliable choice for reconstruction of distal phalanx soft tissue defects and amputations (Figure 73.7). This flap stands in contrast to the historically complication-ridden palmar flap, described by Gatewood, which resulted in frequent proximal interphalangeal (PIP) joint contracture.9 Beasley established four guidelines for proper execution of the thenar flap in an attempt to limit complications associated with the related palmar flap: (1) the metacarpal phalangeal joint of the recipient finger is fully flexed in an attempt to limit required flexion of the PIP joint; (2) the thumb is placed in full palmar abduction or opposition; (3) the flap is designed with a proximal pedicle high on the thenar eminence so that its lateral margin is at the metacarpophalangeal skin crease; and (4) the pedicle is divided after 10 to 14 days.10
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree