Introduction
The scalp is the soft tissue covering the calvaria. It anatomically positioned in the cranial side of the line connecting the supraorbital border of the forehead, the frontal process of the zygomatic bone, the superior margin of the zygomatic arch, the external acoustic foramen, the mastoid process of the temporal bone, and the superior nuchal line of the occipital bone.1 The major difference between the scalp and other skin in terms of appearance is that it has hair in almost all areas, excluding the forehead. In a cross-section, the scalp reveals a layered structure, usually divided into five layers, excluding the temporal region, as follows, from the outermost layer down: skin, subcutaneous fat (dense connective tissue), galea aponeurotica (aponeurotic layer), loose connective tissue; and pericranium (Fig. 4.1). Among these layers, the skin, subcutaneous tissue, and galea aponeurotica layer are closely connected, making it difficult to bluntly separate each layer. Therefore, these layers from the skin to galea aponeurotica are lumped together and also called the superficial fascial layer, whereas loose connective tissue is also called the deep fascial layer.2
Scalp (Skin) and Subcutaneous Fat Layer
The structure of the scalp is fundamentally similar to the skin in other regions; however, the dermis is thick compared with that in other parts of the body and is rich in blood vessels. Furthermore, it has an abundance of hair.
Subcutaneous tissue comprises an abundance of hair follicles and sweat glands. Moreover, there are many fibrous septa, similar to that of the palms of the hands and soles of the feet, closely connecting the skin and the galea aponeurotica layer. Therefore, subcutaneous fat is separated into small fat lobes by these fibrous septa. In this layer are many perforating arteries and veins heading to the skin from the main vascular network of the scalp inside the galea aponeurotica, along with the small sensory nerves transmitting cutaneous sensation.
Galea Aponeurotica
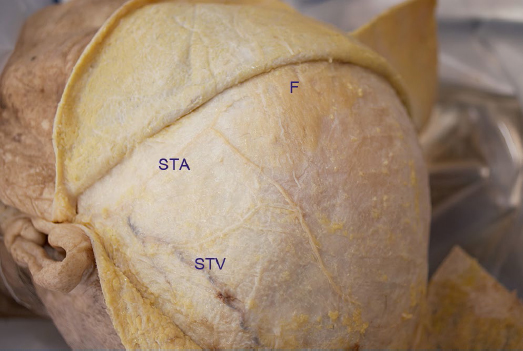
The galea aponeurotica is the intermediate aponeurosis of the occipitofrontalis muscle and is connected to the frontalis muscle at the front as well as to the occipitalis muscle at the rear (Fig. 4.2). The frontalis muscle originates from the galea aponeurotica and attaches to the dermis of the eyebrow after intersecting with the orbicularis oculi muscle and procerus muscle near the supraorbital border. Generally, frontalis muscles run obliquely downward superolaterally to inferomedially; therefore, there is a V-shaped area in the center of the forehead between the bilateral frontails muscles and the galea aponeurotica that extends to the front in this V-shaped part of the forehead. The occipitalis muscle originates from the highest nuchal line of the occipital bone, runs upward, and attaches to the galea aponeurotica. These frontalis and occipitalis muscles are both innervated by the facial nerve; the temporal branch innervates the frontalis muscle, and the occipitalis muscle is innervated by the posterior auricular nerve. It is the role of the frontalis muscle to lift the eyebrows, thereby forming horizontal wrinkles on the forehead. The occipitalis muscle has a role of pulling the galea aponeurotica and placing tension on the scalp; however, it is degenerative and weak, only having the effect of supporting the frontalis muscle. In the temporal region, the galea aponeurotica transitions to the superficial temporal fascia, which is a part of the superficial musculoaponeurotic system (SMAS).3,4 The superficial temporal fascia contains the temporoparietal muscle and superior auricular muscle in the same plane. Major blood vessels of the scalp run in the galea aponeurotica layer and give off multiple branches toward the skin and subcutaneous fat layer. Therefore, massive bleeding is commonly observed when separating the galea aponeurotica and subcutaneous fat layer.
Loose Connective Tissue
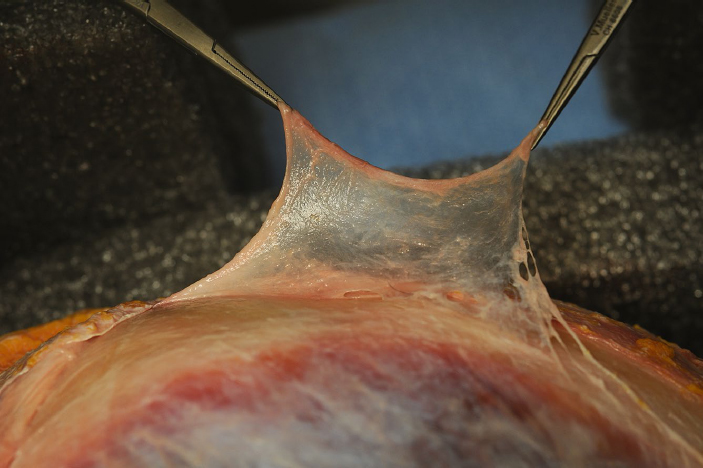
This layer is also known as the subgaleal fascia and subaponeurotic plane (Fig. 4.3). It is found between the galea aponeurotica or pericranium, providing mobility to the scalp. It is approximately 1 to 3 mm thick and is grossly observed as a semitransparent, foamy layer. Chayen et al reported that this loose connective tissue layer is a three-layer structure comprising two loose areolar tissue layers and a dense fascial layer between two loose areolar tissue layers, an outer layer (loose areolar tissue), a dense fascial layer, and a deep layer (loose areolar tissue).5 Although blood vessels are not grossly observed in this layer, it is macroscopically observed as layers having blood vessels. The blood circulation of this layer is supplied via two strains wherein the first is the perpendicular blood flow from the vascular plexus inside the galea aponeurotica layer using perforating vessels; the second is the blood flow by the blood vessel system directly flowing in from the main blood vessel of the scalp to the loose connective tissue layer, such as a superficial temporal artery, supraorbital artery, and supratrochlear artery. Using these blood circulations, it is used as a flap when very thin soft tissue flaps are required during auricular reconstruction and such procedures.6
Fig. 4.2 Galea aponeurotica (cadaver dissection picture of the left superior view.) Left frontalis muscle, galea aponeurotica, and superficial temporal fascia are exposed. F, frontalis muscle; STA, superficial temporal artery; STV, superficial temporal vein.
Pericranium
This soft tissue layer is positioned in the deepest subcutaneous tissue. The pericranium of the head is continuous with the temporal fascia in the temporal region and is not observed underneath the temporalis muscle of the temporal fossa.
Blood Circulation Morphology of the Scalp
Regarding the arterial blood supply to the scalp, the supraorbital artery and supratrochlear artery, branching from the ophthalmic artery, supply blood flow to the anterior scalp; the superficial temporal artery, posterior auricular artery, and occipital artery, branching from the external carotid artery, supply blood flow to the lateral and posterior sides of the scalp, respectively (Table 4.1). These arteries are connected to each other in the parietal region, forming a dense vascular network. These blood vessels form the vascular plexus in the galea aponeurotica layer, thereby branching blood vessels vertically toward the super ficial layer (that is, the subcutaneous fat layer) or deep layer (loose connective tissue layer and the pericranium). These main arteries of the scalp form the vascular plexus also in the loose connective tissue, and this vascular network connects with the perforator vessels from the network in the galea aponeurotica.
Table 4.1 Blood circulation morphology of the scalp
Artery | Origin | Distribution |
Supraorbital artery | Ophthalmic artery (a branch of the internal carotid artery) | Anterior part of the scalp |
Supratrochlear artery | Ophthalmic artery (a branch of the internal carotid artery) | Anterior part of the scalp |
Superficial temporal artery | External carotid artery | Lateral part of the scalp |
Posterior auricular artery | External carotid artery | Posterior part of the scalp |
Occipital artery | External carotid artery | Posterior part of the scalp |
The veins mainly run parallel with the arteries, flowing into the internal jugular vein via veins with the same names as the arteries, that is, the supratrochlear vein, supraorbital vein, superficial temporal vein, posterior auricular vein, and occipital vein. The supratrochlear and supraorbital veins flow into the internal jugular vein via the facial vein; however, some flow inside the orbit toward the intracranial cavernous sinus. Moreover, the superficial temporal vein is connected to the superior sagittal sinus in the cranial cavity via the emissary vein passing through the parietal foramen. This vein causes sustained bleeding from the parietal bone during subperiosteal dissection in the parietal region.
Surgical Annotation
Scalp Flap
This skin flap is the first considered in cases requiring various reconstructions of the soft tissue defect in the head. Although known as a skin flap, it is actually raised underneath the galea aponeurotica. Although it is often fundamentally used as a random pattern flap, it may also be used as an axial pattern flap, including the main arteries distributing the scalp, such as the superficial temporal artery.
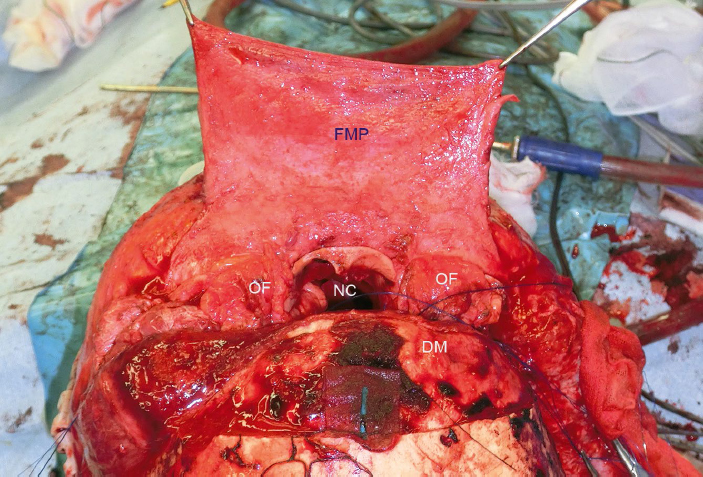
Frontal Musculopericranial Flap
The frontal musculopericranial flap is useful in the reconstruction of the anterior cranial base required after injury or tumor excision because it provides good blood circulation in addition to being strong but thin and flexible (Fig. 4.4). A periosteal flap in the frontal region is sometimes used for repairing anterior skull-base defects. When creating a large periosteal flap such as covering the entire anterior skull base, the blood circulation in the peripheral region of the flap often becomes unstable; then, in cases of large defects, the frontalis muscle flap should be raised with the periosteum.
Characteristics of the Layered Structures of Soft Tissue in the Temporal Region
The layered structures of the soft tissues in the temporal region is greatly different from the layered structures of other parts of the scalp. The following are the two main differences: (1) the temporalis muscle is in the deepest layer, and (2) the pericranium is not present underneath the temporalis muscle, and the pericranium of other parts of the head is continuous with the deep temporal fascia. From these differences, the layered structure of the temporal region is basically as follows, from the surface down: skin, subcutaneous tissue, superficial temporal fascia, subgaleal fascia (also called innominate fascia or loose areolar tissue layer), deep temporal fascia (divided into two layers inferiorly: the superficial layer and the deep layer), temporalis muscle, and subperiosteum (tissues below the pericranium).
The superficial temporal fascia is continuous with the galea aponeurotica layer in other parts of the head upward, in addition to being continuous with the SMAS in the face and continuous with the platysma in the neck.3,4 The superficial temporal fascia layer anatomically has the superior auricular muscle, temporoparietal muscle, and so forth, which are mimetic muscles in relation to the auricle; however, these muscles are difficult to appreciate during surgery and to recognize as the fascia of the superficial layer.
The subgaleal fascial layer consists of a loose connective tissue covering the entire calvarial region, as well as the temporal region, and it has a role of supporting the mobility of the scalp. Blood circulation of this layer is rich in the temporal region as a result of the abundant axial blood supply from the superficial temporal artery. Thin fat tissue is observed between the subgaleal fascia layer and the deep temporal fascia. Regarding the structure of the layers around the suprazygomatic arch region, Moss et al reported a fibrous partition called the inferior temporal septum, which is located along a line connecting the external acoustic meatus and temporal ligamentous adhesion (near the forefront edge of the temporal line and the lateral margin of the orbit) and connecting to the deep temporal fascia and superficial temporal fascia. In addition to reporting that there is a triangular fibrofatty compartment on the caudal side, they found that the temporal branch of the facial nerve runs directly underneath the superficial temporal fascia in this fat tissue in the temporal region above the zygomatic arch.7
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree