• Soft tissue evaluation is a crucial step in planning any aesthetic facial procedure.
• Patient assessment of all aging components and selection of procedures that address specific patient concerns are important.
• A combination of surgical and nonsurgical procedures for global soft tissue rejuvenation is common practice and improves the overall result.
• The surgeon should set up clear expectations regarding realistic results and explain to the patient the benefits and limitations of all the procedures that are proposed.
• Preoperative preparation includes thorough history and physical examination, photo analysis, anesthesia evaluation, and following a checklist.
• Postoperative care, routine pain and blood pressure control, and easy access to the nursing and surgical teams promote a smooth recovery and good patient satisfaction.
Introduction
The soft tissues of the face are a complex arrangement of skin, subcutaneous tissue, muscles, glands, and neurovascular structures connected in several places to the facial skeleton by connective tissue, septa, and ligaments. The smooth, rounded contour of a young face progressively changes with age as the tissues suffer structural alterations. Various predictable surface, volume, and ptotic changes take place. Dyschromia, rhytids, loss of skin elasticity, soft tissue deflation, and descent are the most common signs of aging that we encounter during the assessment of a patient seeking facial rejuvenation.
Understanding the anatomy of facial soft tissues is a prerequisite to understanding facial aging and its effects on the different structures. Knowledge of the anatomy and the subtle changes it suffers over time is essential in making sound decisions and planning of any facial rejuvenation procedure.
Patient evaluation
History
A comprehensive evaluation sheet is filled out by the patient during the initial consultation. The questionnaire includes present and past medical conditions, previous surgical history, prior cosmetic treatments, current medications, and history of smoking. Intrinsic and extrinsic aging factors, such as sun damage, dietary habits, and routine skin care regimen, are specific details key to the evaluation. Other issues that may interfere with the surgical planning are previous surgical and nonsurgical procedures, including injectables, peels, lasers, medications affecting bleeding, and previous history of deep vein thrombosis/pulmonary embolism (DVT/PE). It is our practice to go over the intake sheet and review it with the patient in detail. Some patients are instructed to bring pictures from their 20s for assessment of their facial features and of the individual facial aging process. It is important to understand the patient’s motivation for aesthetic surgery, emotional state, social life, and the support system available after surgery. Daily work and leisure activities can also be impacted by facial procedures, and some patients will not tolerate the postoperative downtime required by certain procedures and would prefer to choose minimally invasive facial rejuvenation options over surgeries that require a long period of downtime.
Differential diagnosis
The evaluation of the facial rejuvenation patient warrants assessment of the interconnections among the skin, fat compartments, muscle, and connective tissue. Skeletal asymmetries, previous facial trauma, severe sun damage, Romberg syndrome, xeroderma pigmentosum, cutis laxa, and Ehlers-Danlos syndrome can all contribute to facial aging and should be recognized and treated accordingly.
Physical examination
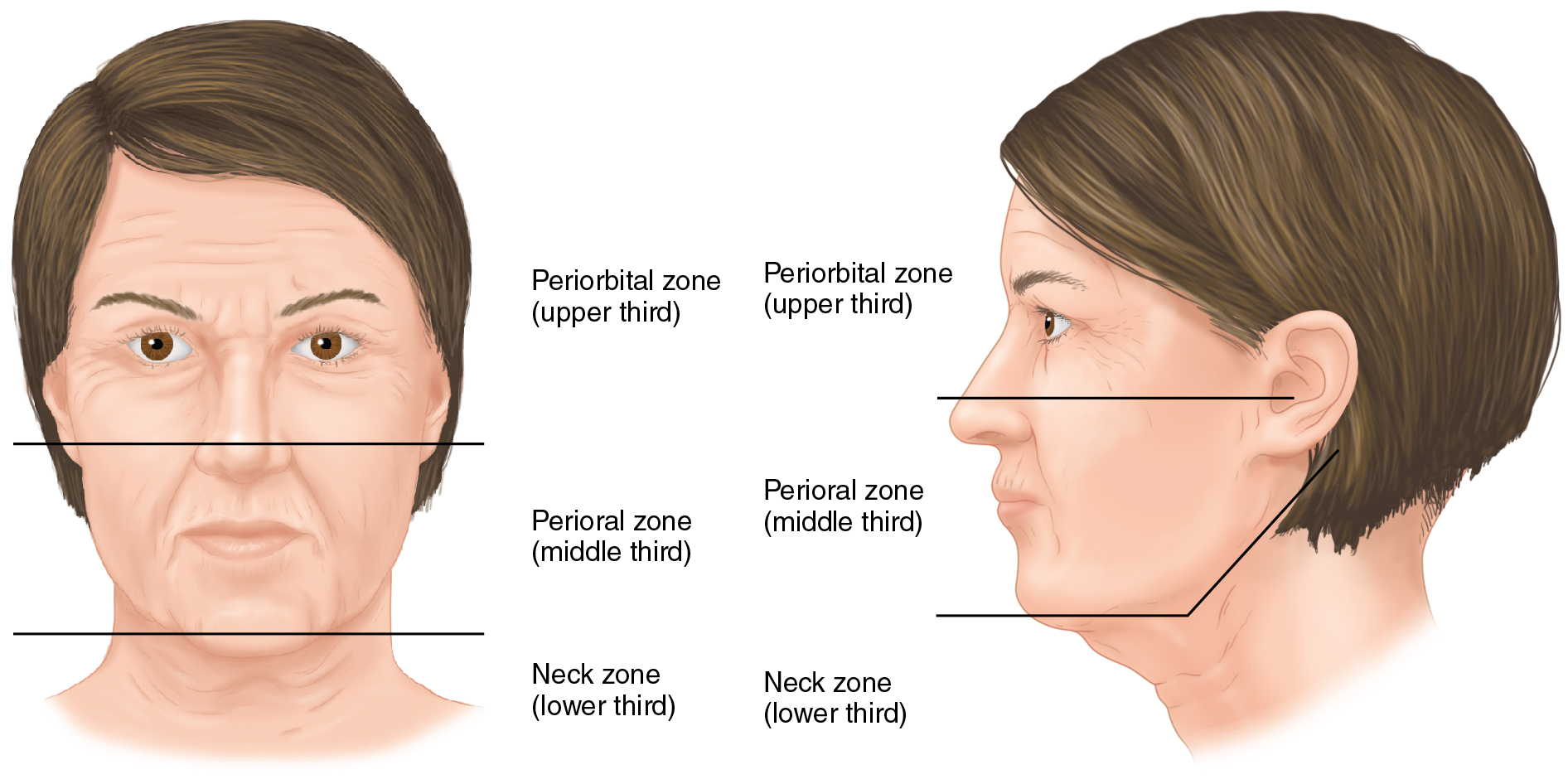
The evaluation begins with a visual assessment of the overall surface changes of the face. A systematic method of assessment includes evaluation of the face globally from top to bottom, dividing it into thirds. Starting from the hairline (trichion) to the chin (menton), or vice versa, can make the process objective and standard and facilitates communication and medical records. All the changes on the skin surface, facial volume, and positions of symmetrical facial structures are noted. The neck segment is considered the lower third in this facial analysis ( Fig. 34.1 ).
Starting with skin surface changes, the Fitzpatrick classification is a useful guide to define the skin type and plan procedures that will affect skin pigmentation. Dyschromias are a common concern in patients who seek facial rejuvenation, and the classification of the skin type will guide the choice of resurfacing procedures that could benefit the patient.
The next step is the evaluation of skin quality and elasticity, presence and degree of wrinkling, and whether the rhytids are dynamic or static. Assessment of volume loss and evidence of soft tissue atrophy in all segments of the face comes next and includes possible facial bone reabsorption and deflation of the superficial and deep fat compartments. The presence of folds and depressions at the level of the retaining ligaments of the face are consistent hallmarks of facial aging and can be predicted ( Fig. 34.2 ).
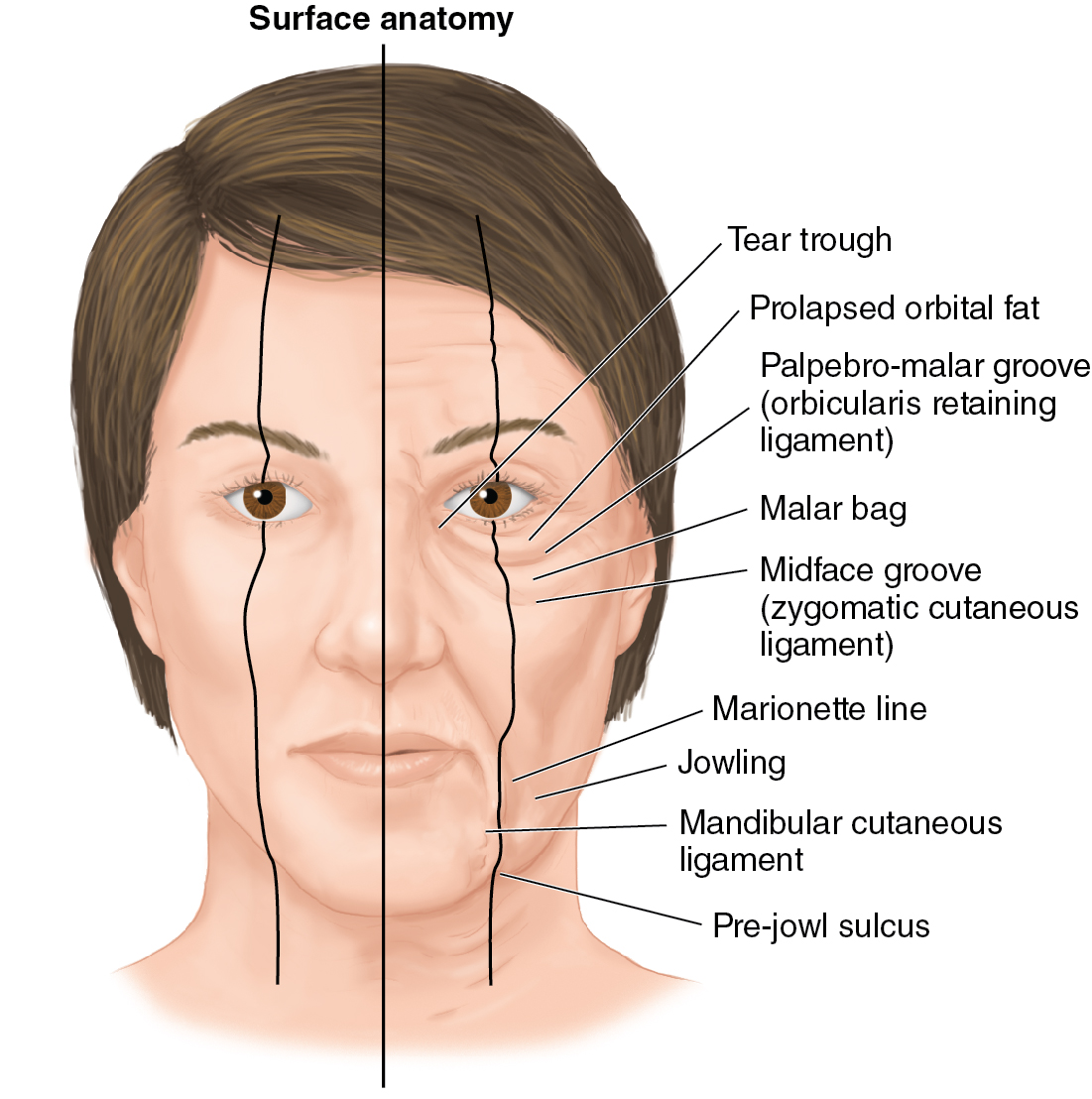
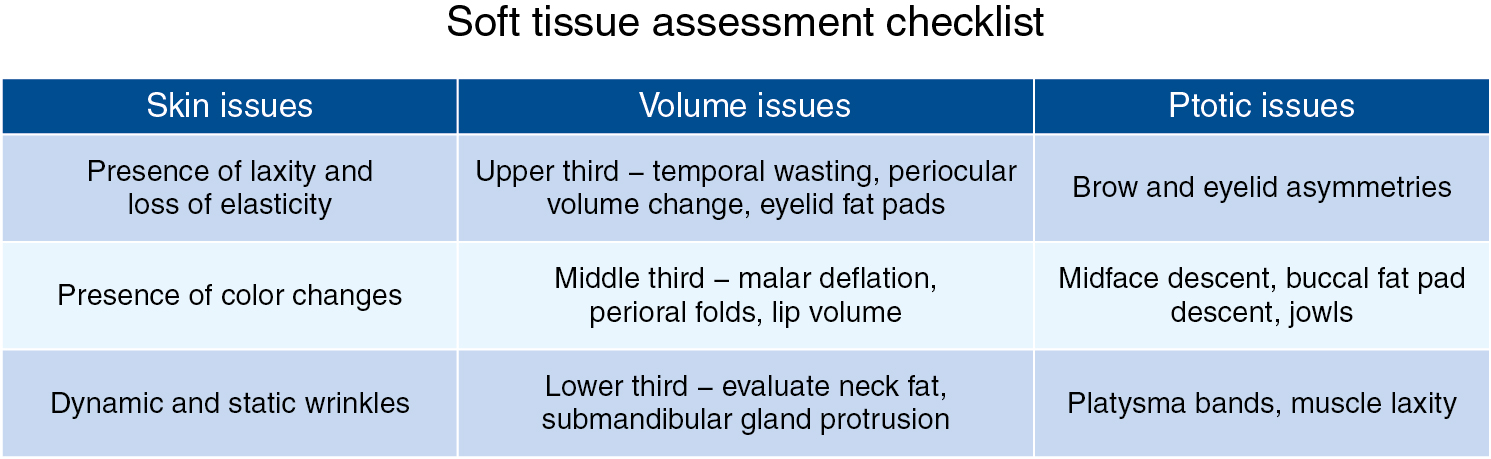
Presence of prominent submandibular glands and digastric muscles should be assessed routinely. Demarcation of the cheek–lid junction and blunting of the jaw line due to tissue deflation and descent are common findings in the aged face. Finally, we look for changes in the position of the structures, asymmetry of eyelid positioning, eyelid ptosis, lower eyelid vectors, smile asymmetries, aging nose, and neck deformities. This global volume and positioning assessment is fundamental to defining the need for “lift and fill” procedures, such as combining a facelift with fat grafting or simply tissue repositioning. Fig. 34.3 shows a soft tissue assessment checklist that is helpful in identifying the most common components of facial aging.
Imaging and other preoperative diagnostic evaluations
Preoperative evaluation is mostly performed through a thorough history and physical examination. Safety is an important part of planning an aesthetic procedure, and evidence-based medicine helps decide which preoperative tests are needed. If the patient has chronic medical issues the preoperative evaluation may include cardiac clearance, radiography, hematology consult, or an adjustment of current medication use. However, if the patient is healthy and younger than 50 years of age, there is no indication for any preoperative test, according to the American Society of Anesthesiology (ASA) preoperative evaluation guidelines.
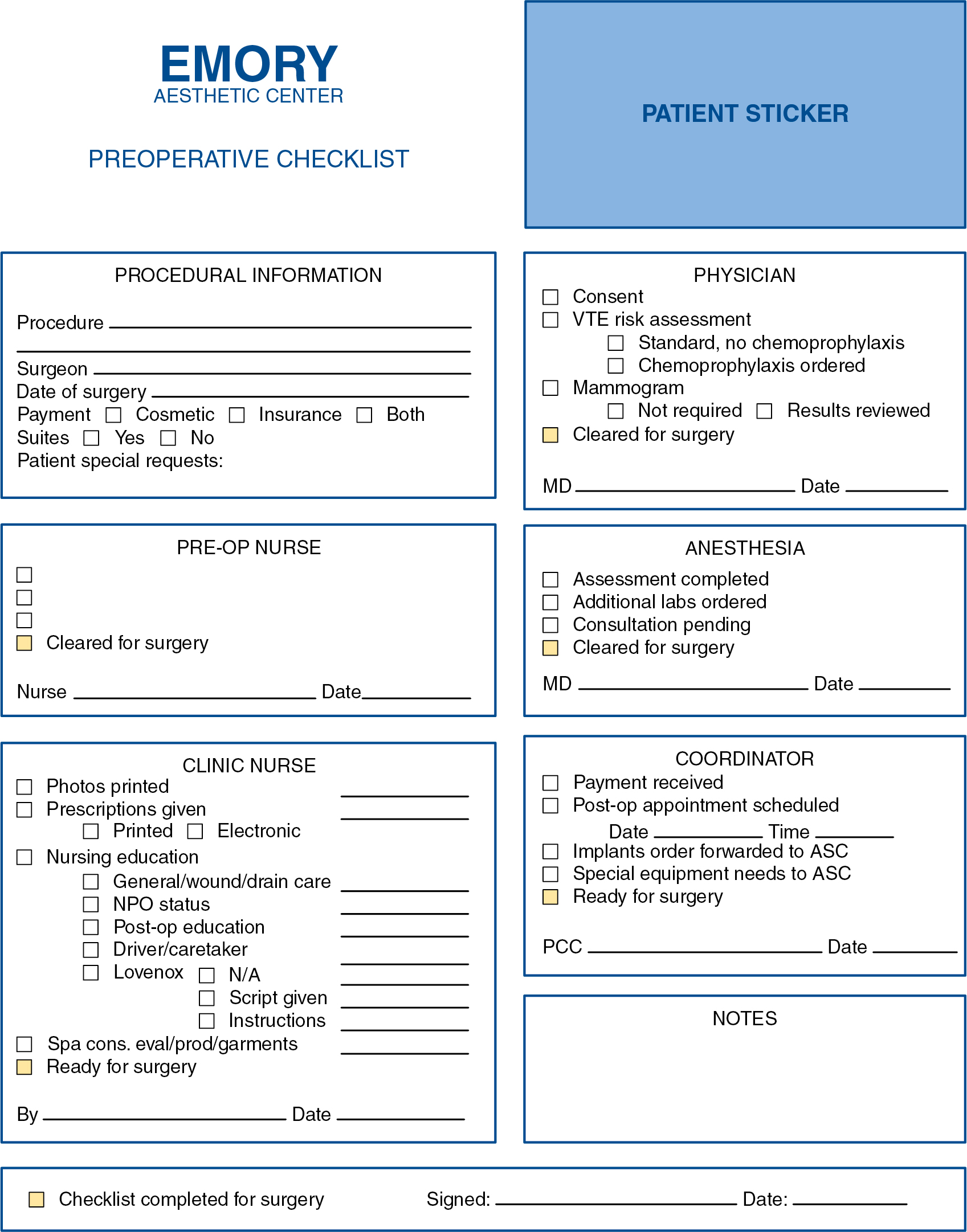
In our plastic surgery center all patients are scheduled for a formal preoperative visit with the surgeon, the nursing team, and the anesthesiologist 2 weeks before the procedure to review all the details of the surgical procedure, provide prescriptions, plan for medication discontinuation, perform the venous thromboembolism (VTE) risk assessment, evaluate the need for preoperative testing, address special equipment needs, confirm surgery payment, and any other preoperative requirements ( Fig. 34.4 ).
Indications/contraindications
Skin care
Skin care is an essential part of facial rejuvenation. It includes cosmeceuticals and topical prescriptions for home use. Tretinoin, topical vitamin C, daily sun screen, and a variety of skin moisturizers are routinely indicated for the majority of patients. A skin spa and experienced aestheticians are part of the team and help the patients select medical-grade products for individual needs, as well as noninvasive skin care procedures, such as superficial peels, nonablative laser treatments, and micro needling. We find that the presence of a skin care team on site is crucial for global patient treatment and satisfaction.
The use of botulinum toxin has become part of the skin treatment for wrinkles and fine lines. For patients presenting with dynamic wrinkles or dynamic as well as fine to moderate static wrinkles, botulinum toxin can be a great adjunct in improving and preventing skin aging.
Depending on the skin type, the characteristics of pigment changes, and skin wrinkling, we offer a different array of chemical peels and lasers. Freckles and sun spots can be treated with superficial exfoliating agents, such as retinoic acid peels, light trichloroacetic acid (TCA) peels, glycolic acid peels, or a combination of agents at low concentrations. For treatment of moderate to deep wrinkles, we prefer agents that penetrate the papillary and/or reticular dermis, such as TCA 30%, croton oil, erbium, and carbon dioxide (CO 2 ) lasers. Dermabrasion is also an option for the treatment of medium to deep wrinkles. The skin needs to be prepared before such treatment. We routinely use tretinoin 0.1% and hydroquinone 4% nightly for 2 to 4 weeks before the procedure to speed up healing and prevent postprocedure hyperpigmentation.
Volume change
Loss of facial volume is a common finding with facial aging. Fillers, such as hyaluronic acid, are a great tool for moderate volume enhancement on the cheeks, lips, and periocular area. They are noninvasive procedures performed in the office with minimal downtime. We use stiffer products with higher G prime for midface deflation and temporal hollowing and softer products for lip enhancement, nasolabial fold improvement, and periorbital volumization. We avoid the use of permanent synthetic fillers, although we are aware that they are available in the market.
Fat is an excellent autologous option when appropriately harvested, prepared, and grafted. We opt for microfat grafting techniques, as described by Coleman and Tonnard, for facial injections of fat. Microfat grafting for the midface, perioral, and periocular areas typically yields good results. Fat is a great material that blends nicely with the surrounding tissues when well used. It has a take rate of approximately 50%, so extra volume should be placed and taken into consideration, always avoiding bolus injections. Microfat grafting can be used intradermally (site-specific natural isotope fractionation [SNIF]) for improvement of perioral wrinkles, as described by Tonnard. We are currently exploring the use of nanofat grafting in the treatment of difficult issues, such as dark circles and facial lines.
The role of facial implants and aesthetic osteotomy for facial improvement has been well established for selected patients. We do not perform aesthetic osteotomy as a routine and opt for silicone chin implants in the case of microgenia and fat grafting or absorbable fillers for upper and midface volumization.
Ptotic changes
Facial tissue descent also occurs with age. It is debatable how much descent versus deflation contributes to the overall aged look, but it is wise to carefully evaluate faces on a case-by-case basis to determine whether there is a single factor or a combination of both factors, which is usually the case. , Descent due to tissue laxity causing caudal displacement of tissues, as in brow ptosis or jowls, is usually treated with surgery. Some noninvasive skin-tightening devices, based on ultrasound or radiofrequency technology, can be used in selected patients to treat tissue laxity and yield moderate results.
Facial asymmetry is a common finding. Mild asymmetries are not noticeable to most patients, but these should discussed as part of the decision-making process regarding surgical or nonsurgical procedures. Several strategies can be used to correct asymmetries, from muscle modulation with botulinum toxin to brow lift or facelift.
Preoperative planning
A formal preoperative consultation is scheduled 2 weeks before the date of surgery, at which time we address any questions that the patients might have and establish positive but realistic expectations for any procedure. We review the incision location, determine the expected recovery time, and schedule follow-up visits. This is a great opportunity to also review any patient concerns and strengthen the rapport with the patient. We reassess the amount of skin aging, volume deflation, descent, and asymmetries and design the preoperative planning according to the examination findings and the patient’s goals.
Photographic evaluation is a fundamental step of planning. It adds valuable information and captures skin changes, asymmetries, and volume distribution, and it is also a fundamental part of medical legal documentation. It is invaluable to have a dedicated photo room with consistent lighting and a system for routine patient positioning and image filing, as well as trained staff to capture comparable pre- and postoperative images. We also use a simulation system to help patients visualize the expected results after surgery. Standardized images are fundamental to accurate documentation and critical analysis of results. It is also important for the physician’s portfolio and marketing.
The decision regarding general versus local anesthesia is made in consultation with the anesthesia team. All patients are operated on in a certified, office-based surgical center that specializes in aesthetic surgery. , Most patients have ambulatory surgery and go home the same day, but for more extensive procedures and for patients’ convenience, we offer onsite suites with overnight nursing assistance.
Primary operative approach
- •
Skin resurfacing: Chemical peels, such as croton oil and TCA, are the preferred skin resurfacing agents for moderate to deep wrinkles. Fractionated CO 2 and erbium lasers are also good alternative resurfacing tools.
- •
Blepharoplasty: Upper blepharoplasty is performed with skin and muscle resection and conservative fat management. Eyelid ptosis is evaluated, and, if necessary, correction is offered at the same time as the blepharoplasty. Lower lid blepharoplasty is usually performed through a skin flap muscle dissection with fat removal or repositioning. Alternatively, transconjunctival fat removal along with skin pinch blepharoplasty is performed as needed for optimal results.
- •
Brow lift: This is often associated with upper blepharoplasty and performed either in the subperiosteal and subgaleal plane, depending on patient morphology and aging changes. Alternatively, brow lift or browpexy is performed through the upper lid.
- •
Midface lift: This procedure can be performed either through the lower lid or through the facelift incision. The use of fat grafting in the midface has improved the results of midface lift for patients with moderate to severe midface deflation.
- •
Facelift: Short scar facelifts are reserved for patients with mild to moderate lower face and neck laxity. For patients with moderate to severe jowls and neck aging, a full periauricular facelift incision is used. The decision about a superficial musculoaponeurotic system (SMAS) flap or SMAS plication depends on the tissue quality, tissue mobility, previous surgeries, and overall goals, but in about 80% of the patients, a SMAS flap is used for tissue suspension.
- •
Fat grafting: This can be performed by itself for isolated facial volumization or in association with surgery. Microfat grafting is the preferred technique and any area of deflation can be treated respecting proper technique. Nanofat grafting is also used in the more superficial planes.
Figs. 34.5 to 34.8 show preoperative and postoperative images of different patient presentations and different surgical approaches for customized results.